ANC Threshold Alert Calculator
Neutrophil Count Assessment Tool
Enter your absolute neutrophil count (ANC) to determine medical urgency based on guidelines from the Infectious Diseases Society of America.
Critical Assessment Results
What Is Medication-Induced Agranulocytosis?
Agranulocytosis is a rare but life-threatening condition where your body stops producing enough neutrophils - the white blood cells that fight off bacteria and fungi. When your absolute neutrophil count (ANC) drops below 100 per microliter, you’re at serious risk of severe, fast-spreading infections. Even a mild sore throat or low-grade fever can become deadly within hours if not treated immediately. This isn’t just a lab number - it’s a medical emergency.
Unlike regular neutropenia (ANC under 1,500), agranulocytosis leaves you with almost no defense. About 70% of cases are caused by medications, not genetics or viruses. Common culprits include clozapine for schizophrenia, antithyroid drugs like propylthiouracil, certain antibiotics such as trimethoprim-sulfamethoxazole, and even some painkillers like dipyrone. The problem? Many people don’t realize they’re at risk until it’s too late.
How Do Medications Cause This?
There are two main ways drugs trigger agranulocytosis. In about 60% of cases, your immune system mistakes your own neutrophils for invaders. The drug binds to them, your body makes antibodies against them, and your neutrophils get destroyed. This is called immune-mediated agranulocytosis. It can happen suddenly - sometimes within days of starting the drug.
The other 40% is direct bone marrow suppression. The drug poisons the stem cells that make neutrophils. This usually takes weeks to months to show up. Clozapine works this way, which is why it needs strict monitoring. Even if you’ve been on it for a year without issues, your bone marrow can still shut down. There’s no safe window - only risk levels.
Which Medications Carry the Highest Risk?
Not all drugs are equal when it comes to agranulocytosis. Some are far more dangerous than others. Here’s what the data shows:
| Medication | Risk Level | Incidence Rate | Monitoring Requirement |
|---|---|---|---|
| Clozapine | High | 0.77% (1 in 130) | Weekly ANC for first 6 months |
| Propylthiouracil | High | 0.36 per 1,000 patient-years | Monthly ANC for first 6 months |
| Trimethoprim-sulfamethoxazole | High | 15.8x higher than other antibiotics | Consider ANC before long-term use |
| Dipyrone | High | 1.2 per 10,000 patient-years | Restricted in many countries |
| Methimazole | Moderate | 0.16 per 1,000 patient-years | Monthly ANC if used >3 months |
| Ibuprofen | Very Low | Minimal association | Not routinely monitored |
Clozapine is the most notorious. It’s the only drug for treatment-resistant schizophrenia that works for many who’ve tried everything else. But its risk is real. The FDA requires weekly blood tests for the first six months. Even then, about 25% of cases still happen despite monitoring. That’s why newer tools - like the HLA-DQB1*05:02 genetic test - are now being used to screen patients before starting clozapine. If you carry this gene, your risk jumps 14 times higher.

Why Early Symptoms Are Often Missed
Most patients don’t wake up one day with agranulocytosis. They get a sore throat, a fever, or feel unusually tired. These are the first signs - and they’re almost always mistaken for the flu or a cold. A 2022 survey of 347 patients found that 86% waited more than 48 hours before seeking help. Over 60% had their symptoms dismissed by doctors who didn’t connect the dots to their medication.
Here’s the hard truth: if you’re on a high-risk drug and you develop a fever above 38.3°C (101°F), you need a blood test that day. Waiting until tomorrow can cost you your life. The Infectious Diseases Society of America says febrile neutropenia with ANC under 500 is a medical emergency. You need antibiotics within an hour - and they must cover Pseudomonas, a bacteria that thrives in people with zero neutrophils.
How Monitoring Works - And Where It Fails
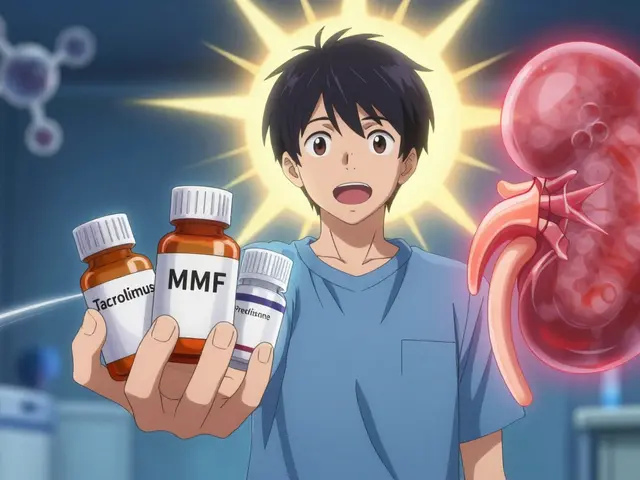
Monitoring isn’t just a suggestion. For clozapine, it’s the law in the U.S. under the REMS program. You must get a complete blood count (CBC) every week for six months, then every two weeks for another six months, then monthly. If your ANC drops below 1,000, treatment stops. If it falls below 500, you’re hospitalized.
