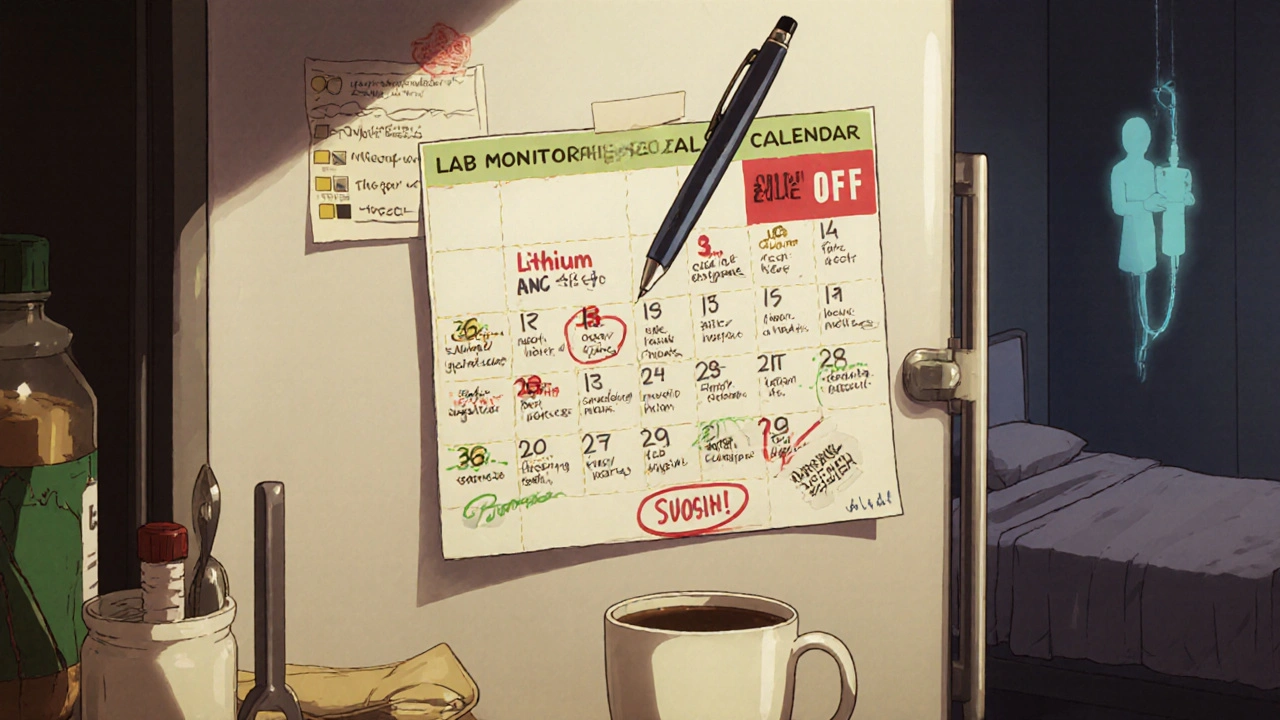
Medication Lab Monitoring Calendar Builder
Select Your Medication
Choose your medication from the list below to see its recommended monitoring schedule.
When you start a new medication, especially one with serious side effects, it’s not enough to just take it and hope for the best. Some drugs can quietly damage your liver, drop your white blood cell count, or throw your electrolytes out of balance - often before you feel anything wrong. That’s where a lab monitoring calendar comes in. It’s not a fancy gadget or a luxury. It’s your early warning system.
Why Your Doctor Isn’t Always Watching
Doctors don’t sit there watching your blood work 24/7. They rely on you to show up for tests. But between busy schedules, missed appointments, and the fact that many side effects don’t show up until damage is already done, it’s easy for things to slip through. A lab monitoring calendar fixes that. It turns guesswork into a clear schedule: When you need a blood test, what they’re checking, and why it matters.Take clozapine, an antipsychotic used for treatment-resistant schizophrenia. It can cause a dangerous drop in white blood cells - a condition called agranulocytosis. If unchecked, this can lead to life-threatening infections. The rule? Weekly blood tests for the first 18 weeks, then every two weeks, then monthly. Miss one test, and you could be putting your life at risk. A printed or digital calendar with these dates marked clearly keeps you on track.
