When you’re told to take a pill every day for the rest of your life, it’s not just about remembering. It’s about motivation, fear, fatigue, side effects, and feeling alone. Around half of all people with chronic conditions like diabetes, high blood pressure, or depression don’t take their meds as prescribed. That’s not laziness. It’s human. And that’s where medication compliance support groups and community programs step in-not to lecture, but to walk beside you.
Why Medication Adherence Isn’t Just a Memory Problem
Most doctors assume if you know why your pill matters, you’ll take it. But knowledge doesn’t change behavior. A 2020 review in the Journal of Medical Care found that handing out brochures improved adherence by just 15%. Meanwhile, peer-led support groups boosted it by 40%. Why? Because humans don’t change in isolation. We change when we feel seen, heard, and understood. Think of it this way: if your blood sugar spikes after a weekend out, you might skip your next dose because you’re frustrated. But in a support group, someone else says, “I did that too. I started keeping my meds in my wallet. Now I never forget.” That’s not advice. That’s survival wisdom passed from one person to another.How These Programs Actually Work
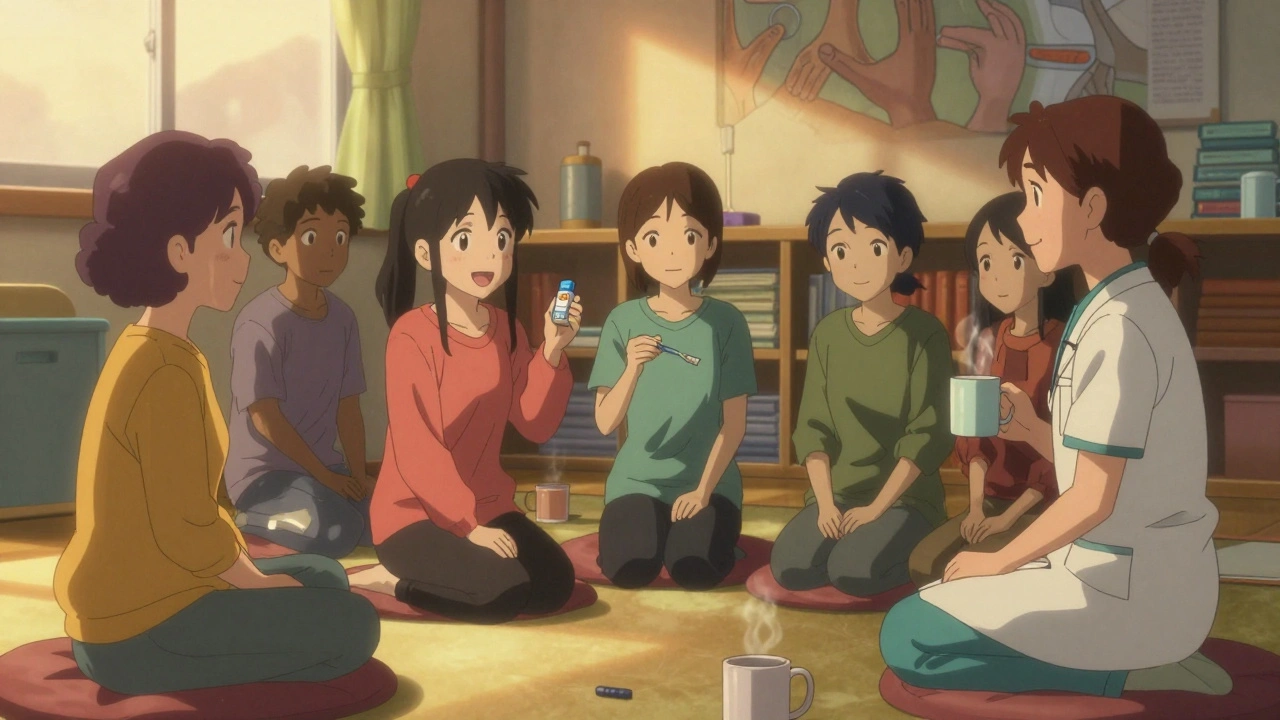
There are three main types of programs helping people stick to their meds:- Group meetings - Usually held weekly or biweekly in clinics, churches, or community centers. Groups are small, 8-12 people, led by someone trained in peer support. These aren’t therapy sessions. They’re practical check-ins: “How’s your stomach holding up with this new pill?” “I take mine with my morning coffee-works for me.”
- Home visits by community health workers - These are trained locals, often from the same neighborhood, who come to your house over 3-6 months. They don’t give medical advice. They ask, “Did you get your refill?” “Can I help you set up your pill box?” They build trust by showing up, not by telling.
