More than 10% of Americans carry a label saying they’re allergic to penicillin. But here’s the truth: over 95% of them aren’t actually allergic. That mislabeling isn’t just a paperwork error-it’s costing lives, increasing antibiotic resistance, and driving up medical bills. If you’ve been told you’re allergic to penicillin-or any antibiotic-based on a childhood rash, a stomachache, or a doctor’s guess, you might be avoiding safe, effective drugs without reason.
Why False Allergy Labels Are a Hidden Crisis
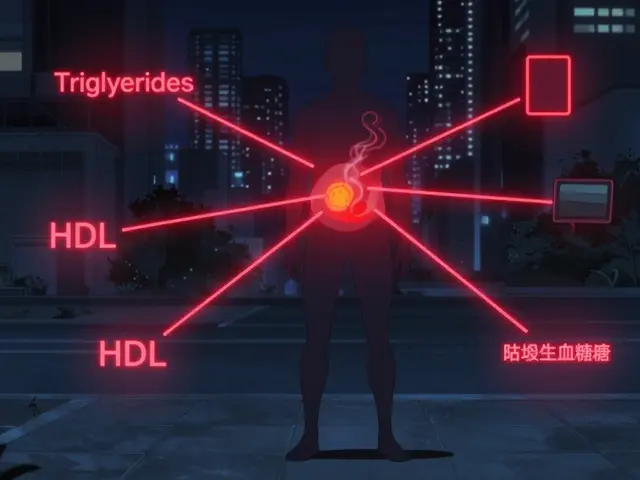
When a patient is labeled allergic to penicillin, doctors often switch to broader-spectrum antibiotics like vancomycin, clindamycin, or fluoroquinolones. These drugs aren’t just more expensive-they’re less precise. They kill off good bacteria, increase the risk of deadly infections like C. diff, and fuel the rise of superbugs. The CDC estimates that false penicillin allergy labels contribute to 50,000 extra C. diff cases every year in the U.S. alone, adding $650 million to healthcare costs. And it’s not just about infections. Patients with false labels face longer hospital stays, higher rates of surgical complications, and fewer treatment options when they really need help. A 68-year-old woman from Massachusetts General Hospital had avoided penicillin for 40 years because of a rash at age 5. She ended up hospitalized three times for stubborn UTIs. After testing proved she wasn’t allergic, she was treated with a simple amoxicillin course-and never had another hospital visit for two years. That one test saved an estimated $28,500.How Do You Know If Your Allergy Label Is Real?
Most people who say they’re allergic to penicillin never had a proper test. They might’ve had a rash after taking the drug as a kid, or their parent said they were allergic, or a nurse noted "allergic" in the chart without confirmation. Real IgE-mediated penicillin allergies-those that cause anaphylaxis-are rare. Only 1-2% of people who carry the label actually have them. The biggest red flag? If your reaction was:- A rash that didn’t blister or peel
- Stomach upset, nausea, or diarrhea
- A headache or dizziness
- Something that happened more than 10 years ago
What Does Drug Allergy Testing Actually Look Like?
Testing isn’t scary. It’s safe, quick, and often done right in your doctor’s office. There are two main steps:- Skin testing-a tiny amount of penicillin is placed on your skin, then gently pricked. If you’re allergic, you’ll get a red, itchy bump within 15-20 minutes. This test is highly accurate for immediate reactions.
- Oral challenge-if skin testing is negative, you’ll take a small dose of penicillin (like amoxicillin) under observation. You’ll be monitored for 30-60 minutes. If nothing happens, you’ll take a full therapeutic dose.
Who Can Do the Testing?
You don’t need to see an allergist in a big city. More and more primary care doctors, pharmacists, and even nurse practitioners are trained to do this. A 2021 study found that after just 10 supervised cases, non-allergists were able to perform the testing with 92% accuracy and fewer than 2% of errors. Hospitals like the University of Pennsylvania have built entire programs around it. Since 2020, they’ve tested over 1,800 patients with zero severe reactions. The key? Using a simple tool called PEN-FAST. It asks five questions:- Was the reaction 5 or more years ago?
- Was it just a rash?
- Was there no anaphylaxis or angioedema?
- Was there no treatment needed?
- Was the reaction not confirmed by testing?
What Happens After You’re Cleared?
Getting cleared isn’t the end-it’s the beginning. You need to make sure your medical records reflect the change. Too many patients test negative but still have "penicillin allergy" listed in their chart because the system didn’t update. Your allergy status should be updated to say something like: "Penicillin allergy ruled out by skin testing and oral challenge on [date]. Tolerated amoxicillin without reaction." Don’t just rely on "allergy removed." Be specific. Cross-reactivity between different penicillins and cephalosporins varies. If you’re cleared for amoxicillin, you might still need testing for other beta-lactams. And tell your pharmacist. Tell your dentist. Tell your next doctor. You’re not just helping yourself-you’re helping the system. Fewer broad-spectrum antibiotics prescribed means less resistance for everyone.
