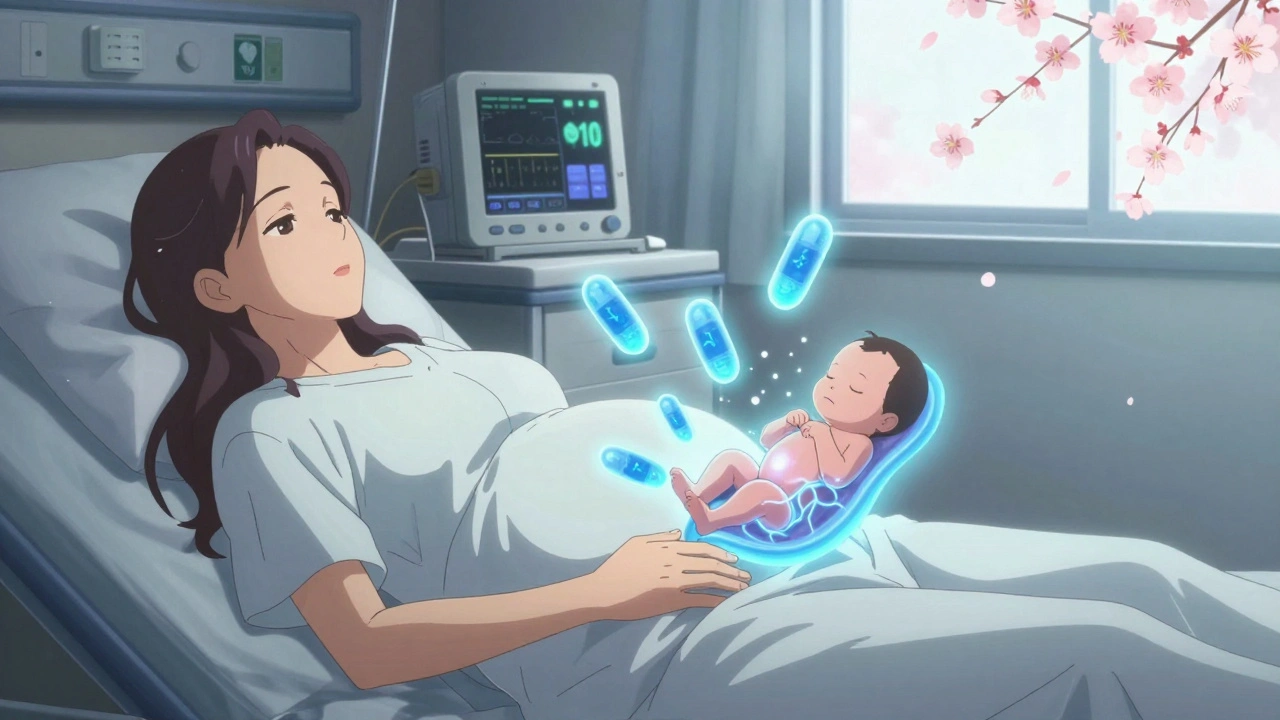
When a pregnant person is using opioids, whether prescribed or not, the stakes aren’t just about their own health-they’re about the life growing inside them. Opioid use disorder (OUD) during pregnancy isn’t rare. Between 2010 and 2020, cases of neonatal opioid withdrawal syndrome (NOWS), formerly called NAS, increased fivefold in U.S. hospitals. That’s not just a statistic. It’s a wave of babies born with trembling hands, high-pitched cries, and trouble eating-each one needing care that’s more complex than most new parents expect.
What Happens When Opioids Cross the Placenta
Opioids don’t stay in the mother’s bloodstream. They cross the placenta easily, reaching the baby’s developing brain and nervous system. That’s why babies exposed to opioids before birth often go into withdrawal after birth. It’s not because the mother did something wrong-it’s because the baby’s body has adapted to the drug’s presence and now has to adjust without it.The symptoms of neonatal opioid withdrawal syndrome (NOWS) can show up as early as 48 hours after delivery. Common signs include:
- High-pitched, persistent crying
- Shaking or twitching limbs
- Feeding problems-difficulty latching, vomiting, poor weight gain
- Fast breathing (over 60 breaths per minute)
- Temperature changes-either too high or too low
- Loose, watery stools (more than three per hour)
These symptoms aren’t just uncomfortable-they can be dangerous. About 50% to 80% of babies exposed to opioids during pregnancy will need medical help for withdrawal. That’s why monitoring starts the moment the baby is born.
