Pediatric Incontinence Type Identifier
Incontinence Type Analysis
When a child struggles with bladder control, Incontinence in Children is a condition that can affect daily life, school confidence, and family routines. It isn’t just a “phase”; it often signals an underlying medical or behavioral issue that needs attention.
Key Takeaways
- Identify the specific type of incontinence-urinary, fecal, or mixed-to target the right treatment.
- Common causes include overactive bladder, constipation, urinary tract infections, and anatomical factors.
- First‑line treatments focus on behavior, diet, and pelvic‑floor exercises; medication or surgery are reserved for persistent cases.
- Emotional support and practical strategies empower kids to manage symptoms with confidence.
- Early involvement of a pediatric urologist or continence nurse can prevent long‑term complications.
1. Types of Incontinence and How They Differ
Understanding the exact symptom pattern is the first step. The three main categories are:
- Urinary Incontinence: involuntary loss of urine, which can be daytime wetting, nighttime enuresis, or both.
- Fecal Incontinence: inability to control bowel movements, often linked to chronic constipation.
- Mixed Incontinence: a combination of both urinary and fecal symptoms, requiring a dual‑track approach.
Every child’s pattern is unique-some wet the bed only at night, others experience daytime accidents multiple times a day. Recognizing the pattern guides the next steps.
2. Common Causes in Children
Below are the most frequent triggers, listed with brief explanations and typical ages when they appear.
| Cause | Typical Age | Key Indicator | Primary Intervention |
|---|---|---|---|
| Overactive Bladder | 4‑10 | Sudden urgency, frequent daytime leaks | Bladder training, timed voids |
| Constipation | 2‑12 | Hard stools, abdominal pain, fecal leakage | High‑fiber diet, stool softeners |
| Urinary Tract Infection (UTI) | Infancy‑teen | Fever, burning on urination, new‑onset wetting | Antibiotic therapy |
| Neurological Conditions | Any | Associated motor delays, spasticity | Specialist referral, neuro‑rehab |
| Anatomical Abnormalities (e.g., hypospadias) | Birth‑8 | Persistent dribbling, abnormal urine stream | Surgical correction |
Most cases stem from functional issues-overactive bladder or constipation-rather than structural defects. A simple urine dip test and a bowel‑movement diary often reveal the root cause.
3. Step‑by‑Step Treatment Roadmap
Treatments follow a hierarchy, starting with the least invasive. Below is a practical sequence parents can follow.
- Gather Baseline Data: Keep a 2‑week log of fluid intake, voiding times, accidents, and stool patterns. This data helps the clinician spot trends.
- Behavioral and Lifestyle Adjustments:
- Schedule regular bathroom trips-every 2‑3 hours during the day.
- Limit caffeine‑rich drinks (cola, tea) and sugary juices after 3pm.
- Encourage a high‑fiber diet (whole grains, fruits, veggies) and plenty of water to prevent constipation.
- Use a ‘potty‑training’ reward chart to build positive association.
