Steroid Myopathy Assessment: Timed Chair Rise Test
How to Perform the Test
Stand up from a standard chair without using your hands. Repeat this 5 times as quickly as possible. Time your total time using a stopwatch or timer.
According to medical studies, if your time for 5 chair rises exceeds 10 seconds, it may indicate steroid myopathy. This test is one of the most reliable early detection methods for steroid-induced muscle weakness.
What Your Results Mean
The timed chair rise test is a simple functional assessment that helps identify steroid myopathy early. The key threshold is 10 seconds for 5 repetitions.
- Normal Under 10 seconds: Your muscle function appears normal for the chair rise test
- Mild Weakness 10-15 seconds: Indicates early muscle weakness that may be steroid myopathy
- Significant Weakness Over 15 seconds: Suggests more advanced muscle weakness requiring medical attention
Next Steps
If your results indicate weakness:
- Discuss results with your doctor
- Ask about a referral to a physical therapist experienced with steroid myopathy
- Consider starting a supervised resistance training program
- Track your progress with regular chair rise tests
When you're on long-term steroids for asthma, rheumatoid arthritis, or another chronic condition, you might notice something strange: you can't stand up from a chair without using your arms. Climbing stairs feels impossible. Lifting your arms to brush your hair becomes a struggle. And here's the kicker - there's no pain. Just pure, silent weakness. This isn't just being out of shape. It's steroid myopathy, a hidden side effect that affects up to 21% of people on chronic steroid therapy.
What Is Steroid Myopathy?
Steroid myopathy is muscle weakness caused by corticosteroids like prednisone, dexamethasone, or cortisone. It's not an infection. It's not inflammation. It's a direct toxic effect on your muscles. First noticed back in the 1930s in patients with Cushing syndrome, it's now one of the most common drug-related muscle problems in the world. The World Health Organization estimates that as the population ages and more people rely on long-term steroids, cases will rise by 12-15% over the next decade.The problem starts when steroids bind to receptors inside muscle cells. This triggers two damaging processes: it ramps up muscle breakdown (catabolism) and shuts down muscle building (anabolism). Fast-twitch muscle fibers - the ones you use to stand up, climb stairs, or lift things - are the first to shrink. And unlike other muscle diseases, there's no swelling, no pain, no elevated enzymes in your blood. That’s why it’s so easy to miss.
How to Spot the Signs Early
Most people don’t realize they have steroid myopathy until they can’t get out of a low chair. That’s not normal. Here’s what to watch for:- Difficulty rising from a seated position without pushing off with your hands
- Needing a handrail to climb stairs
- Struggling to lift your arms above shoulder height
- Feeling like your legs are “heavy” or “wooden”
- No muscle pain or cramping - just weakness
These aren’t vague complaints. They’re clinical red flags. A 2019 study in Muscle & Nerve found that 78% of patients on steroids had measurable strength loss - even when their doctor’s manual muscle test said they were fine. That’s because standard exams miss early changes. You need objective tests.
