Most people think of chestnuts as festive treats roasting on an open fire or tossed into hearty European recipes, but hidden behind their sweet, starchy flesh is a tricky reality: for some, chestnuts can bring on an allergic storm that’s every bit as serious as classic tree nuts. Chestnuts aren’t just another Christmas staple; they stand at the crossroads of food reactions, cross-allergies, and sneaky symptoms that can trip you up if you’re not paying close attention. You might believe you’re safe if you avoid walnuts, pecans, and cashews, but chestnuts might just be your blind spot. Ready to find out how this can mess with your plans?
The Science Behind Chestnut Allergies
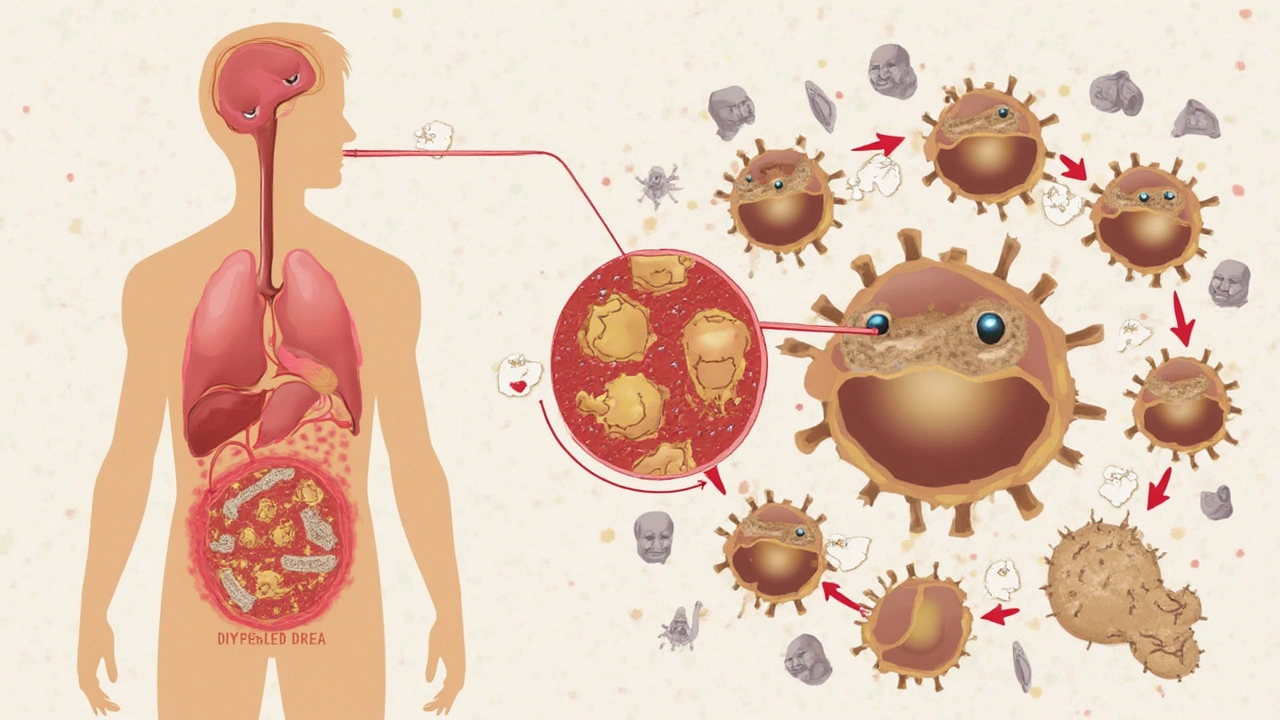
Chestnut allergy isn’t as rare as it sounds—at least, not in the UK and Europe, where the European or sweet chestnut (Castanea sativa) is common in markets and kitchens. It’s not the same thing as a peanut allergy, even though both can be severe. Chestnuts belong to a different botanical family than your typical tree nuts. Yet, the proteins inside chestnut are surprisingly similar to those in other nuts—and even in certain fruits and latex. This is where things get complicated. When you eat a chestnut, your immune system might think it’s being attacked, especially if you already react to apple, kiwi, avocado, or even latex gloves. This shared trait is called cross-reactivity.