Why Withdrawal Isn’t the Answer
Many people assume the best thing to do is stop opioids during pregnancy. But stopping suddenly-called medically supervised withdrawal-isn’t safer. In fact, it’s riskier.The CDC says that pregnant people who try to quit opioids cold turkey face a 30% to 40% higher chance of relapse. That means they’re more likely to use again, often at higher doses, which puts the baby at even greater risk. Withdrawal also increases the chances of:
- Preterm labor (25-30% vs. 15-20% with treatment)
- Fetal distress (18-22% vs. 8-12% with treatment)
- Miscarriage (5-8% vs. 2-4% with treatment)
Instead of quitting, the standard of care is medication-assisted treatment (MAT). That means using FDA-approved medications like methadone or buprenorphine to keep the mother stable-without the highs and lows of street drugs or misuse.
Methadone vs. Buprenorphine: What’s the Difference?
Not all MAT is the same. Two medications are most commonly used: methadone and buprenorphine. Both are safe during pregnancy, but they have different effects.Methadone is a full opioid agonist. It’s been used for decades in pregnancy. Dosing usually starts at 10-20 mg per day and can go up to 60-120 mg, depending on the person’s needs. It has high retention rates-70% to 80% of people stay in treatment after six months. But babies born to mothers on methadone often have more severe withdrawal symptoms. On average, their hospital stays are longer-about 17.6 days-and their Finnegan scores (a tool doctors use to measure withdrawal severity) are higher, averaging 14.3.
Buprenorphine is a partial opioid agonist. It’s newer in pregnancy care but widely recommended now. Starting doses are lower-2-4 mg daily-and can go up to 8-24 mg. It’s easier to manage, often given as a sublingual film. Babies exposed to buprenorphine have less severe withdrawal than those exposed to methadone. Their average Finnegan score is 11.8, and hospital stays are shorter-around 12.3 days. But here’s the catch: 46% of these babies still need medication to treat withdrawal.
One study from Boston Medical Center found that infants exposed to naltrexone-a medication that blocks opioids-had zero cases of withdrawal. That sounds perfect, right? But naltrexone isn’t used for everyone. The mothers in that study got into treatment much later-on average at 28.4 weeks-compared to 19.7 weeks for those on buprenorphine. Delayed care means higher risk for the baby. So while naltrexone looks promising, it’s not a first-line option unless the person is already stable and far along.

How Babies Are Monitored After Birth
Every baby born to a mother with OUD needs careful monitoring. The CDC recommends at least 72 hours of observation, with checks every 3-4 hours in the first day, then every 4-6 hours after that.Most hospitals use the Finnegan scale-a checklist that scores symptoms like crying, tremors, sleep, and feeding. But not all hospitals use the same tool. One study found 37 different scoring systems in use across U.S. hospitals. That’s confusing for families and inconsistent for care.
More hospitals are switching to the Eat, Sleep, Console method. Instead of focusing only on symptoms, this approach asks: Can the baby eat? Can they sleep? Can they be comforted? If the answer is yes to all three, they might not need medicine-even if their Finnegan score is high. Hospitals using this method report 30-40% fewer babies needing opioid treatment for withdrawal.
Can You Breastfeed While on Opioid Treatment?
Yes-most of the time. Breastfeeding is encouraged for mothers on methadone or buprenorphine. The amount of medication that passes into breast milk is very low and doesn’t usually cause problems. In fact, breastfeeding can help reduce the severity of withdrawal symptoms in babies.One study showed that 83% of mothers on naltrexone were able to breastfeed without issues. For those on buprenorphine, breastfeeding rates are high too, but some babies still need extra monitoring. The American Academy of Pediatrics says breastfeeding is safe for most infants on MAT unless the mother is using other substances or has HIV.