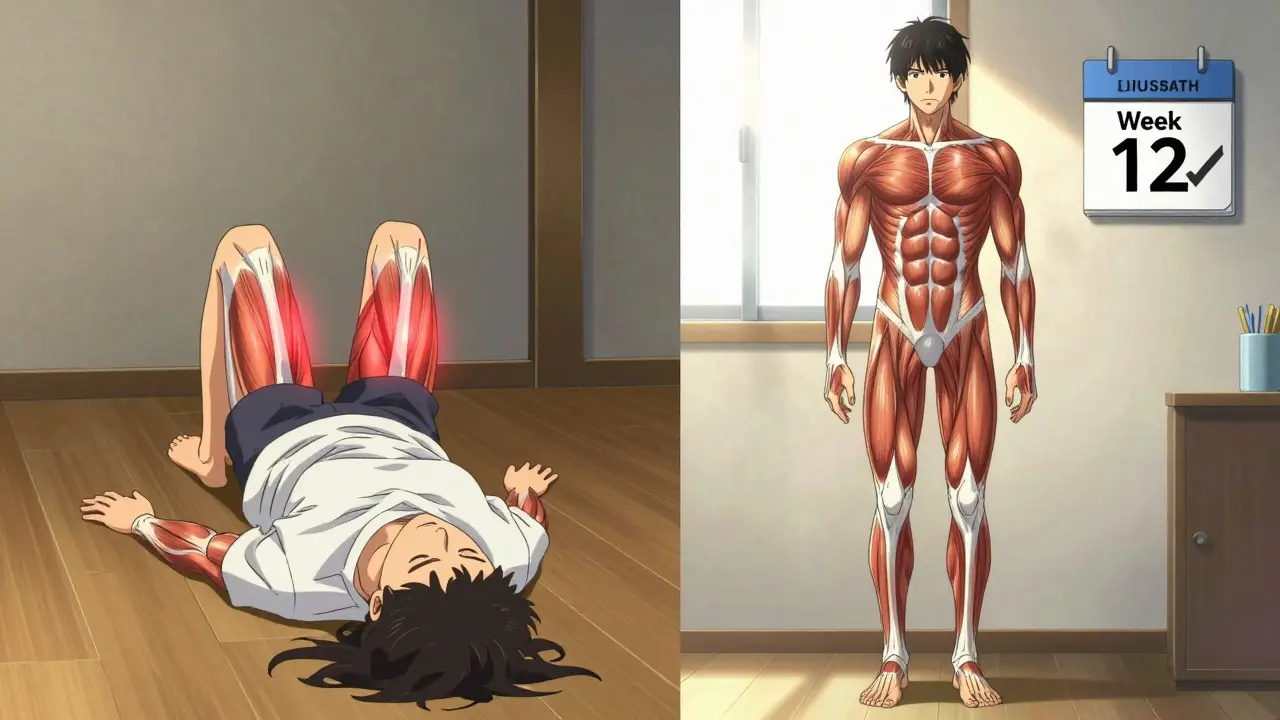
The timed chair rise test is one of the most reliable. Try standing up from a standard chair five times without using your arms. If it takes more than 10 seconds, you’re likely losing muscle function. Another test: lie on the floor and stand up without using your hands. If you have to roll over and push up with your arms - that’s the Gower’s maneuver. It’s a classic sign of proximal weakness.
How It’s Different From Other Muscle Problems
Many patients are told their weakness is just from their disease - like rheumatoid arthritis getting worse. But steroid myopathy has unique markers:| Feature | Steroid Myopathy | Inflammatory Myopathy (e.g., Polymyositis) |
|---|---|---|
| Onset | Gradual, over weeks to months | Can be sudden or progressive |
| Pain | Absent | Often present |
| CK Levels | Normal (30-170 U/L) | High (often >500 U/L) |
| EMG Results | Normal or mild changes | Early recruitment, fibrillations |
| Muscle Biopsy | Type 2b fiber atrophy only | Inflammation, immune cells present |
| Response to Stopping Steroids | Improves slowly | Worsens initially |
One key point: stopping steroids doesn’t make steroid myopathy worse - unlike inflammatory muscle diseases. That’s a major clue. Also, your creatine kinase (CK) blood test will almost always be normal. If it’s high, something else is going on.

Who’s at Risk?
Anyone on long-term steroids is at risk - especially if they’re taking more than 10 mg of prednisone daily for over four weeks. But some groups are hit harder:- People on high-dose IV steroids in the ICU (like dexamethasone for COVID or sepsis)
- Patients with chronic lung disease (COPD, asthma)
- Those with autoimmune disorders (lupus, rheumatoid arthritis, vasculitis)
- Children on long-term dexamethasone for leukemia treatment
Dexamethasone is especially risky. Its chemical structure makes it more damaging to muscle tissue than prednisone. A 2022 study found it caused myopathy at lower doses and faster rates in pediatric leukemia patients. And here’s the sad truth: a 2022 survey by the National Organization for Rare Disorders found that 68% of patients waited over five months to get the right diagnosis. Many were told they were just “getting older” or “too tired from their illness.”
Physical Therapy: The Only Proven Treatment
There’s no magic pill to reverse steroid myopathy. But there is one thing that works: targeted physical therapy.The goal isn’t to build bulk. It’s to slow down muscle breakdown and retrain your body to use what’s left. Resistance training is the gold standard. The American Physical Therapy Association recommends:
- 2-3 sessions per week of moderate resistance training
- Intensity: 40-60% of your one-rep max (1RM)
- Focus on proximal muscles: hips, thighs, shoulders
- Start low: begin at 30% 1RM, increase by 5-10% every two weeks
A 2020 randomized trial in the Journal of Rehabilitation Medicine followed 88 patients. Those who did supervised resistance training improved their chair rise time by 23.7% in 12 weeks. The control group - who just did stretching - improved by only 8.2%. No injuries. No setbacks.