Barriers to Testing-and How to Overcome Them
Despite the evidence, fewer than 40% of eligible patients get tested. Why?- Wait times-some clinics have 14-week backlogs for allergy appointments.
- Doctors don’t know how-many aren’t trained in de-labeling protocols.
- Patient fear-people worry testing will trigger a reaction.
- Electronic health records-many systems don’t let you easily remove or update allergy flags.
- Ask your primary care doctor: "Can we test me for penicillin allergy?" Don’t wait for them to bring it up.
- If they say no, ask for a referral to a pharmacist with allergy training or a local clinic that runs de-labeling programs.
- Check if your hospital has an antibiotic stewardship program-they often run these tests.
- Use the PEN-FAST tool yourself. If you score under 3, you’re low risk and eligible for direct challenge.
The Bigger Picture: Why This Matters for Everyone
This isn’t just about you. False allergy labels are making antibiotics useless for everyone. When we overuse vancomycin and azithromycin, bacteria evolve to resist them. MRSA and drug-resistant E. coli are spreading because we’re using blunt tools when we could be using scalpels. The CDC, Infectious Diseases Society of America, and American Academy of Allergy all agree: penicillin allergy de-labeling belongs in every antibiotic stewardship program. Starting in 2025, Medicare will even start rewarding hospitals that reduce inappropriate antibiotic use linked to false allergy labels. And it’s working. Epic Systems, which runs EHRs in 84% of U.S. hospitals, added an automated penicillin de-labeling tool in 2021. Since then, over 198,000 false labels have been removed. That’s nearly 200,000 people who can now safely take the best drug for their infection.What to Do Next
If you’ve been told you’re allergic to penicillin:- Look back at your reaction. Was it a rash? Stomach upset? Something that happened over 10 years ago?
- Use the PEN-FAST tool. Answer those five questions. If you scored under 3, you’re likely not allergic.
- Ask your doctor for a referral to a de-labeling program. If they don’t know what you’re talking about, ask for a pharmacist or an allergist.
- Don’t wait. Every day you avoid penicillin, you’re contributing to a public health crisis.
- When you’re cleared, make sure your records are updated-and tell everyone who treats you.
Can I be allergic to penicillin if I never had a reaction before?
No. A true penicillin allergy requires a prior immune response. If you’ve taken penicillin before without symptoms like hives, swelling, or trouble breathing, you’re very unlikely to suddenly become allergic. Many people are mislabeled based on childhood rashes that were viral, not allergic.
Is penicillin allergy testing painful?
Skin testing feels like a tiny pinch-less than a mosquito bite. The oral challenge involves swallowing a pill or liquid. Most people feel nothing. There’s no injection, no IV, and no needles beyond the skin test. The entire process is designed to be as comfortable as possible.
How long does the whole testing process take?
Most people complete testing in under two hours. Skin testing takes about 30 minutes to read results. The oral challenge requires 30-60 minutes of observation after each dose. Some clinics offer same-day results. If you’re low risk, you might be cleared in a single visit.
Will my insurance cover drug allergy testing?
Yes. Most insurance plans, including Medicare and Medicaid, cover allergy testing for drug hypersensitivity when it’s medically indicated. Many hospitals offer the test at no cost as part of their antibiotic stewardship programs. Always ask your provider about costs upfront.
Can I be allergic to one penicillin but not another?
Yes. Penicillin is a class of drugs, and cross-reactivity varies. Being allergic to amoxicillin doesn’t mean you’re allergic to ampicillin or cephalexin. That’s why testing should specify the exact drug. After testing, your record should say "tolerated amoxicillin," not just "not allergic to penicillin."
What if I have a reaction during testing?
Reactions during testing are rare-and clinics are prepared. If you develop hives, swelling, or breathing issues, staff will immediately stop the test and give you antihistamines or epinephrine. These reactions are mild in over 98% of cases and easily managed. The risk of a reaction during testing is far lower than the risk of complications from using a less effective antibiotic.
Can I get tested if I’m pregnant?
Yes. Penicillin is one of the safest antibiotics during pregnancy. If you’ve been avoiding it due to a false label, testing is not only safe-it’s recommended. Skin testing and oral challenges are routinely performed on pregnant patients with no increased risk to mother or baby.