The classic allergen in chestnut is called "Cast s 1," which is a chitinase protein. If you’ve ever reacted to bananas, avocados, or even that odd itch after eating raw tomatoes, you might have what's known as latex-fruit syndrome. That’s because these foods and chestnuts share protein structures your immune cells find hard to tell apart. The funny—and slightly annoying—thing is, some folks go years eating chestnuts with no problem, until one day, boom: itchy mouth, swelling lips, maybe even trouble swallowing or breathing. That’s how unpredictable allergies can be.
It isn’t only about eating whole chestnuts, either. Some people react to chestnut flour, an ingredient sneaking into gluten-free baking and artisanal breads. And then there’s the bizarre but real case of folks who only react to uncooked chestnuts—cooking seems to break down the troubling proteins for them. If that sounds niche, consider this: chestnut trees are also related to oak and beech, and if you struggle with hay fever or pollen allergies, there’s an added layer of risk. Your immune system can get confused by all these similar bits of protein, turning something as harmless as autumnal foraging into a sneezing, itchy nightmare.
And just so you know, actual horse chestnuts (Aesculus hippocastanum)—those shiny round seeds you find on the ground—aren’t edible and don’t cause food allergies. It’s the European chestnut you’ll find roasted at markets or used in chestnut spread that’s the culprit.
Symptoms: What Happens If You're Allergic?
Chestnut allergy symptoms run the full spectrum from mild to "drop everything and run to A&E" serious. For most people, it’s a classic oral allergy syndrome (OAS)—you take a bite, and suddenly your lips or mouth start tingling, maybe a burning sensation kicks in. Sometimes your throat gets scratchy, and you feel like you need to clear it constantly. If you’ve already got pollen allergies, this oral reaction can get triggered faster and with smaller amounts of chestnut.
But it doesn’t stop at the mouth. More severe cases involve hives, wheezing, swelling around the face or neck, vomiting, stomach cramps, or even a sudden drop in blood pressure (anaphylaxis). Doctors have seen folks who only touched raw chestnuts at a market stall, then rubbed their eyes, and ended up with red, itchy skin around their eyes. That’s called contact urticaria.
If you’ve ever had bad allergic reactions to bananas, avocados, or even latex gloves (think medical settings or kitchen chores), pay extra attention. Due to the protein similarities, this is one allergy that loves to crossover and play tricks. And age doesn’t offer you much immunity; adults can randomly develop new sensitivities even after years of safe chestnut snacking.
Something many people don’t realise: cross-reactivity means you might also react to tree pollen or foods in the Rosaceae family (apples, cherries, peaches). If you spot redness, swelling, trouble breathing, or fast heartbeat after eating chestnuts, don’t brush it off as a fluke. Symptoms aren’t just annoying—they can be life-threatening. Find a quick and clear list of warning signs and deeper info about chestnut allergy symptoms from health professionals before you risk another mouthful.
The unpredictability of symptom severity can catch even experienced allergy sufferers out. One day you might have nothing but a tickle; next time, you’re calling for help. The immune system is funny like that—it’s rarely consistent. Hang onto that bit of knowledge if you’re ever in doubt after chestnut exposure.

Cross-Reactivity: Why Tree Nut Allergies Raise Chestnut Risks
If you know you have a strong reaction to classic tree nuts like hazelnuts, walnuts, or cashews, you probably keep an eye on ingredient lists. But here’s a kicker—just because chestnuts aren’t classified as the same "tree nut family" doesn’t mean you’re in the clear. Research straight out of allergy clinics in Europe has shown that up to 50% of people with tree nut allergies can also react to chestnut proteins, thanks to that protein family overlap.
This cross-reactivity creates double trouble for those with broader food allergies. For example, people with oral allergy syndrome tied to birch pollen (very common in the UK during spring) are more likely to react to chestnuts than those without pollen allergies. That’s because birch, apple, hazelnut, and chestnut all share certain protein profiles, causing the immune system to get unnecessarily worked up. Cross-reactions can even be unidirectional—you might be fine with chestnuts but can’t touch hazelnuts, or vice versa. It’s like your immune system flips a coin and picks battles at random.
And it gets weirder. A chunk of people react to chestnuts not because of the nuts themselves, but because their immune system remembers a long-standing latex allergy. Health workers, chefs, or kids who had frequent surgeries with latex gloves are at greater risk here. Think about how many times you’ve worn rubber gloves during cleaning or food prep—your immune system can make the leap from latex to chestnut surprisingly easily. This is called latex-chestnut syndrome and is a classic studied case in European allergy textbooks.