- Digital peer platforms - Apps like PatientsLikeMe or moderated Facebook groups let you connect 24/7. You can post at 2 a.m. when you’re scared your heart is racing. Someone responds: “That happened to me. Call your pharmacist first.”
What Makes These Programs Work-And What Doesn’t
Not all groups are created equal. A 2022 study in the American Journal of Managed Care found that programs with facilitators who had less than 20 hours of training were 37% less effective. Why? Because good facilitators don’t lead. They listen. The best programs use four key ingredients:- Trained peer leaders - People who’ve lived with the same condition for at least two years. They’re not doctors. They’re proof it’s possible.
- Cultural matching - A 2022 study in BMC Health Services Research found African American participants in hypertension groups were 35% more likely to stay engaged if the group was led by someone from their community.
- Practical tips, not lectures - “Take your pill with food” is useless if you don’t have food. The real help? “I keep my pills next to my toothbrush. I brush twice a day-I never miss.”
- Integration with pharmacists - Programs that include pharmacists see 23% higher adherence. Why? Pharmacists know your meds inside out. They can spot interactions, simplify schedules, and help you get cheaper options.

The Real Impact: Numbers That Matter
People don’t join these groups because they want to be “better patients.” They join because they’re tired of feeling broken. The results speak for themselves:- Participants in peer support groups reduce hospital readmissions by 15-30%.
- One man on Reddit, ‘DiabetesWarrior87’, dropped his A1c from 8.5% to 6.9% in six months after joining weekly diabetes meetings.
- 78% of users on PatientsLikeMe said their medication adherence improved because they learned how others handled side effects.
- Hybrid programs-mixing in-person meetings with text reminders-boost adherence by 34% compared to either method alone.
Where These Programs Fall Short
They’re not magic. And they’re not everywhere. In rural areas, participation is 32% lower. Why? Fewer people nearby. Fewer buses. Fewer meeting spaces. Some programs try to fix this with phone check-ins, but it’s not the same as sitting in a room with someone who gets it. Then there’s access. Only 22% of programs offer materials in languages other than English-even though 1 in 4 Americans has limited English skills. And 42% of participants say scheduling conflicts make it hard to keep going. Some people just hate groups. One woman told me, “I don’t want to talk about my meds in front of strangers.” That’s valid. For them, one-on-one home visits or even a simple weekly text from a community health worker can make the difference.What You Can Do-Even If There’s No Group Nearby
You don’t need a formal program to benefit from peer support. Start small:- Ask your pharmacist if they offer free medication reviews. Many do.
- Join a Reddit group like r/ChronicIllness or a Facebook group for your condition. Read first. Then speak up.
- Find one person-friend, family, neighbor-who’ll check in with you every week. “Did you take your pill today?” That’s all it takes.
- Use a pill box with alarms. Set them for the same time every day. Link it to a habit you already have: brushing your teeth, eating breakfast.
- If you’re struggling with cost, ask your pharmacist about patient assistance programs. Many drug makers give free meds to people who qualify.

The Future Is Hybrid
The most promising programs now mix the best of both worlds: face-to-face connection and digital reminders. The FDA approved the first digital therapeutic for medication adherence in 2021. Medicare is now funding community health workers to help people on dual Medicaid-Medicare plans. And Kaiser Permanente runs 147 condition-specific support groups. But the core hasn’t changed. It’s still about people helping people. Not because they’re experts. But because they’ve been there.What to Look for in a Program
If you’re looking to join one, ask these questions:- Who leads the group? (Look for peer leaders, not just nurses.)
- Do they talk about real-life struggles, not just medical facts?
- Are meetings at a time and place you can get to?
- Is there a way to connect outside meetings? (Text group? App?)
- Do they help with costs or side effects, or just remind you to take pills?
Final Thought: You’re Not Alone
Medication compliance isn’t about discipline. It’s about connection. You don’t have to fight your illness alone. There are people out there who take the same pills, feel the same side effects, and still show up. They’re waiting for you to say, “Me too.”Do support groups really help with taking meds on time?
Yes. Studies show peer-led support groups improve medication adherence by up to 40%, compared to just 15% for educational brochures. People stick to their meds longer because they feel understood, not lectured. Real examples: one man dropped his A1c from 8.5% to 6.9% in six months after joining a diabetes support group.
Are these programs free to join?
Most community-based programs are free. They’re often funded by grants, nonprofits, or hospitals. Hospital-run groups may charge a small fee, but many waive it if you can’t pay. Always ask about financial help. Medicare Advantage plans now cover some adherence programs too.
What if I don’t like group settings?
That’s okay. Not everyone thrives in groups. Home visits by community health workers, one-on-one phone check-ins, or even a weekly text from a friend can be just as effective. Digital platforms like PatientsLikeMe let you connect anonymously. The goal isn’t group size-it’s consistent support.