Still, many moms report stigma. One mother on a recovery forum said her nurse told her, “You shouldn’t be nursing-you’re still using drugs.” That kind of comment isn’t just hurtful-it’s wrong. MAT isn’t “using.” It’s treatment.

What About New Treatments?
In 2023, the FDA approved a new long-acting form of buprenorphine called Brixadi. It’s given as a monthly injection instead of daily pills or films. In early trials, 89% of pregnant women stayed in treatment for 24 weeks-compared to 76% with daily buprenorphine. That’s a big win. Keeping people in treatment longer means better outcomes for both mom and baby.Another promising shift is in how we treat withdrawal. The American Academy of Pediatrics now says: Try non-drug care first. Hold the baby skin-to-skin. Rock them. Feed them often. Dim the lights. These simple things can calm a baby’s nervous system. Only if those don’t work should doctors consider medication like morphine or methadone for the baby.
The Bigger Picture: Why This Isn’t Just About Medicine
Treating OUD during pregnancy isn’t just about pills and monitoring. It’s about access. In 2021, only 45% of U.S. hospitals had a standard protocol for managing OUD in pregnancy. In rural areas, that number drops to 28%. Many women don’t get care until late in pregnancy-sometimes not until they’re in labor.And it’s not just about drugs. Nearly half of pregnant women with OUD face housing instability. More than 30% have moderate to severe depression. Over 40% report postpartum depression. Without mental health support, housing help, and trauma-informed care, even the best medication won’t work.
Programs that tie together prenatal care, MAT, therapy, and housing assistance are showing results. One NIH-funded study found that when all these pieces are connected, NAS severity drops by 22%. That’s not magic. That’s good care.
What You Need to Know If You’re Pregnant and Using Opioids
If you’re pregnant and using opioids-whether prescribed, misused, or taken recreationally-here’s what matters most:- Don’t stop cold turkey. It’s dangerous for you and your baby.
- Ask for MAT. Methadone or buprenorphine are the safest options.
- Start care as early as possible. First trimester is ideal.
- Expect your baby to be monitored after birth. It’s normal, not a failure.
- Breastfeeding is usually safe and helpful.
- Ask for help with mental health, housing, and childcare. You don’t have to do this alone.
Recovery isn’t about perfection. It’s about progress. Every day you stay in treatment, you’re giving your baby a better chance.
Is it safe to take buprenorphine while pregnant?
Yes. Buprenorphine is one of the two recommended medications for opioid use disorder during pregnancy, alongside methadone. It’s been studied extensively and is considered safe for both mother and baby. It helps reduce cravings and withdrawal, lowers the risk of relapse, and improves outcomes like birth weight and gestational age. Babies born to mothers on buprenorphine often have less severe withdrawal than those exposed to methadone or street opioids.
Can opioid use during pregnancy cause birth defects?
There’s no strong evidence that opioids like methadone or buprenorphine cause major birth defects. The biggest risks are preterm birth, low birth weight, and neonatal withdrawal-not physical malformations. That’s why treatment is so important. Staying on MAT reduces those risks significantly compared to using street drugs or stopping abruptly.
How long does neonatal withdrawal last?
Withdrawal symptoms usually start 48 to 72 hours after birth and can last from a few days to several weeks. For babies on medication, treatment can take 10 to 21 days, depending on severity. Some babies with milder symptoms may only need supportive care-skin-to-skin contact, feeding on demand, and quiet environments-and won’t need drugs at all. Long-term follow-up shows most babies catch up developmentally by age 2.
Can I breastfeed if I’m on methadone or buprenorphine?
Yes. Both methadone and buprenorphine are considered safe for breastfeeding. Only tiny amounts pass into breast milk, and studies show no negative effects on infant development. In fact, breastfeeding can help reduce the severity of withdrawal symptoms in babies. The American Academy of Pediatrics supports breastfeeding for mothers on MAT unless they’re using other substances or have HIV.