What exercises work best?
- Chair stands (sit-to-stand without hands)
- Mini squats with support
- Step-ups onto a low platform
- Seated shoulder presses with light bands
- Wall push-ups (easier than floor push-ups)
Avoid high-intensity workouts, heavy lifting, or endurance training like long walks or cycling. These can trigger more muscle breakdown. Progress slowly. Listen to your body. If you feel sore the next day, you went too hard. The goal is consistency, not intensity.
What About Stopping Steroids?
It’s tempting to think: “If steroids are causing this, just stop them.” But that’s not always possible. For many, steroids are life-saving. Stopping them could trigger a flare-up of lupus, asthma, or another serious condition.The key is balance. Work with your doctor to use the lowest effective dose. Some patients can switch to alternate-day dosing. Others may benefit from newer drugs like vamorolone, a selective glucocorticoid receptor modulator. Phase II trials showed it provided the same anti-inflammatory effect as prednisone - but with 40% less muscle weakness.
Even if you can’t stop steroids, physical therapy still helps. Muscle doesn’t disappear overnight. With the right training, you can preserve strength, reduce fall risk, and keep your independence.
Why This Is Still Overlooked
Despite being the most common drug-induced muscle disease - accounting for 65% of all medication-related weakness - steroid myopathy is rarely screened for. Only 32% of rheumatology clinics and 27% of pulmonology clinics have any formal strength assessment protocol.Doctors assume weakness is from the underlying disease. Patients assume it’s just aging. But the cost of ignoring it is high. A 2021 study estimated each case adds $1,200-$2,400 per year in extra healthcare costs - from falls, hospital visits, and rehab. That’s not just money. It’s lost mobility, lost confidence, lost life.
What You Can Do Today
If you’re on steroids and feel weaker:- Ask your doctor for a timed chair rise test. Time yourself doing five stands without using your hands.
- Request a referral to a physical therapist who understands steroid myopathy - not just general rehab.
- Start light resistance training at home: chair stands, wall push-ups, step-ups. Do them daily.
- Track your progress. Note how many seconds it takes to stand, how many steps you can climb without holding on.
- Don’t accept “it’s just from your disease.” Ask: Could this be steroid myopathy?
Steroid myopathy doesn’t have to be a silent thief of your strength. It’s detectable. It’s treatable. And with the right approach, you can keep moving - even while you’re on the medication you need.
Can steroid myopathy be reversed?
Yes, but slowly. Muscle strength typically improves over weeks to months after reducing steroid dose or stopping, especially with consistent resistance training. Some patients regain near-normal function, while others retain mild weakness. The key is early intervention - the longer the weakness goes untreated, the harder it is to recover fully.
Does steroid myopathy cause muscle pain?
No. One of the defining features of steroid myopathy is the absence of pain. You’ll feel weakness - like your legs won’t lift you up or your arms won’t reach - but there’s no soreness, cramping, or tenderness. If you have pain, another condition like polymyositis or tendonitis may be involved.
Are blood tests useful for diagnosing steroid myopathy?
Blood tests like creatine kinase (CK) are usually normal in steroid myopathy, which helps rule out inflammatory muscle diseases. Other tests like aldolase or LDH are also typically within normal range. Normal results don’t mean you’re fine - they actually support the diagnosis of steroid myopathy. Diagnosis relies more on clinical signs and functional tests than bloodwork.
Can I still exercise if I have steroid myopathy?
Yes - but carefully. Low-to-moderate resistance training is not only safe, it’s essential. Avoid high-intensity workouts, heavy lifting, or long cardio sessions. Focus on controlled movements like chair stands, light resistance bands, and wall push-ups. Start at 30% of your one-rep max and increase slowly. Always work with a therapist who understands steroid-induced muscle loss.
What’s the difference between steroid myopathy and deconditioning?
Deconditioning is general weakness from lack of activity. Steroid myopathy is specific muscle fiber damage from steroids. Deconditioning improves quickly with any movement. Steroid myopathy requires targeted resistance training to rebuild type 2b muscle fibers. You can be deconditioned without steroids - but steroid myopathy only happens with steroid use. Both can coexist, but they need different approaches.
