

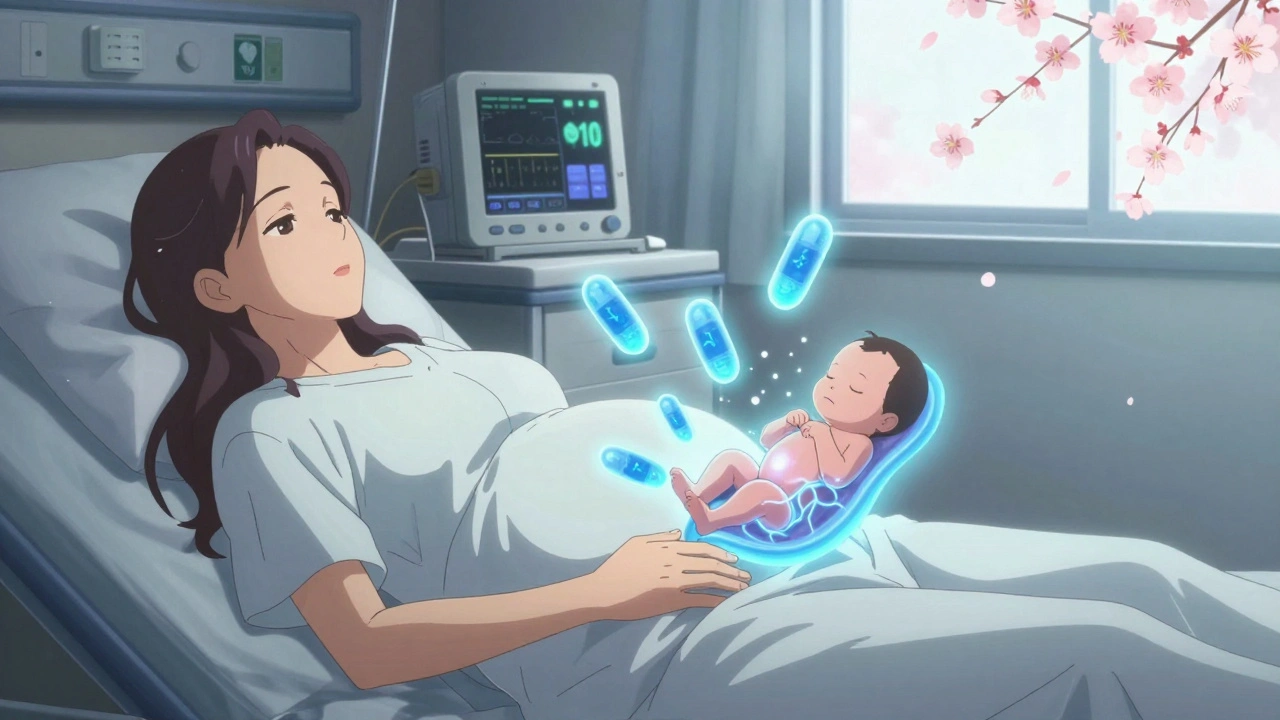
When a baby is born after being exposed to certain medications or drugs in the womb, they can go through neonatal withdrawal, a condition where the newborn’s body reacts to the sudden absence of substances it became dependent on during pregnancy. Also known as neonatal abstinence syndrome, it’s not rare—thousands of infants in the U.S. experience it each year, mostly from opioid exposure. This isn’t about bad parenting. It’s about how the developing nervous system adapts to drugs like methadone, buprenorphine, oxycodone, or even some antidepressants—and then struggles when those drugs are cut off at birth.
Neonatal abstinence syndrome, the clinical term for drug withdrawal in newborns shows up in predictable ways: excessive crying, tremors, tight muscles, poor feeding, fast breathing, and trouble sleeping. These symptoms aren’t just uncomfortable—they can lead to weight loss, dehydration, and longer hospital stays. The severity depends on the drug, how much and how often the mother took it, whether she used multiple substances, and even the baby’s genetics. Some babies show signs within 24 hours; others don’t react until a week after birth. That delay is why doctors watch newborns closely for at least 72 hours if there’s any known exposure.
What helps? Non-pharmacological care, a gentle, low-stimulus approach that includes swaddling, skin-to-skin contact, quiet rooms, and frequent feeding works for many babies. For others, medicine like morphine or methadone is needed to ease symptoms slowly, then tapered down. The goal isn’t to eliminate all discomfort—it’s to avoid complications and give the baby time to rewire their nervous system. Studies show that babies who get consistent, calm care from their parents recover faster and leave the hospital sooner.
And here’s the thing: neonatal withdrawal isn’t just about opioids. It can happen with SSRIs, benzodiazepines, or even heavy caffeine use. That’s why doctors now ask detailed questions about every medication, supplement, or substance a pregnant person takes—not to judge, but to prepare. If you’re expecting and taking any of these, talk to your provider early. There are safer options, and planning ahead makes a huge difference.
The good news? Most babies with neonatal withdrawal grow up just fine. With the right care, they catch up on growth and development. But the journey starts with recognizing the signs, knowing what to expect, and having a team ready to help. Below, you’ll find real guides from doctors, pharmacists, and parents who’ve been through it—covering everything from what medications trigger withdrawal to how to support a baby at home after discharge.
Opioid use during pregnancy requires careful medical management. Learn the risks of withdrawal, how MAT with methadone or buprenorphine helps, what to expect with neonatal withdrawal, and why breastfeeding is often safe.