Medications That Need a Lab Calendar (And What to Track)
Not every drug needs this level of oversight. But for these common ones, skipping lab checks is a gamble you shouldn’t take:- Lithium (for bipolar disorder): Blood levels must be checked 5-7 days after starting, then weekly until stable. After that, every 6 months. Too high? You get tremors, confusion, even seizures. Too low? Your mood swings come back. The timing matters - tests must be done 12 hours after your last dose.
- Warfarin (blood thinner): INR levels need checking monthly. More often if your dose changes, you start a new antibiotic, or you change your diet. An INR too high means you could bleed internally. Too low, and you’re at risk for stroke.
- Corticosteroids (like prednisone): If you take them for more than two weeks straight, your adrenal glands can shut down. A morning cortisol test before stopping the drug is critical to avoid adrenal crisis - a medical emergency.
- LONSURF (for advanced colon cancer): This chemo drug lowers blood counts fast. Weekly CBCs (complete blood count) are required. If your platelets or neutrophils drop too low, your next dose is delayed. Missing a test means you might get a dangerous dose when your body can’t handle it.
- Mirtazapine (antidepressant): Less intense, but still needs monitoring. Weekly weight and appetite checks for the first 4-8 weeks. Weight gain is common, and catching it early helps manage it.
- Dorzolamide/Timolol (glaucoma eye drops): Annual eye exams are required to check for damage to the optic nerve. Side effects like blurred vision or eye pain? Don’t wait - get checked.
Digital vs. Paper: Which Works Better?
You’ve got options. But not all are created equal.Printable calendars (like those from Community Behavioral Health or CBH Philly) are simple. You can tape them to your fridge. You can mark off tests with a pen. They’re reliable - no battery, no app update, no glitch. But they don’t remind you. You have to remember to check them.
Digital tools like Blood Cancer United’s Health Manager app do more. They let you log symptoms - nausea, dizziness, fatigue - and tie them to your medication timing. Did you feel dizzy after eating? Did your headache start after skipping breakfast? The app finds patterns you’d miss. It syncs with your calendar, sends alerts, and lets you share reports with your doctor in one click.
Ulta Lab Tests lets you order your own blood work, which sounds great - until you realize they don’t tell you when to test or what to look for. You still need a calendar to know the schedule. Don’t skip the scheduling part.
How to Build Your Own Lab Monitoring Calendar
Start with your prescription. Then follow these steps:- Ask your doctor or pharmacist: “What labs do I need, how often, and why?” Write down the exact tests - don’t rely on memory.
- Find the timing rules: Some tests need to be done before breakfast. Others need to be 12 hours after your last dose. Note those details.
- Choose your format: Use a printable PDF, a Google Calendar, or an app like Health Manager. Pick one you’ll actually use.
- Set reminders: Schedule alerts for 3 days before each test. Include the time of day and any prep rules (fasting, no caffeine, etc.).
- Track symptoms: Every time you get a lab test, write down how you’ve been feeling. Did you have more fatigue? Worse nausea? That data helps your doctor adjust your treatment.
- Bring it to every appointment: Even if your doctor has your chart, they might not have looked at your calendar. Hand them your printed sheet or open your app. Say, “Here’s what I’ve tracked.”
What Happens When You Skip a Test
It’s not just about getting a bad result. It’s about missing the chance to stop something before it gets worse.Warfarin users who skip INR checks are 3 times more likely to have a major bleed. Lithium patients who go 12 months without a level check are at high risk for kidney damage or neurological toxicity. Clozapine patients who miss ANC tests can develop sepsis within days.
These aren’t hypotheticals. They’re documented cases. A 2025 study from Community Behavioral Health showed that patients who used a structured lab calendar had 68% fewer hospitalizations due to drug side effects compared to those who didn’t.
When the Schedule Changes
Your calendar isn’t set in stone. If your dose changes, you start a new drug, or you get sick, your monitoring needs might change too.For example, if your clozapine dose is lowered and your ANC stays above 1500 for three months straight, your doctor might reduce testing from weekly to monthly. But don’t assume - ask. Update your calendar immediately. And if you’re unsure, keep testing until you get clear instructions.