How long does it take to see improvement with physical therapy?
Most patients start noticing small improvements in 4-6 weeks - like being able to stand without hands or climb a flight of stairs without stopping. Significant gains, like a 20%+ improvement in timed chair rises, typically happen after 12 weeks of consistent therapy. Patience and consistency matter more than intensity.
Is steroid myopathy permanent?
Not usually. With proper management - reducing steroid dose when possible and doing targeted strength training - most people recover significant strength. In rare cases, especially with prolonged high-dose use, some weakness may persist. But complete, permanent disability is uncommon. Early recognition and therapy make all the difference.
Next Steps: What to Ask Your Doctor
If you suspect steroid myopathy, bring this list to your next appointment:- “Could my weakness be from the steroids I’m taking?”
- “Can we do a timed chair rise test or Gower’s maneuver?”
- “Can you refer me to a physical therapist experienced in steroid myopathy?”
- “Is there a lower-dose alternative or a different steroid I could try?”
- “Should we check my muscle strength every 3-6 months while I’m on long-term steroids?”
Don’t wait until you fall. Don’t assume it’s just aging. Steroid myopathy is real, common, and manageable. With the right awareness and action, you can keep your strength - and your independence - even while you’re on the medication you need.







Comments (8)
Lydia H.
January 17, 2026 AT 19:55 PMBeen on prednisone for lupus for 7 years. I thought my weakness was just from being tired all the time. Turns out I’ve been using my arms to stand up for years and never thought twice about it. This article finally put a name to it. Feels good to know it’s not just me getting old.
Astha Jain
January 18, 2026 AT 07:47 AMso like… steroids make ur muscles weak?? wow. i thought they just made u jacked. also why is everything so long on here like its a textbook lmao
Phil Hillson
January 20, 2026 AT 00:37 AMOkay but let’s be real this is just another medical article trying to scare people into therapy. I’ve been on 5mg prednisone for 3 years and I still deadlift 225. Who even cares if you need your arms to stand up? Maybe you’re just lazy. Also why is there a whole table comparing it to polymyositis like this is a rare disease. It’s literally just a side effect. Stop overcomplicating things.
Josh Kenna
January 21, 2026 AT 12:03 PMI’m a PT and I see this ALL the time. Patients come in saying ‘I can’t get up from my couch’ and the doc says ‘it’s your arthritis’ or ‘you’re just out of shape’. No. It’s the steroids. And it’s fixable. I had a 68-year-old woman on 10mg prednisone for RA start doing chair stands 3x a week. In 8 weeks she was climbing stairs without the rail. No magic. Just consistency. Please don’t let anyone tell you this is normal.
Erwin Kodiat
January 22, 2026 AT 06:14 AMI’m from the Philippines and we don’t have great access to PT here, but I shared this with my cousin who’s on steroids for nephrotic syndrome. She started doing wall push-ups and chair stands every morning. Now she can carry her toddler without help. Small steps matter. You don’t need a gym. You just need to move. And you deserve to keep your strength.
Valerie DeLoach
January 23, 2026 AT 21:22 PMThis is one of the most important articles I’ve read in years. Steroid myopathy is silently robbing people of their independence, and the medical community is failing to screen for it. The fact that 68% of patients wait over five months for diagnosis is unacceptable. We need standardized strength assessments in every clinic that prescribes long-term steroids. Not just rheumatology and pulmonology-endocrinology, oncology, and pediatrics too. This isn’t just about muscle; it’s about dignity. And it’s preventable.
Christi Steinbeck
January 24, 2026 AT 21:27 PMI was told my weakness was ‘just aging’ until I found this. I started chair stands every day. After 6 weeks, I stood up from my couch without my arms for the first time in 2 years. I cried. If you’re on steroids and you feel weak-don’t wait. Start today. You don’t need permission. You don’t need a fancy gym. Just get up. And keep getting up.
Jacob Hill
January 25, 2026 AT 11:39 AMThank you for this. I’ve been telling my doctor for months that my legs feel ‘heavy,’ and he kept saying ‘it’s the disease.’ I finally printed this out and handed it to him. He actually paused. Then said, ‘You’re right. Let’s do the chair test.’ We did it. Took me 14 seconds. He looked shocked. He referred me to PT today. I’m not giving up. Not anymore.