Mixing up what you’re sensitive to is easier than you’d expect. Some allergists recommend annual re-testing because food allergies can shift over time, especially in kids or people with changing immune systems. Even if you’ve outgrown your childhood nut allergy, there’s no guarantee chestnuts are safe for life. Other contributors—such as pollution, changing diets, or climate shifts—may even increase the chance that cross-reactivity shows up later in adulthood.
If you’ve got a family history of mixed allergies or you’re someone already dodging food triggers, keep chestnuts on your radar. It might just save you a world of hassle.
Getting Diagnosed: Tests That Actually Help
If you suspect chestnuts are messing with your immune system, don’t rely on guesswork. The gold standard for allergy detection is a mix of skin prick tests, specific IgE blood tests, and—when it’s safe to do so—supervised food challenges. Most GPs in the UK will start with a chat about your symptoms, then refer you to an allergist for further workup. One quirky but useful fact: chestnut allergy testing sometimes uses extracts of the raw nut, as roasting can change the protein structure and make the test less accurate.
If you have related allergies (tree nuts, latex, avocado), mention it openly. Some clinics offer allergy panels that target potential food and latex cross-reactions so you don’t have to be tested individually for every single foodstuff. If you deal with hay fever or pollen issues, let your doctor know—there are even tests that check for specific birch, oak, or beech pollen allergies, all of which can up your risk with chestnuts.
Blood tests aren’t perfect, but they can pinpoint whether your immune system churns out IgE antibodies specific to chestnuts. High levels mean you’re probably sensitive, but low or borderline numbers aren’t always a free pass. Think of it as another clue rather than a definite diagnosis. In some specialist centres, food challenges are closely supervised, starting with tiny doses and ramping up only if there are no issues. This is risky business though, so never try this at home—leave it to the pros with EpiPens ready.
If you’ve got kids, be especially alert. Young ones may not explain their symptoms clearly, so even vague complaints about an itchy mouth or upset tummy after eating chestnut should put you on alert. Bring a food diary if you’re going for allergy tests; timing, amount eaten, and the exact symptoms (was it hives, sore throat, or upset stomach?) make a big difference in making the right call.
And don’t rule out multiple triggers. It’s possible to have a full house—reacting to chestnuts, latex, and certain fruits. The more detailed picture you can give your allergy specialist, the better your long-term action plan will be.
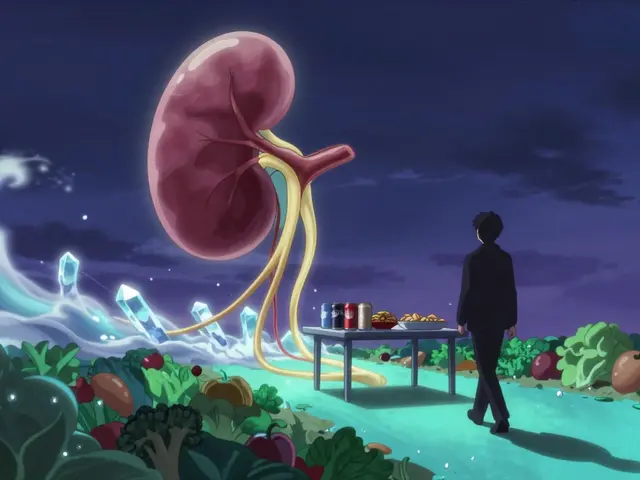
Prevention and Everyday Living with Chestnut Allergy
So you or someone you know has a confirmed chestnut allergy? Life doesn’t have to get boring, but you will need to stay on your toes. The first line of defence is the usual drill: check labels ruthlessly. Chestnuts aren’t always labeled as “nuts”—sometimes you’ll find words like “marron” or “castagna” on ingredient lists, especially in imported foods and restaurant desserts. Chestnut flour shows up in trendy gluten-free bakes, so don’t let your guard down at cafes or artisan bakeries.
If you’re eating out, speak up. Don’t just ask if something contains chestnuts—mention the allergy and double-check whether chestnut flour or purée is in sauces or pastries. Chefs like to get creative, and chestnut puree is a sneaky staple in some upscale dishes (like Mont Blanc desserts, holiday stuffing, and wild game gravies). Get into the habit of carrying your own snacks, especially if you’re travelling in Europe, where chestnut treats are popular street food in colder months.