Same goes for corticosteroids. If you’re tapering off, you might need a cortisol test before stopping completely. Skip that, and you could collapse from adrenal failure.
Real-Life Example: Sarah’s Story
Sarah, 58, started lithium for bipolar disorder. Her doctor gave her a printout with a list of tests. She forgot about it. Three months later, she felt foggy, her hands shook, and she vomited. She went to the ER. Her lithium level was 2.1 - toxic. Normal is 0.6-1.2. She spent five days in the hospital. Her kidneys were damaged.After that, she started using a digital calendar app. She set reminders, logged her mood, and tracked her water intake (dehydration raises lithium levels). Now, she’s been stable for 14 months. No hospital visits. No side effects.

What’s Next? AI and Wearables
The future is coming. Some apps are starting to use AI to predict when your lab values might go off track - based on your past results, diet, sleep, and even weather. Wearables that track heart rate variability might soon hint at early signs of inflammation or stress from medication side effects.But right now, the best tool is still the one you use consistently: a simple calendar with clear dates, clear tests, and clear rules. No AI can replace you showing up for your blood test on time.
Final Rule: Don’t Guess. Track.
Medications save lives. But they can also hurt you - silently. A lab monitoring calendar isn’t about being paranoid. It’s about being smart. It’s about taking control before something goes wrong.Write it down. Set the alarms. Bring it to your next appointment. You’re not just taking a pill. You’re managing a process. And that process needs a plan.
Do I need a lab monitoring calendar for every medication?
No. Only medications with known risks that require blood tests or clinical monitoring need one. Common examples include lithium, warfarin, clozapine, corticosteroids, and certain cancer drugs. If your doctor says, "We’ll check your blood in a few weeks," that’s your cue to start tracking.
Can I just rely on my doctor to remind me?
No. Doctors have hundreds of patients. They won’t remember your specific schedule. Even if they send a reminder, it might get lost in a flood of emails or texts. Your calendar is your responsibility - and your safety net.
What if I miss a lab test?
Don’t panic. Call your doctor or pharmacist right away. They’ll tell you whether to reschedule, skip the next dose, or come in for an urgent check. Never guess. Missing one test doesn’t mean you’ve failed - it means you need to get back on track.
Can I order my own blood tests without a doctor’s order?
Yes, through services like Ulta Lab Tests. But ordering alone isn’t enough. You still need to know which tests to order, when to take them, and what the results mean. Without guidance, you might test too early, too late, or the wrong thing. Always confirm your schedule with your provider.
How long do I need to keep using the calendar?
As long as you’re taking the medication - and sometimes longer. Clozapine requires lifelong ANC monitoring. Lithium often needs checks every 6 months even after years of stability. Stopping the calendar too soon is a common mistake. Always ask your doctor when, or if, you can stop.
Can I use a regular calendar app like Google Calendar?
Yes - and it’s a good idea. Set recurring events with clear labels: "Lithium Level Check - 8 AM - Fast", "INR Test - Monthly", "ANC Blood Draw - Weekly". Add notes about prep rules. You can even attach PDFs of your calendar or lab instructions to the event.
Why does timing matter so much for lithium tests?
Lithium levels change based on when you last took your dose. Testing too soon after taking it gives a falsely high reading. Testing too late gives a falsely low one. The standard is 12 hours after your last dose - that’s when your blood level is stable and reflects your true dose. Always note the time you took your pill and schedule the test accordingly.
Are there free printable lab calendars I can use?
Yes. Community Behavioral Health (CBH), Taiho Oncology (for LONSURF), and the NIH offer free, condition-specific templates. Search for "[medication name] lab monitoring calendar PDF" - you’ll find them. Print one and keep it where you’ll see it every day.
Next Steps: What to Do Today
1. Look at your current prescriptions. Which ones require lab monitoring?2. Call your pharmacy or doctor’s office. Ask for the official monitoring schedule.
3. Pick one tool - paper, Google Calendar, or Health Manager - and set up your first three test reminders.
4. Write down one symptom you’ve noticed lately. Track it alongside your next lab test.
5. Bring your calendar to your next appointment. Say, "I’ve been tracking this - here’s what I’ve seen."
Your health isn’t something you wait for. It’s something you manage - one test, one date, one day at a time.