Comments (13)
Glendon Cone
December 31, 2025 AT 17:55 PMWow, this is wild. I’ve been told I’m allergic to penicillin since I was 7 because of a rash that turned out to be chickenpox. 😅 Got tested last year-turned out I’m fine. Now I take amoxicillin like it’s candy. Saved my butt during a sinus infection last winter. Why isn’t this common knowledge??
Henry Ward
January 1, 2026 AT 08:07 AMOf course it’s a crisis. Because the medical-industrial complex doesn’t want you to know you’ve been getting overprescribed antibiotics for decades. They profit from your ignorance. This isn’t about health-it’s about control. You think your doctor cares? They’re just following the EHR prompts. Wake up.
Shae Chapman
January 1, 2026 AT 17:59 PMI cried reading this. My mom had a false label for 50 years. She got pneumonia last year and they gave her vancomycin-she was in the hospital for 3 weeks. After testing? Just amoxicillin. She’s back to gardening. 🥹 Thank you for writing this. I’m sending it to everyone I know.
Nadia Spira
January 1, 2026 AT 21:51 PMLet’s deconstruct the epistemological framework here: the conflation of symptomatology with immunological truth is a product of ontological laziness within allopathic medicine. The PEN-FAST algorithm is a neoliberal technocratic solution to a systemic failure of diagnostic epistemic humility. You’re not ‘cleared’-you’re assimilated into a pharmacological orthodoxy that still pathologizes uncertainty.
henry mateo
January 2, 2026 AT 16:04 PMjust read this and i think i might be one of those people. i had a rash when i was 10 and they just put 'allergic' in my file. never thought to question it. gonna ask my doc next week. thanks for the nudge 🙏
Kunal Karakoti
January 4, 2026 AT 11:03 AMIn India, we rarely label people allergic without testing. But we also rarely have access to penicillin at all. The irony is that the wealthy get mislabeled, while the poor never get the chance to be labeled. This is a first-world problem with third-world consequences.
Joseph Corry
January 5, 2026 AT 11:58 AMAnother virtue-signaling piece from the medical establishment. ‘Save money’? Please. The real savings come from reducing liability and pushing patients toward branded alternatives. And don’t get me started on how ‘oral challenge’ is just a glorified placebo test. If you’re so sure, why not just give the full dose without observation? Hypocrisy.
Colin L
January 6, 2026 AT 08:53 AMI remember when I was a kid, my mum said I was allergic to penicillin because I got a rash after taking it for a throat infection. But here’s the thing-I didn’t even have a throat infection. It was just a cold. And the rash? Probably from the soap I started using that week. Fast forward 25 years, I’m in my 40s, and I’ve been prescribed azithromycin for every little thing. I’ve had C. diff twice. I’ve had yeast infections so bad I couldn’t sit down. And now I’m being told I could’ve just taken amoxicillin all along? I’m furious. And also… relieved? I don’t even know how to feel. I’m going to book a test tomorrow. I hope it’s not too late.
Hayley Ash
January 6, 2026 AT 18:05 PMOh great another ‘you’re not allergic’ article. Next they’ll tell me my fear of spiders is just a cultural construct and I should go hug one. Sure. Let me just swallow a pill in a clinic because some guy with a clipboard says I’m ‘low risk.’ And then when I go into anaphylaxis, who gets sued? You? No. Me. Thanks for the life advice, Karen.
kelly tracy
January 8, 2026 AT 16:01 PMEveryone’s so excited about this ‘testing’ but no one talks about how the system will NEVER update your records. I got tested in 2021. My chart still says ‘penicillin allergy.’ I had to call the hospital 7 times. They said ‘we don’t remove allergies, we just add a note.’ So now I have TWO conflicting entries. Brilliant.
Cheyenne Sims
January 8, 2026 AT 16:07 PMIt is imperative that patients adhere to established medical protocols regarding hypersensitivity. The absence of documented clinical evidence does not negate the potential for life-threatening reactions. This article presents a dangerously oversimplified narrative that undermines the foundational principles of clinical safety. The consequences of premature de-labeling are not merely theoretical-they are documented, fatal, and entirely preventable. I urge caution.
Kelly Gerrard
January 9, 2026 AT 12:56 PMThis is a game-changer. I’ve been avoiding penicillin since I was 8. Now I’m 32. I just booked my test. Thank you for giving me back my health. 🙏
Aayush Khandelwal
January 10, 2026 AT 04:58 AMPenicillin de-labeling is the ultimate hack of the biomedical system. It’s not just about drugs-it’s about reclaiming agency from algorithmic medicine. The PEN-FAST tool? It’s a poetic subversion of bureaucratic inertia. We’re not just removing labels-we’re dismantling the myth that medicine knows best. I’ve done it. My cousin did it. My neighbor did it. Now my aunt’s in line. This isn’t science. It’s liberation.