If you or your kids are at risk of severe reactions, you already know the drill: an adrenaline (epinephrine) auto-injector should always be close at hand. Make sure everyone around you—family, friends, colleagues—knows how to use it. Medical alert bracelets are a smart backup in case you need help fast and can’t speak for yourself.
For those with latex allergies, avoid chestnuts and always flag both allergies to your GP and dentist. Sometimes even the “natural flavourings” or extracts in toothpastes and sweets can cause a reaction. If you’re a keen cook or work with raw chestnuts for crafts or holiday stuff, wear non-latex gloves to cut the risk of a contact reaction, and wash up thoroughly when done.
Don’t slack off just because cooking destroys some proteins in chestnuts. A few folks only react to raw or undercooked versions, but most will have symptoms regardless of prep method. Supermarkets sometimes bundle chestnuts with other unlabeled foods or nuts in display bins—cross-contamination is a real risk, so steer clear if you can’t be sure the product is nut-free.
Allergy apps that scan barcodes, regular checks of ingredient lists (they do get updated!), and a well-rehearsed emergency plan will become your best mates. If you’ve got a sweet tooth and don’t want to give up festive bakes, try swapping in pumpkin, sweet potato, or cooked apple for a similar taste with zero allergy drama. At parties and gatherings, don’t shy away from bringing your own safe version of a favourite dish—most friends will appreciate the heads up and the extra treat.
Kids might need help practicing how to say “I have a chestnut allergy” confidently, especially if they’re at school or parties. Teachers, carers, and club leaders should all have allergy action plans and know where your child’s medication is. As a Manchester local, I’ve found many cafes and food halls surprisingly receptive—just speak up, and staff are usually happy to help you find safe options. Protecting yourself isn’t about being fearful; it’s about being fully informed, so you can focus on enjoying the good stuff—without the risk.








Comments (10)
Preeti Sharma
July 17, 2025 AT 00:15 AMYou know, the whole idea of chestnut allergies triggering reactions often seems overblown to me. Sure, people can be allergic to anything, but chestnuts? Not the usual suspect in the nut allergy lineup. Most folks freak out about peanuts or tree nuts like walnuts, but chestnuts? I think society just clings to allergy fears because it helps create more sensational news, not because it's a huge actual threat.
But I admit there's always cross-reactivity, which is fascinating from a biochemical standpoint. The way proteins can mimic each other between nuts is wild. Still, I wonder if the preventative tips people follow are sometimes more about anxiety than necessity.
So, what is the real rate of chestnut allergy? Are people mistaking oral allergy syndrome for a full-blown allergic reaction? It would help if there were more nuanced discussions about the severity and prevalence before everyone goes avoiding chestnuts entirely.
Ted G
July 18, 2025 AT 04:16 AMThis is exactly the kind of topic where you gotta be suspicious. Allergies aren’t just random, you know? It’s like there’s a deeper agenda at play, maybe pushing people to buy more allergy tests or medicine. Chestnuts being singled out? Convenient. Anyone else think this is just part of a big pharma push to keep us anxious and dependent?
I bet there’s some shady stuff behind how these allergy connections between nuts are researched too. Skepticism is healthy when it comes to these 'cross-reactivity' claims. What’s likely is that the symptom descriptions are exaggerated for marketing.
People should question where the info is coming from, and not just take it all at face value. Otherwise we’re trapped in this never-ending cycle of allergy paranoia that lines someone’s pockets. Just my take.
Miriam Bresticker
July 19, 2025 AT 08:20 AMomg, this article rlly hit home for me! I’ve struggled with various nut allergies since childhood but chestnuts were a mystery 😅
The cross-reactivity part explains a lot tho, cuz I got tested for tree nut allergy and it’s confusing which nuts to avoid exactly. The symptoms can be so subtle or crazy intense 😵💫 like, sometimes my throat gets itchy for no obvious reason after eating things that might have traces of chestnuts?
💡 The prevention tips were super helpful! I’m gonna try keeping an allergy diary now to track any sneaky reactions I overlooked. It’s def not just paranoia when you have these random symptoms showing up, right?