Comments (10)
Reema Al-Zaheri
November 19, 2025 AT 04:51 AMThere's a critical omission here: the lack of standardized, interoperable formats for lab monitoring calendars across healthcare systems. If your doctor uses Epic, your pharmacist uses Cerner, and your app uses Apple Health, none of them talk to each other. You end up maintaining three separate calendars, each with slight discrepancies. This isn't just inconvenient-it's a systemic failure in care coordination. The solution isn't better apps; it's mandatory FHIR-based interoperability for all prescription monitoring data.
Angela Gutschwager
November 20, 2025 AT 03:00 AMUgh. I just want my pill and a Netflix binge.
Andy Feltus
November 20, 2025 AT 11:47 AMSo we're treating patients like lab rats with a spreadsheet? How noble. We've reduced human physiology to a checklist of blood draws, as if the body is a car that needs a tune-up every 3,000 miles. The real tragedy isn't that people forget tests-it's that we've built a system where compliance is the only thing keeping you alive, and the system itself never takes responsibility. We don't need calendars. We need better drugs.
Steve and Charlie Maidment
November 20, 2025 AT 13:50 PMLook, I get it. You're trying to be helpful. But let's be real-most people can't even remember to refill their prescriptions, let alone track 12 different blood tests with exact timing windows. And don't get me started on the fact that these calendars assume you have reliable internet, a smartphone, a printer, transportation to a lab, and the mental bandwidth to manage this while juggling work, kids, and chronic pain. This isn't empowerment-it's privilege wrapped in a PDF. The real problem is that we're asking people with limited resources to fix a system that's broken by design. And no, telling them to "just use Google Calendar" isn't a solution. It's a joke.
Chuck Coffer
November 22, 2025 AT 13:37 PMInteresting. So you're telling me the solution to pharmaceutical toxicity is... more paperwork? Brilliant. Next you'll suggest we install mandatory breathalyzer tests before taking Tylenol. At what point do we stop outsourcing our biology to spreadsheets and start demanding safer medications? Or is the industry just fine with us becoming full-time lab technicians?
Marjorie Antoniou
November 22, 2025 AT 14:27 PMI'm a nurse, and I've seen what happens when people skip tests-not because they're careless, but because they're overwhelmed. This post is vital. But the real win isn't the calendar-it's when someone says, "I brought my tracker," and the doctor actually looks at it. That moment changes everything. If you're reading this and you're scared, you're not alone. Start small. One test. One reminder. One conversation with your provider. You're not failing. You're learning.
Andrew Baggley
November 23, 2025 AT 23:45 PMThis is the kind of post that gives me hope. Seriously. Most people think medication is just swallowing a pill and hoping for the best. But you? You're treating your body like the complex, beautiful machine it is. That mindset? That’s the real medicine. Whether you use paper, Google Calendar, or a sticky note on your mirror-just do it. Your future self will thank you. And if you miss a test? No guilt. Just reset and keep going. Progress, not perfection.
Frank Dahlmeyer
November 24, 2025 AT 04:12 AMLet me tell you something-when I was on warfarin after my pulmonary embolism, I had a laminated calendar taped to my fridge with color-coded markers for INR days, dietary restrictions, and even the name of the lab technician who always gave me extra gummy bears. I didn't just track my blood-I tracked my life. And when I missed one test because I was traveling and the lab was closed? I called my anticoagulation clinic at 6 a.m., explained the situation, and they gave me a same-day appointment at a different location. That’s the power of being proactive. Don’t wait for the system to catch you-be the one who shows up. You’re not a patient. You’re a partner. And partners don’t ghost their own health.
Codie Wagers
November 25, 2025 AT 21:37 PMHow convenient. A blog post that makes patients responsible for the failures of pharmaceutical oversight, clinical negligence, and fragmented healthcare infrastructure. You’ve turned a systemic crisis into a productivity hack. Brilliant. Tell me-when the next drug causes irreversible liver damage because the monitoring schedule was wrong, who gets sued? You? The calendar? Or the company that never bothered to develop a safer alternative? This isn’t empowerment. It’s gaslighting disguised as advice.
Paige Lund
November 26, 2025 AT 03:31 AMYeah, I’ll just add another thing to my 17 daily reminders.