

When we talk about community programs, organized local efforts that connect people to health resources, education, and support outside of clinics and hospitals. Also known as public health initiatives, these programs fill gaps that doctors and pharmacies can’t reach on their own. Think of them as the quiet backbone of real-world health — not flashy, but essential. They’re the free blood pressure checks at the library, the pharmacist leading a class on how to take your meds safely, or the group that drives seniors to their appointments. These aren’t optional extras. They’re what keep people from falling through the cracks.
Many of the issues covered in our posts — like medication side effects, unwanted reactions to drugs that can be managed with better support and monitoring, or deprescribing seniors, the careful process of stopping unnecessary medications in older adults — don’t just happen in medical charts. They happen in homes, in cars, in kitchens where someone forgets to take their pill or is too scared to ask their doctor a question. Community programs step in here. They turn complex medical info into simple, relatable advice. They train neighbors to recognize signs of trouble, help people track lab tests with printable calendars, and teach how to report side effects clearly so doctors actually listen.
These programs also tackle bigger problems like healthcare access, the ability to get timely, affordable care regardless of income or location. A person in a rural town might not have a nearby pharmacy that stocks cheap generics. A community program might set up a monthly drop-off for discounted meds. Someone on multiple drugs might not know grapefruit ruins their blood pressure pill — but a local health worker can explain it in plain language during a cooking class. These aren’t theoretical fixes. They’re daily actions that save lives.
And they’re not just for the elderly or low-income. Anyone can benefit. If you’ve ever wondered how to time zinc with antibiotics, or if caffeine makes your ADHD meds too strong, you’re already dealing with the kind of real-life questions community programs answer. They don’t replace doctors — they make doctors’ advice stick.
What you’ll find in the posts below is a collection of real stories and practical guides that show how these programs work in practice. From how to report side effects so they’re taken seriously, to why lab monitoring calendars help people stay safe on risky drugs, every article ties back to one truth: health doesn’t live in a hospital. It lives in neighborhoods, in conversations, in the small habits people build with help. These aren’t just medical topics — they’re human ones. And that’s where community programs make the biggest difference.
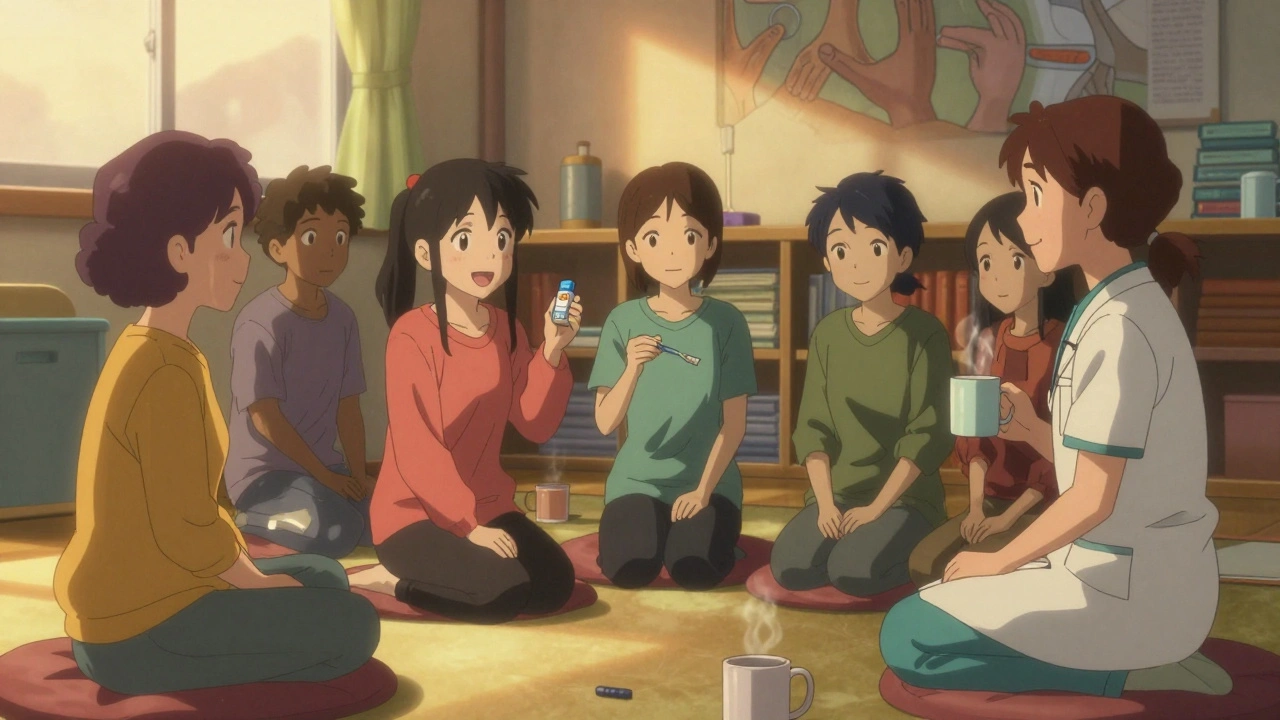
Support groups and community programs help people stick to their meds by offering real-life advice, peer connection, and practical support-proven to cut hospital visits and improve health outcomes.