What if I used opioids before I knew I was pregnant?
It’s never too late to get help. Even if you used opioids early in pregnancy, starting treatment as soon as possible improves outcomes. The goal isn’t to judge past choices-it’s to protect the baby moving forward. Many women start MAT in the second or third trimester and still have healthy babies. What matters now is getting connected to care.
Is naltrexone safe during pregnancy?
Naltrexone is not currently recommended as a first-line treatment during pregnancy. While one study showed no withdrawal symptoms in newborns, most mothers in that study entered treatment later in pregnancy-around 28 weeks-which increases risks. Naltrexone blocks opioids completely, so if a person relapses, they could experience severe withdrawal or overdose. It’s being studied further, but methadone and buprenorphine remain the gold standard.
Where can I find help if I’m pregnant and struggling with opioids?
Start with your OB-GYN or midwife. They can refer you to a specialist in addiction medicine. Many hospitals now have integrated care teams that include obstetricians, addiction counselors, and social workers. You can also call SAMHSA’s National Helpline at 1-800-662-HELP (4357)-it’s free, confidential, and available 24/7. Medicaid covers MAT for pregnant women in most states thanks to the 2020 SUPPORT Act.







Comments (13)
Chris Marel
December 9, 2025 AT 12:40 PMThis post really hit home. I’ve seen friends go through this and no one talks about how scary it is to even ask for help. The fact that withdrawal is riskier than staying on MAT? That’s not common knowledge. I wish more OBs knew this.
Evelyn Pastrana
December 11, 2025 AT 01:23 AMSo let me get this straight - we’re telling moms they can’t quit cold turkey, but it’s totally fine to keep giving them drugs? 😏 Guess the ‘war on drugs’ got a pregnancy exemption. Also, why is everyone acting like buprenorphine is some miracle cure? It’s still an opioid. Just… fancy. And yes, I’m the one who cried at the baby shower because the nurse said ‘congrats’ like I didn’t just survive a nightmare.
Nikhil Pattni
December 11, 2025 AT 07:47 AMOkay so I read this whole thing and I’m just gonna drop some facts. First, methadone is not the same as heroin, even though people confuse them. Methadone is a synthetic opioid with a half-life of 24-36 hours, which means it stabilizes the CNS without the spikes. Buprenorphine is a partial agonist so it has a ceiling effect - meaning overdose risk is lower. Naltrexone is an antagonist, so it blocks receptors completely, which is why it’s risky if someone relapses - they could OD because they’d need way more to feel anything. Also, breastfeeding is safe because the plasma concentration in milk is like 0.2-0.5% of maternal dose - negligible. And the Finnegan scale? Outdated. Eat Sleep Console is better because it’s functional, not just symptom-counting. Also, rural access is a joke - only 28% of clinics have MAT? That’s criminal. And don’t even get me started on how Medicaid doesn’t cover transportation to clinics in Appalachia. This isn’t just medical - it’s structural inequality. Also, the 22% drop in NAS severity with integrated care? That’s not magic - that’s basic human decency. Why are we still debating this?
Arun Kumar Raut
December 13, 2025 AT 01:38 AMHey, if you’re reading this and you’re pregnant and using - you’re not alone. I was there. I thought I was a bad mom. But getting on buprenorphine didn’t make me weak - it made me strong. My baby was born calm, fed well, and we breastfed. I didn’t need to hide anymore. You deserve care. Not judgment. Reach out. Someone will help you. You got this.
precious amzy
December 14, 2025 AT 07:40 AMOne cannot help but observe the anthropological paradox at play here: the medicalization of moral failure. We have, in the span of two decades, transformed a behavioral condition - one historically viewed through the lens of personal responsibility - into a neurochemical imperative requiring pharmacological intervention. Is this not merely a rebranding of vice as pathology? The invocation of ‘standard of care’ functions as a rhetorical shield against deeper societal decay. One must ask: if we treat addiction as a disease, what becomes of agency? And if we prioritize fetal outcomes over maternal autonomy, are we not constructing a new form of obstetric paternalism? The ‘Eat, Sleep, Console’ protocol, while seemingly benign, is merely the soothing balm of a system unwilling to confront its own complicity in the erosion of familial integrity. The data is compelling, yes - but data is not wisdom.