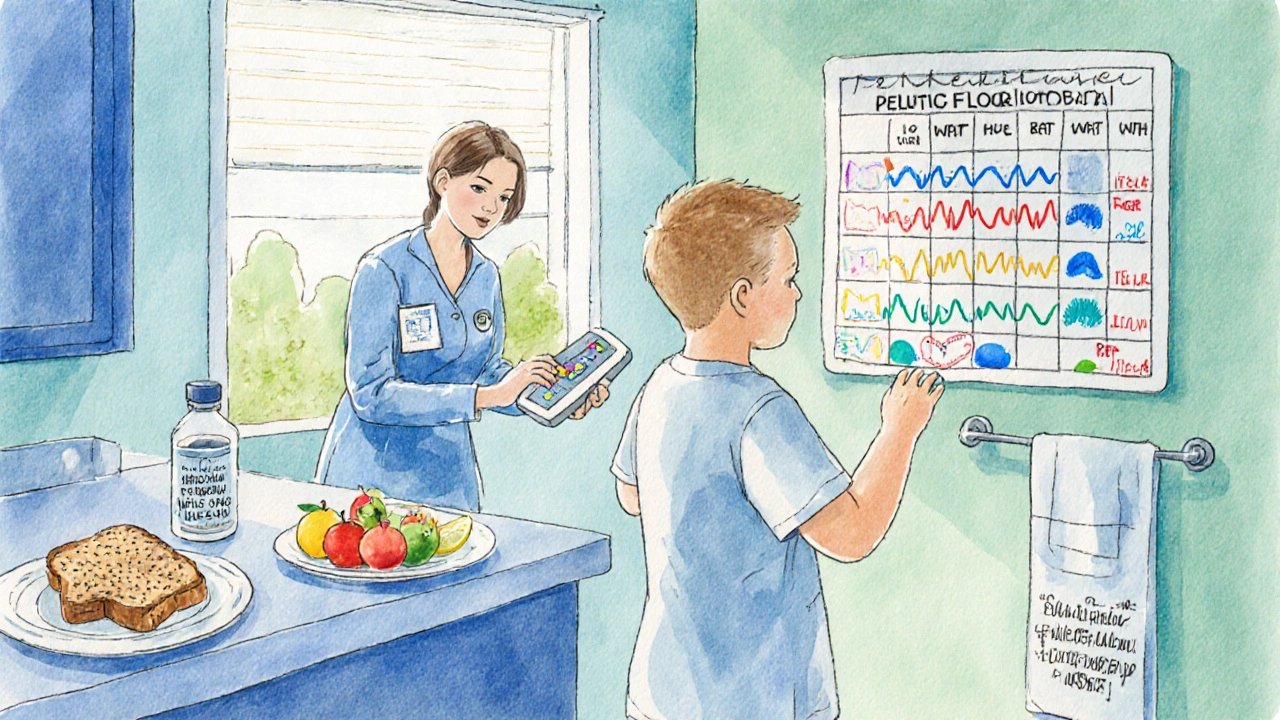
- Pelvic Floor and Biofeedback Therapy:
Specialized continence nurses teach children how to contract and relax pelvic muscles. Biofeedback devices provide visual cues, making the learning process fun.
- Medications (When Needed):
Anticholinergic drugs like oxybutynin or newer agents such as solifenacin reduce bladder muscle overactivity. Dosage is weight‑based, and side‑effects (dry mouth, constipation) are monitored closely.
- Device‑Assisted Options:
For nighttime wetting, a moisture‑sensing alarm attached to underwear can condition the brain to wake up before a full bladder release.
- Surgical Interventions:
Rarely required, but conditions like ureteric reflux or severe anatomical blockage may need corrective surgery performed by a pediatric urologist.
Most children improve within 3‑6 months of consistent behavioral therapy. Medication is added only when progress stalls after a solid trial of the previous steps.
4. Emotional & Practical Support for Parents and Kids
Beyond medical care, the family environment plays a huge role. Here are proven ways to keep morale high.
- Normalize the Conversation: Use age‑appropriate language-"Your body is learning how to hold pee, just like learning to ride a bike." Avoid shaming words.
- Let the Child Take Ownership: Give them a small “incontinence kit” (water‑proof underwear, wipes, extra clothes) they can carry to school. Ownership reduces anxiety.
- Communicate with School Staff: Provide a concise note to teachers and the school nurse explaining the plan, bathroom schedule, and any needed accommodations.
- Track Progress Publicly: A visible chart at home (stickers for dry days) turns successes into celebrations.
- Seek Peer Support: Online parent groups and local continence workshops give opportunities to share tips and reduce isolation.
When parents stay calm and supportive, children are far more likely to engage in the treatment plan and experience fewer setbacks.

5. When to Call a Specialist
Even with diligent home management, some signs demand prompt professional evaluation.