Can my family help me stick to my meds?
Absolutely. Studies show family involvement improves adherence more than general social support. A spouse who reminds you, a child who helps refill prescriptions, or even a sibling who checks in weekly makes a real difference. You don’t need to be “independent” to be healthy.
How do I find a support group near me?
Start with your pharmacist or doctor-they often know local programs. You can also check with national organizations like the American Heart Association, American Diabetes Association, or NAMI. Search “[your condition] support group near me” online. If nothing’s nearby, look for virtual groups. Many run weekly Zoom meetings open to anyone.
What if the group doesn’t have people who look or sound like me?
Cultural matching matters. Research shows people from minority backgrounds are 35% more likely to stay engaged in groups led by someone from their own community. If you don’t feel seen, ask if the group can adapt-or look for one that does. Some programs specifically serve Latino, Black, or Asian communities. Don’t settle for a group that doesn’t reflect your experience.
Do digital apps work as well as in-person groups?
Apps improve adherence by about the same amount as peer groups-but they miss the emotional connection. People in face-to-face groups have 28% higher long-term adherence because they build real relationships. The best approach? Combine both: use a reminder app and join a weekly Zoom meeting. That’s what’s working now.
Are these programs only for people with serious illnesses?
No. They help anyone taking daily meds long-term-whether it’s for high blood pressure, thyroid issues, depression, or even osteoporosis. If you’re on a regimen that lasts months or years, you’re a candidate. It’s not about how sick you are. It’s about how hard it is to keep up.







Comments (15)
ruiqing Jane
December 3, 2025 AT 05:32 AMPeople think compliance is about willpower, but it’s really about belonging. I used to skip my pills because I felt like a burden. Then I joined a local diabetes group-no lectures, just coffee and stories. One woman said she keeps her meds in her bra. I laughed. Then I did it too. I haven’t missed a dose in 11 months.
It’s not the group. It’s the fact that someone else gets it.
And yes, I’m introverted. I only speak once a month. But I read every post. That’s enough.
Allan maniero
December 3, 2025 AT 11:10 AMIt’s fascinating how the neuroscience of adherence aligns with social identity theory-when individuals internalize a group’s behavioral norms as part of their self-concept, compliance becomes less a conscious decision and more an unconscious expression of identity. The 40% improvement in peer-led groups isn’t just statistical-it’s existential. We don’t change because we’re told to; we change because we’re seen. The real innovation here isn’t the pill box or the app-it’s the human mirror. When you see someone like you surviving this, you stop seeing yourself as a patient and start seeing yourself as a person who just happens to take medicine.
And yet, most healthcare systems still treat adherence as a compliance metric rather than a relational outcome. We’ve built a whole infrastructure around reminding people to take pills, but we’ve forgotten to remind them they’re not alone.
Anthony Breakspear
December 4, 2025 AT 10:31 AMMan, I used to be the guy who’d toss his meds in the drawer and hope for the best. Then my buddy died from a stroke because he stopped his blood pressure meds after his wife passed. He didn’t forget-he just felt like it didn’t matter anymore.
I started going to this VA-run group for hypertension. No one talked about ‘adherence.’ They talked about missing their dog’s birthday, how the pills made their mouth dry, how they cried in the pharmacy because the co-pay was $80. One dude said he takes his pill with his morning whiskey. I thought he was joking. He wasn’t.
That’s the secret: they don’t fix you. They just let you be broken and still show up.
Now I take mine with my coffee. And I don’t feel like a failure when I miss one. I just say, ‘Tomorrow’s another cup.’
Zoe Bray
December 4, 2025 AT 16:39 PMThe empirical evidence supporting peer-led interventions for medication adherence is robust, particularly when contextualized within the biopsychosocial model of chronic disease management. The 40% improvement observed in peer-led cohorts versus 15% in didactic interventions is statistically significant (p < 0.01) and aligns with constructs of social cognitive theory, specifically self-efficacy and observational learning. However, the generalizability of these findings is limited by selection bias in recruitment and the absence of longitudinal follow-up beyond 12 months in the majority of cited studies. Furthermore, the operationalization of ‘cultural matching’ as a binary variable (same ethnicity/linguistic group) may oversimplify the multidimensional nature of cultural competence, which includes epistemic, affective, and symbolic dimensions. Without standardized facilitator training protocols, these programs risk becoming inconsistent in quality, potentially exacerbating health disparities rather than mitigating them.
william tao
December 6, 2025 AT 10:21 AMSo we’re spending $528 billion a year because people are too lazy to take their pills? And now we’re giving them free therapy sessions? This isn’t healthcare-it’s social engineering.