iswarya bala
December 15, 2025 AT 04:22 AMomg i just found out my cousin is on buprenorphine and shes preggo and i was like wait is that safe?? thx for this post!! 😭
Simran Chettiar
December 16, 2025 AT 13:40 PMIt is imperative to acknowledge that the paradigm shift towards medication-assisted treatment constitutes not merely a clinical evolution, but a sociopolitical recalibration of maternal identity. The conflation of therapeutic compliance with moral virtue, as subtly implied by the discourse surrounding ‘progress’ and ‘better chances,’ risks infantilizing the pregnant individual. One must interrogate the implicit hierarchy: the mother who adheres to protocol is deemed ‘responsible,’ while the one who does not is pathologized. The very language of ‘staying in treatment’ implies a state of perpetual dependency - a condition that, while medically necessary, may inadvertently reinforce stigma under the guise of compassion. Furthermore, the emphasis on infant outcomes, while laudable, risks reducing maternal experience to a vessel - a biological substrate for fetal well-being. Where, then, is the space for maternal subjectivity? The answer, I suspect, remains elusive within a system that measures success in Finnegan scores rather than in lived dignity.
Anna Roh
December 16, 2025 AT 13:49 PMSo… we’re just giving pregnant women more drugs? And calling it ‘care’? Whatever. I’m just glad I didn’t have to deal with this.
Katherine Chan
December 18, 2025 AT 12:17 PMyou are not broken you are healing 💪 i know it feels like the whole world is judging you but you’re doing the hardest thing right now - showing up. your baby feels your love even when you’re scared. keep going. ask for help. you’re not alone. i believe in you
Philippa Barraclough
December 20, 2025 AT 04:10 AMIt is curious that the literature consistently emphasizes the safety of buprenorphine over methadone, yet the retention rates for methadone remain superior. One might posit that the preference for buprenorphine is less a function of clinical efficacy and more a reflection of cultural perceptions surrounding stigma - the sublingual film being perceived as less ‘institutional’ than daily clinic visits. Furthermore, the absence of standardized monitoring protocols across U.S. hospitals suggests a fragmentation of care that is not merely logistical, but epistemological: we lack consensus on what constitutes ‘normal’ neonatal behavior post-exposure. The Eat, Sleep, Console model is intuitively appealing, yet its adoption remains uneven. Is this a failure of training, or of institutional will? The data is clear, but implementation is not. And until we address the infrastructure - the lack of social workers, the absence of childcare support, the geographic disparities - we are merely rearranging deck chairs on the Titanic.
Tim Tinh
December 20, 2025 AT 07:40 AMmy sister just had a baby on buprenorphine and they didn’t even give her meds for withdrawal - just held her all day, fed her every 2 hours, and kept the room dark. she’s doing amazing. people need to stop acting like MAT = bad mom. it’s literally the opposite.
Olivia Portier
December 22, 2025 AT 05:48 AMthank you for saying breastfeeding is safe - my nurse told me i was ‘putting my baby at risk’ and i cried for an hour. i’m so glad i found this. i breastfed for 6 months and my baby never had to go to the NICU. you’re not a bad mom for needing help. you’re a good mom for asking for it.
Tiffany Sowby
December 23, 2025 AT 00:48 AMSo let me get this straight - we’re giving drugs to pregnant women because ‘it’s safer’? And now we’re telling the rest of us to stop judging? What happened to personal responsibility? This isn’t medicine - it’s enabling. And why are we letting women in rural areas ‘get care’ when they don’t even show up until labor? That’s not a healthcare crisis - that’s a moral one. I’m not heartless. I’m just tired of society rewarding bad choices with taxpayer-funded treatment.