But here’s the problem: only 68% of doctors follow these rules. In rural areas, labs are far away. Some patients forget. Others don’t understand the stakes. A 2020 study found 22.7% of clozapine users missed at least one test. That’s not negligence - it’s a system failure.
New technology is helping. Point-of-care devices like the Hemocue WBC DIFF can give you your ANC in five minutes, not two days. These are now approved in the U.S. and Europe. Some clinics use them during clinic visits. Others are pushing for home testing kits. But access is still unequal. In low-income countries, only 32% have any formal monitoring system.
What Happens After Diagnosis?
If you’re diagnosed, the first step is simple: stop the drug. Immediately. No exceptions. Even if you’ve been on it for years and it’s working perfectly, you stop. Recovery usually takes one to three weeks. Your bone marrow will start making neutrophils again - if you haven’t already developed a severe infection.
If you’re sick, you go to the hospital. Broad-spectrum antibiotics start right away. You may need granulocyte colony-stimulating factor (G-CSF), a drug that forces your bone marrow to produce more white cells. In rare cases, you’ll need a stem cell transplant if your marrow is permanently damaged.
But here’s the hopeful part: if caught early and treated fast, death rates drop from 20% to under 5%. That’s the difference between ignoring a fever and acting on it.

What’s New in 2025?
The field is changing fast. In May 2023, the European Hematology Association lowered the intervention threshold from ANC <500 to <1,000. Why? Because data showed 78% of serious infections happened when ANC was between 500 and 1,000. Waiting until it hits 500 is too late.
AI is now being used in electronic health records to flag patients at risk. A 2022 trial across 12 hospitals showed AI alerts reduced missed cases by 47%. That’s huge. Also, pharmacogenomic testing is becoming standard. By 2028, experts predict 40% of high-risk drugs will require genetic screening before prescribing.
But the biggest gap remains access. Rural patients are 2.3 times more likely to die from medication-induced agranulocytosis. Why? No labs. No specialists. No follow-up. This isn’t just a medical issue - it’s a justice issue.
What You Need to Do If You’re on a High-Risk Drug
If you’re taking clozapine, propylthiouracil, or trimethoprim-sulfamethoxazole, here’s your action plan:
- Know your drug’s risk level. Ask your pharmacist or doctor.
- Get your ANC tested on schedule - no exceptions.
- If you have a fever above 38.3°C (101°F), go to the ER today. Say: "I’m on [drug name]. I think I might have agranulocytosis. I need a CBC now."
- Keep a log of your ANC results. Track trends, not just numbers.
- Don’t wait for symptoms. Some people have no warning signs until it’s too late.
- If your clinic doesn’t offer point-of-care testing, ask if they can refer you to one that does.
There’s no magic pill. But with awareness, discipline, and fast action, you can live safely on these drugs. The alternative isn’t just risk - it’s death.
Can agranulocytosis be reversed after stopping the drug?
Yes, in most cases. Once the triggering medication is stopped, the bone marrow typically recovers within 1 to 3 weeks. Neutrophil counts begin rising within days, and full recovery is common unless severe infection or permanent marrow damage has occurred. Recovery speed depends on the drug, how long it was taken, and the patient’s overall health.
Is agranulocytosis always caused by medication?
No. While about 70% of cases are drug-induced, other causes include autoimmune diseases, viral infections like hepatitis or HIV, chemotherapy, radiation, and rare genetic disorders. However, medication remains the most common and preventable cause, especially in adults taking long-term prescriptions.
Can I take over-the-counter painkillers if I’m on a high-risk drug?
Generally, yes - but with caution. Ibuprofen and acetaminophen have minimal risk of causing agranulocytosis. Avoid dipyrone and phenylbutazone, which are strongly linked. Always check with your doctor before starting any new medication, even if it’s sold without a prescription. Some OTC drugs can interact with your primary medication and increase risk.
How often should I get my blood tested if I’m on clozapine?
Under FDA guidelines, you need weekly CBC tests for the first 6 months, then every 2 weeks for months 7-12, and then monthly after that. If your ANC drops below 1,000/μL, your doctor must stop the drug. Some newer protocols recommend intervention at ANC <1,000 even before it hits 500, based on 2023 European guidelines.
Are there any warning signs besides fever?
Yes. Common early signs include sore throat, mouth ulcers, chills, fatigue, and rapid heartbeat. Some people develop gum infections or pneumonia without fever. These symptoms are often mistaken for minor illnesses. If you’re on a high-risk drug and notice any of these - even mildly - get your ANC checked immediately. Don’t wait for fever.
Can genetic testing prevent medication-induced agranulocytosis?