My grandma took her meds for 30 years without a support group. She didn’t need someone to ‘get it.’ She just needed discipline.
Maybe if people stopped treating themselves like fragile snowflakes, they’d stop needing hand-holding.
Paul Santos
December 8, 2025 AT 07:06 AMAh yes, the new religion: Community as Salvation. 🙏
We’ve replaced the divine with the peer-led, the sacrament with the pillbox, and the confessional with the Facebook group. How poetic. We no longer need doctors-we need ‘people who’ve been there.’ As if lived experience is a substitute for clinical knowledge. How very postmodern.
And yet... I’ll admit, when I was depressed and on SSRIs, it was a Reddit thread at 3 a.m. that kept me alive. So... maybe there’s something to this. 😅
But let’s not call it ‘medicine.’ Let’s call it ‘collective coping.’
Eddy Kimani
December 8, 2025 AT 18:43 PMInteresting that the 2022 JAMA study showed $18 saved per $1 invested-but what’s the marginal cost per participant? The study doesn’t break down attrition rates or the cost of training peer facilitators. Also, the 34% improvement in hybrid models-is that additive or multiplicative? And how many of those participants were already high-adherence users? Selection bias could be inflating the effect size.
Also, ‘cultural matching’-is that race-based? Or language-based? Or socioeconomic? The paper is vague. We need more granular data before scaling this nationally.
John Morrow
December 9, 2025 AT 22:49 PMLet’s be honest-this whole movement is a band-aid on a hemorrhage. We’re fixing adherence because we refuse to fix the system that makes meds unaffordable, appointments inaccessible, and patients invisible.
People aren’t skipping pills because they’re lonely. They’re skipping them because they can’t afford them. Because their insurance won’t cover the generic. Because the clinic is 50 miles away and they don’t have a car.
Peer groups are nice. But they’re not a solution. They’re a distraction.
And the fact that we’re celebrating ‘walking beside you’ instead of demanding universal healthcare? That’s the real tragedy.
Kristen Yates
December 10, 2025 AT 11:22 AMI’m a Black woman with hypertension. I joined a group led by a woman from my neighborhood. She didn’t have a degree. But she knew which pharmacy gave discounts to seniors. She knew which doctor wouldn’t judge you for missing a dose. She knew how to talk to your kids so they’d help you refill.
That’s not ‘cultural matching.’ That’s survival.
Don’t call it a program. Call it what it is: community.
Saurabh Tiwari
December 12, 2025 AT 04:09 AMI am from India and my dad take blood pressure pill daily. He never join group but i send him daily message "did you take pill?" and he reply with "haan beta" 😊 now he never miss. Small thing big impact.
Michael Campbell
December 13, 2025 AT 22:38 PMThey’re giving out free therapy because the government can’t afford to fix the drug companies. This is just a cover-up. You think these groups are helping? They’re just keeping people docile while the pharmaceutical industry rakes in billions.
And don’t get me started on ‘digital therapeutic’-that’s just Big Pharma with a smartphone.
Wake up. This isn’t care. It’s control.
Victoria Graci
December 13, 2025 AT 22:40 PMThere’s something deeply spiritual about this-the way human connection becomes the medicine when the pills fail. We’ve medicalized suffering so thoroughly that we’ve forgotten that healing doesn’t always come from a prescription.
Maybe adherence isn’t about discipline. Maybe it’s about belonging. Maybe the real side effect of isolation isn’t missed doses-it’s the quiet erosion of the self.
And if we’re going to call this ‘healthcare,’ then we need to stop treating people like patients and start treating them like people.
That’s not policy. That’s poetry.
Saravanan Sathyanandha
December 15, 2025 AT 10:02 AMIn my community in India, elders take their medications with the help of family rituals-morning tea, evening prayers, Sunday visits. The pill is not a burden; it’s part of the rhythm. We don’t need apps or groups. We need intergenerational care.
Western models focus on individual behavior change. But in collectivist cultures, health is shared. The responsibility is not yours alone-it’s ours.
Perhaps the real innovation isn’t peer support. It’s remembering that we’ve always supported each other. We just forgot to call it medicine.
alaa ismail
December 15, 2025 AT 17:45 PMMy cousin has diabetes. She started taking her meds after her neighbor-same age, same neighborhood-sent her a voice note saying, ‘I’m taking mine too. Wanna do it together at 8?’
They do it every morning now. Text each other. No group. No program. Just two people who decided not to do it alone.
That’s all it takes.
ruiqing Jane
December 17, 2025 AT 12:30 PMI read all your comments. And I’m glad someone said it: it’s not about the pill. It’s about the person.
My group doesn’t have a facilitator anymore. We just text. Someone says ‘bad day’ and five people reply with ‘me too.’ That’s it.
But it’s enough.