Thanks for the informative read, I feel more empowered now! 🤗✨
Claire Willett
July 20, 2025 AT 12:23 PMThis is a solid resource for anyone navigating the complexities of nut allergies and cross-reactivity. From a clinical perspective, the proteins involved in chestnut allergies are quite homologous to those in other tree nuts, which sheds light on why some patients experience simultaneous reactions.
Interestingly, the oral allergy syndrome component often complicates diagnosis, as symptoms can be mild and mistaken for other issues. That’s why I always recommend patients get comprehensive skin prick or IgE testing, combined with food challenges under medical supervision, to clarify the diagnosis.
For prevention, strict avoidance and reading labels meticulously is critical. It’s not enough to trust casual assurance; cross-contamination is prevalent in food manufacturing. This article correctly points that out.
Dominique Jacobs
July 21, 2025 AT 16:26 PMLet's not dance around it — nut allergies, including chestnuts, can be seriously dangerous. People underestimate this because chestnuts aren’t as common in some diets, but that doesn’t mean they aren’t potent allergens.
Cross-reactivity is huge here — if you're allergic to one tree nut, chestnuts could easily trigger a reaction even if you've never eaten them before. That can be scary and often sneaky, because it might present with mild symptoms first, then blow up later.
Everyone planning to eat chestnuts, especially if they have known allergies, should listen up and get tested officially. Playing it safe with prevention strategies like carrying antihistamines or epinephrine auto-injectors isn’t a joke — it’s survival.
olivia guerrero
July 22, 2025 AT 20:30 PMAbsolutely love how this article lays everything out clearly!!! 🌟 Chestnut allergies can totally sneak up on you, especially if you’ve got other tree nut sensitivities, which is why staying vigilant is so important!!!
Don’t ever feel bad about being cautious — your health always comes first!!! 🙌 Tips like carrying an allergy action plan and informing those around you about your risks can literally save your life!!!
Keep spreading awareness and positivity about how to stay safe while still enjoying the things you love!!! That balance is so key!!! 💖
Benton Myers
July 24, 2025 AT 00:33 AMJust reading through this, I can’t help but think about how underrated chestnuts are in both nutrition and allergen discussions.
It’s interesting to note that many people assume chestnuts are similar to other nuts, but their botanical family is quite different. This nuance might explain the complexity of allergic reactions and cross-reactivity outlined in the article.
Regardless, the clear advice on prevention and testing is crucial. It’s a calm reminder that understanding your body’s responses is actually empowering.
Pat Mills
July 25, 2025 AT 04:36 AMLet me just say, this whole allergy panic around chestnuts and nuts in general feels blown WAY out of proportion.
There’s a healthy way to approach food without turning every bite into a potential emergency. I get people have allergies, and some cases are serious, but the media hype and constant warnings turn normal eating into a paranoid nightmare.
Truth is, if you prep yourself and are sensible about your intake with proper tests, you won’t have problems. But the narrative that chestnuts are some silent danger waiting to attack? Nah, that’s fearmongering plain and simple.
Matt Tait
July 26, 2025 AT 08:40 AMHonestly, the amount of misinformation and half-truths about chestnut allergies is staggering. If you ask me, most people commenting here are either exaggerating or underselling the danger.
Sure, cross-reactivity exists, but unless you have verified IgE-mediated allergy, you’re just playing guessing games. And let's be real, some of these prevention tips feel like common-sense advice dressed up as medical gospel.
Bottom line: Get tested, consult an allergist, stop googling random symptoms, and chill out. The internet isn’t your personal doctor.
Claire Kondash
July 27, 2025 AT 12:43 PMReading this piece conjures a bittersweet tapestry of thoughts about the human condition and our complex relationship with nature’s bounty. The potential for chestnuts to provoke allergic manifestations, set against their humble stature in the tree nut hierarchy, feels almost emblematic of the delicate dance between human vulnerability and biological reality.
It calls into question how our sensory perceptions and biochemical idiosyncrasies shape not only our health but also our societal rituals and fears. The detailed discourse on cross-reactivity serves as a metaphorical bridge, weaving together disparate threads of our bodily defenses and environmental interactions.
Ultimately, embracing such knowledge empowers a deeper existential confidence, allowing us to savor life’s seasonal gifts while respecting the invisible limits that define our corporeal existence. 🌰✨🙏