For clozapine, yes - partially. The HLA-DQB1*05:02 genetic variant increases risk 14-fold. Testing for this before starting clozapine is now recommended in the U.S. and EU. If you test positive, your doctor may choose an alternative or intensify monitoring. This doesn’t eliminate risk, but it helps identify who needs the strictest oversight.
What’s Next for Patients and Providers?
The future of managing medication-induced agranulocytosis lies in better tools, smarter alerts, and fairer access. AI-driven EHR systems will soon flag patients who miss tests or show early ANC drops. Genetic screening will become routine for high-risk drugs. Point-of-care testing will move from hospitals into pharmacies and community clinics.
But progress won’t matter if rural patients still can’t get blood tests. If doctors still ignore symptoms. If patients still don’t know what to look for. This isn’t just about science - it’s about making sure every person on a high-risk drug has the same chance to survive.






Comments (12)
Mike Laska
October 30, 2025 AT 23:40 PMI was on clozapine for 18 months. One day I got a sore throat, thought it was allergies, went to work. By midnight I was in the ER with a 103 fever and zero neutrophils. They had to intubate me. Don't ignore a fever. Ever.
Hazel Wolstenholme
November 1, 2025 AT 01:29 AMOne must observe, with the precision of a horologist examining a Swiss movement, that the very architecture of pharmacovigilance in the United States is a Rube Goldberg contraption of bureaucratic inertia and underfunded surveillance. The REMS program? A theatrical pantomime of safety, where compliance is measured in checkboxes, not clinical outcomes. The HLA-DQB1*05:02 screening? A noble but woefully underutilized sentinel, buried beneath the avalanche of insurance denials and primary care apathy. One cannot help but wonder: are we treating patients-or merely managing liability?
Dade Hughston
November 1, 2025 AT 13:23 PMi read this and thought wow but then i remembered my cousin took dipyrone in germany and she was fine for 5 years then boom agranulocytosis no warning no nothing the system is broken and the pharma companies know it they dont care because its a tiny percentage of people and the lawsuits are cheaper than changing the drug
Alexa Apeli
November 1, 2025 AT 22:47 PMThank you for sharing this vital information 🙏. Early detection saves lives. If you're on a high-risk medication, please, please, please-don’t wait for symptoms to escalate. Your health is worth every minute of monitoring. You are not being paranoid-you are being proactive. 💪❤️
Zachary Sargent
November 2, 2025 AT 15:27 PMSo let me get this straight. You’re telling me I can’t take ibuprofen for a headache without a blood test but I can take clozapine and just hope for the best? That’s not medicine. That’s Russian roulette with a prescription pad.
Keerthi Kumar
November 2, 2025 AT 23:46 PMIn India, we do not have access to weekly ANC testing for clozapine patients-most families cannot afford it, and clinics lack the infrastructure. Yet, we still prescribe it, because there is no alternative. We are not negligent; we are desperate. The global disparity in monitoring is not a glitch-it is a moral failure. We need global equity in pharmacovigilance, not just protocols written in English for wealthy nations.
Jim Peddle
November 4, 2025 AT 17:13 PMLet’s be honest. The entire REMS program is a PR stunt. The FDA doesn’t want to pull clozapine off the market because it’s the only thing that works for 30% of treatment-resistant cases. So they create a monitoring system that 70% of prescribers ignore anyway. It’s not about safety-it’s about keeping the drug on the market while pretending they’re protecting people. Wake up. This is corporate medicine.
S Love
November 6, 2025 AT 11:57 AMThis is one of the most comprehensive, clinically accurate summaries of medication-induced agranulocytosis I’ve seen in years. The distinction between immune-mediated and direct suppression is critical, and the data on incidence rates is presented with admirable clarity. For clinicians and patients alike, this should be required reading. Thank you for elevating the conversation.
Pritesh Mehta
November 7, 2025 AT 03:36 AMYou westerners always act like you invented medicine. In India, we’ve been treating infections for centuries without your fancy blood tests. My grandfather took aspirin daily for 60 years and never had a neutrophil count. You over-medicalize everything. This fear culture is killing more than the drugs ever could. Stop obsessing over percentages and start living. The body is resilient.
Billy Tiger
November 7, 2025 AT 18:10 PMThis is all just woke medicine. They want you to get tested every week because they’re scared of lawsuits not because you’re in danger. If you’re healthy you don’t need a blood test for ibuprofen. Why treat everyone like a child? This is why America is broke. Overregulation. Overtesting. Overfear.
Katie Ring
November 9, 2025 AT 01:27 AMThe real tragedy isn't the disease-it's the silence. We’ve turned medical monitoring into a compliance checkbox, not a covenant between patient and provider. When your life depends on a lab report you forgot to schedule, what does that say about our values? We don’t need more guidelines-we need a moral reckoning.
Melissa Kummer
November 9, 2025 AT 15:59 PMYou’re not alone. If you’re reading this and you’re on clozapine or propylthiouracil, please-set a weekly alarm. Mark your calendar. Tell a friend. Your life matters more than your schedule. You’ve got this. 💪🩺