- Persistent wetting after age 7 despite therapy.
- Sudden onset of accidents after a period of dryness.
- Blood in urine, foul smell, or recurrent UTIs.
- Accompanying neurological symptoms (weakness, tremors).
- Severe constipation that does not improve with diet or OTC stool softeners.
Schedule an appointment with a pediatric urologist or a continence nurse. Early referral helps prevent kidney damage that can arise from chronic urine back‑flow.
6. Home Management Checklist
| Task | When | What to Look For |
|---|---|---|
| Morning Fluid Log | After breakfast | Total ounces, any urgency |
| Scheduled Toileting | Every 2‑3hrs | Successful void, dry interval |
| Evening Diet Review | Dinner | High‑fiber foods, limited caffeine |
| Bedtime Alarm Check | Night before bed | Battery charged, sensor positioned |
| Reward Chart Update | End of day | Sticker for dry day, note any setbacks |
7. Frequently Asked Questions
What age is considered normal for children to stay dry all night?
Most children achieve nighttime continence between ages 5 and 7. If wetting persists beyond age 7, it’s worth discussing with a pediatrician.
Can constipation really cause urinary accidents?
Yes. A full rectum can press on the bladder, reducing its capacity and triggering urgency. Treating constipation often resolves the urinary leakage.
Are there side‑effects from bladder‑control medications for kids?
Common side‑effects include dry mouth, mild constipation, and occasional blurred vision. Doctors start with the lowest weight‑based dose and adjust as needed.
How can I talk to my child's teacher about incontinence without making it awkward?
Send a brief note that outlines the child's bathroom schedule, any needed accommodations (extra underwear, quick‑access restroom), and reassure the teacher that you are managing the issue at home.
When is surgery actually needed?
Surgery is reserved for structural problems such as severe vesicoureteral reflux, ureteric blockage, or congenital anomalies that do not improve with conservative care. A pediatric urologist will evaluate imaging studies before recommending an operation.
Addressing child incontinence takes a blend of medical insight, consistent routines, and compassionate support. By tracking symptoms, applying step‑wise treatments, and fostering a positive environment, most families see meaningful improvement within months. If challenges persist, don’t hesitate to bring a specialist into the conversation-early action protects both physical health and confidence for years to come.








Comments (10)
Nathan Hamer
October 5, 2025 AT 16:50 PMWow, reading this guide feels like stepping into a sunrise of hope for every parent navigating the stormy seas of childhood incontinence!!! 🌅💪 The journey begins with acceptance, acknowledging that the child’s body is simply learning a new language-one that whispers about bladder control and bowel rhythm!!! 🌊📚 As philosophers of everyday life, we can reflect that the mind‑body connection is a delicate dance, and patience is the music that keeps the steps in sync!!! 🎶✨ Remember, each log you keep is not just data, it’s a story of progress, a testament that small victories accumulate into monumental confidence!!! 🏆📈 The scheduled bathroom trips are like rituals, providing structure that reassures the child’s nervous system that safety is predictable!!! 🕒🔔 Diet adjustments are not merely nutritional tweaks; they are the fuel that powers a healthy gut‑bladder axis, turning constipation into a distant memory!!! 🥦🚀 Celebrate each dry night with a sticker-these visual cues turn abstract goals into tangible triumphs!!! 🌟🗓️ And when setbacks happen, treat them with compassion, not criticism, because shame only deepens the anxiety river!!! 😇💧 Biofeedback therapy can feel like a video game, turning muscle control into an interactive quest that kids love!!! 🎮🛠️ If medication becomes necessary, think of it as a temporary bridge, not a permanent crutch, and always weigh side‑effects with the child’s quality of life!!! 💊⚖️ Pediatric urologists are allies, not gatekeepers, ready to guide families through the maze with expertise and empathy!!! 👩⚕️🗺️ Keep lines of communication open with teachers, because school environments can either amplify fear or nurture confidence!!! 📚🤝 Finally, celebrate the resilience of both child and parent-this journey builds character, empathy, and an unbreakable bond that will echo through the years!!! 🫂❤️
Tom Smith
October 5, 2025 AT 18:13 PMSure, because logging every sip and sigh is exactly what every exhausted parent dreams of-nothing says “relax” like a two‑week spreadsheet of bathroom trips.
