

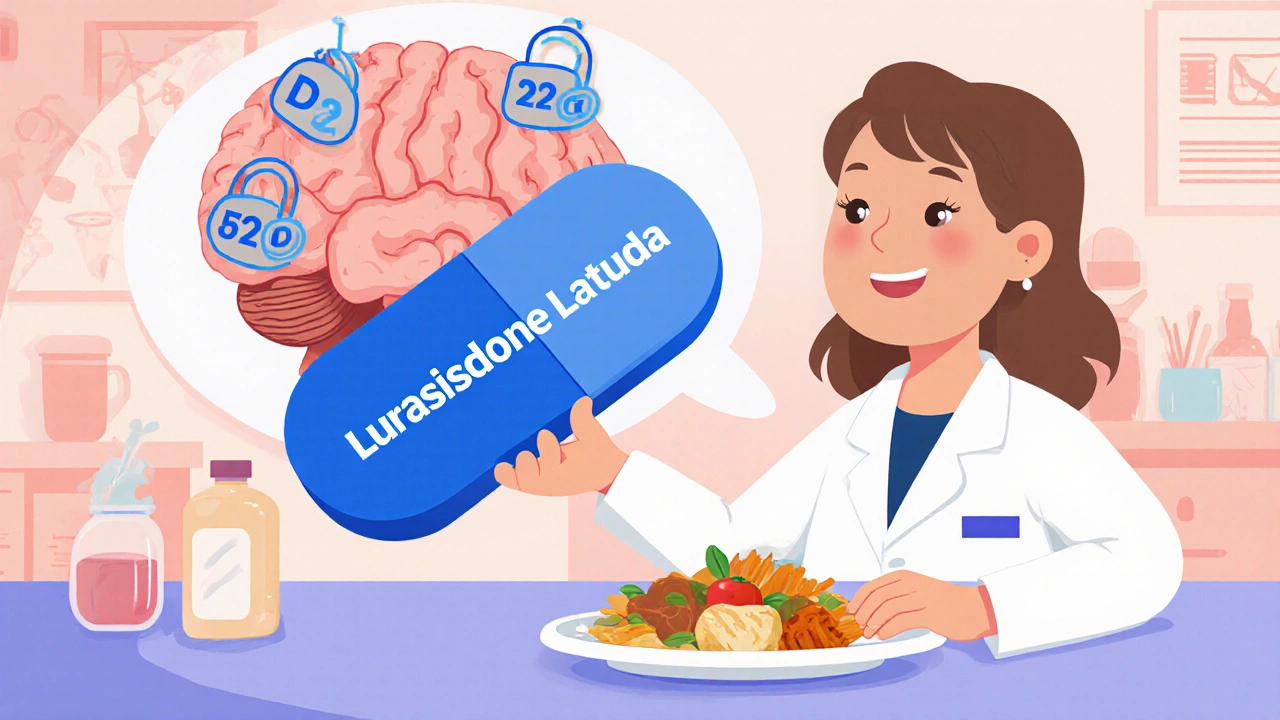
When you see the name Lurasidone, an atypical antipsychotic approved for schizophrenia and bipolar depression, Latuda you might wonder what makes it different from other mood‑stabilizing drugs. In plain terms, Lurasidone works by balancing dopamine and serotonin activity in the brain, which helps reduce hallucinations, mood swings, and other psychotic symptoms. If you're looking for detailed info on Lurasidone, you’ve landed in the right spot. The medication belongs to the class of atypical antipsychotics, a group known for fewer motor side effects compared to older drugs. It’s also prescribed for schizophrenia, a chronic mental health condition that often requires lifelong management. People with bipolar depression may receive Lurasidone as part of a broader treatment plan to stabilize mood and prevent depressive episodes. These connections form a clear picture: Lurasidone treats schizophrenia, Lurasidone helps bipolar depression, and Lurasidone is an atypical antipsychotic.
The practical side of Lurasidone matters just as much as the theory. Doctors usually start patients on a low dose and may increase it based on response and tolerance. Common side effects include nausea, sedation, and sometimes a temporary increase in blood sugar. Rare but serious risks involve movement disorders like akathisia, where patients feel an uncontrollable urge to move. Because side effects can dictate whether a patient sticks with the medication, clinicians compare Lurasidone to other atypical agents such as aripiprazole or quetiapine. This comparison often hinges on how each drug impacts weight, metabolic health, and the risk of extrapyramidal symptoms. For example, Lurasidone tends to cause less weight gain than many of its peers, making it a good option for patients concerned about obesity. The drug’s pharmacokinetic profile also means it should be taken with food; otherwise, absorption may be insufficient, reducing its effectiveness. Understanding these nuances helps patients and providers make informed choices and minimizes the chance of discontinuation.
Beyond effectiveness and safety, Lurasidone fits into a broader therapeutic ecosystem. For individuals with schizophrenia, long‑term antipsychotic therapy is essential to prevent relapse, and the medication’s once‑daily dosing can improve adherence. In bipolar depression, it is often combined with mood stabilizers like lithium or lamotrigine to cover the full spectrum of mood swings. Monitoring blood work periodically—especially fasting glucose and lipid panels—helps catch any metabolic shifts early. Lifestyle factors such as a balanced diet, regular exercise, and avoiding alcohol can also lessen side effects and boost overall outcomes. As research evolves, new data may highlight additional benefits or clarify rare risks, but the core principles remain: Lurasidone addresses dopamine and serotonin imbalance, it belongs to the atypical antipsychotic class, and it’s used for both schizophrenia and bipolar depression. Below you’ll find a curated set of articles that dive deeper into dosing strategies, side‑effect management, and how Lurasidone stacks up against alternative treatments.
A concise overview of the newest Lurasidone clinical trials, key results, safety data, and how it stands against other antipsychotics in 2025.