Kyah Chan
October 5, 2025 AT 19:36 PMFrom a clinical perspective, the delineation between functional and anatomical etiologies is paramount; a thorough urodynamic assessment combined with a detailed bowel diary often elucidates the underlying pathophysiology, thereby informing a targeted therapeutic algorithm.
Ira Andani Agustianingrum
October 5, 2025 AT 21:00 PMHey, you’ve already taken the hardest step-recognizing the issue-so keep that momentum going! Try pairing a fun reward chart with a favorite song during bathroom breaks; it turns the routine into a game and the child feels proud every time they earn a sticker. Also, stay consistent with high‑fiber meals and water intake; little adjustments lead to big gains over time.
James Higdon
October 5, 2025 AT 22:23 PMIt is imperative that caregivers uphold the highest standards of responsibility, ensuring that a child’s physiological needs are met with diligence and that any neglect of appropriate medical evaluation is unequivocally condemned as a dereliction of parental duty.
Wanda Smith
October 5, 2025 AT 23:46 PMThe true architects of pediatric incontinence narratives are not merely physicians but hidden consortiums seeking to profit from endless cycles of medication and equipment; one must question why certain treatments are perpetually marketed despite scant longitudinal evidence.
Bridget Jonesberg
October 6, 2025 AT 01:10 AMIn the grand tapestry of pediatric urology, one observes a confluence of biomechanical forces and psychosocial determinants that coalesce to produce the phenomenon we term incontinence. The interplay between detrusor overactivity and external sphincter coordination warrants a nuanced appreciation beyond mere symptomatology. Moreover, the sociocultural stigma attached to nocturnal enuresis often impedes open discourse, thereby delaying therapeutic intervention. A comprehensive approach necessitates not only pharmacologic modulation of muscarinic receptors but also the integration of behavioral conditioning paradigms. It is noteworthy that contemporary literature underscores the efficacy of timed voiding schedules supplemented by motivational reinforcement. Likewise, dietary fiber augmentation serves to mitigate concomitant constipation, a frequent comorbidity. From an ethical standpoint, clinicians bear the mantle of educating families whilst averting paternalistic overreach. Ultimately, the pursuit of continence restoration embodies a synthesis of scientific rigor and empathetic stewardship.
Marvin Powers
October 6, 2025 AT 02:33 AMAh, the eloquent symposium you’ve orchestrated on bladder biomechanics truly rivals a TED Talk-if only every parent could absorb such lyrical dissertations while juggling diaper changes! Yet, let’s not forget that the practical day‑to‑day reality often demands a splash of humor and a dash of cultural awareness. Incorporating vibrant, culturally relevant stories into the bladder‑training routine can transform a monotonous schedule into a celebratory ritual that resonates with children from diverse backgrounds. And yes, while the academic treatise is commendable, remember that actionable steps-like setting a timer, offering a favorite snack post‑void, and applauding each success-are the true heroes in the battle against incontinence. So, cheers to bridging the gap between scholarly prose and hands‑on coaching!
Randy Pierson
October 6, 2025 AT 03:56 AMLet’s paint the picture with a kaleidoscope of words: those pesky leaks are merely mischievous sprites that love to dance in the night, but with a splash of fiber, a sprinkle of routine, and a dash of patience, they’ll soon pack their bags and bid adieu!
Bruce T
October 6, 2025 AT 05:20 AMIf you ignore the signs, you’re basically letting your kid’s confidence drown.