Topical Steroid Risk Calculator
Steroid Risk Assessment Tool
This tool helps you understand the potential risk of skin atrophy and infections based on your topical steroid use. Enter your usage details to get a risk assessment.
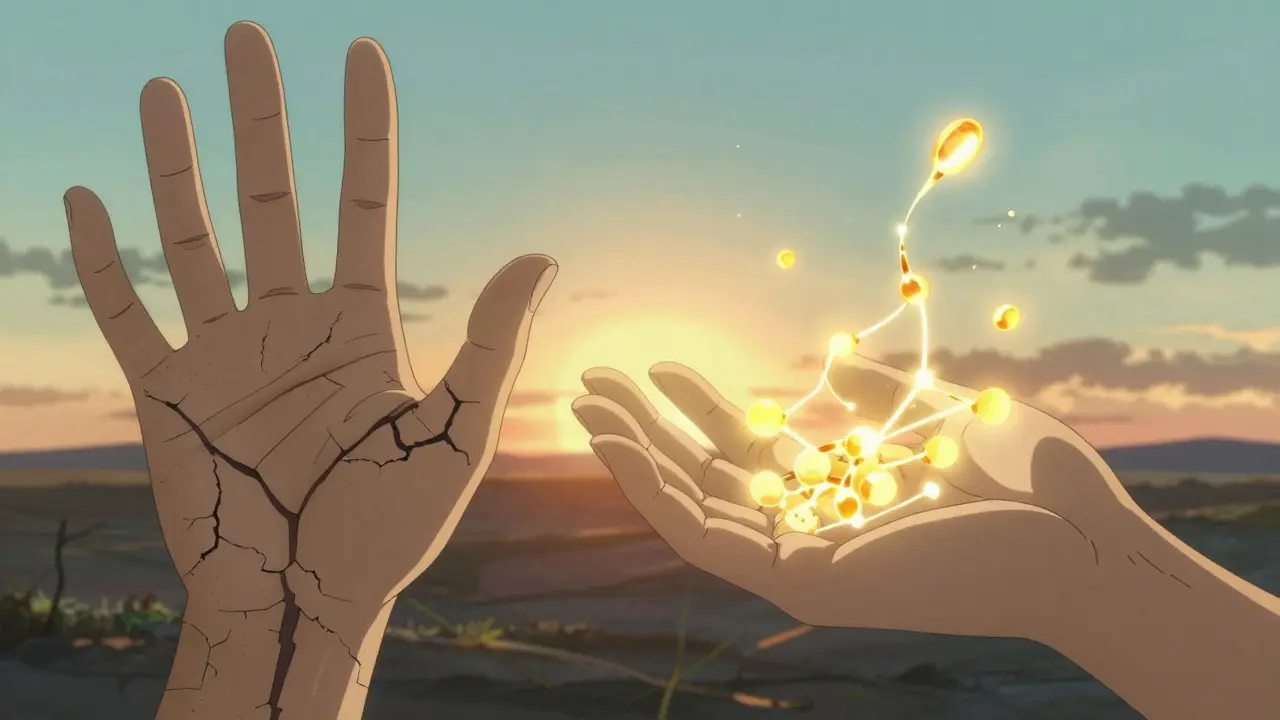
Most people think of topical corticosteroids as a quick fix for itchy, red, or inflamed skin. And for good reason-they work fast. But what happens when you use them too long, too often, or too strong? The skin doesn’t just get better. It starts to break down. Thinner. More fragile. More prone to infection. And sometimes, when you stop using them, things get worse before they get better.
How Topical Corticosteroids Damage Skin Structure
Topical corticosteroids don’t just calm inflammation-they shut down the skin’s natural repair system. When you apply a steroid cream or ointment, it enters skin cells and binds to receptors that control gene activity. This suppresses the production of key proteins like collagen, elastin, and lipids that hold the skin together. Collagen is what gives skin its thickness and strength. Without it, the dermis thins out. The epidermis, the outer layer, also shrinks. The result? Skin that looks and feels like tissue paper.
It’s not just about visible thinning. The skin’s barrier-the protective shield made of ceramides, cholesterol, and fatty acids-gets damaged too. These lipids form a tight, waterproof layer between skin cells. Corticosteroids reduce their production by up to 70% in some cases. That means water escapes easily (increased transepidermal water loss), irritants slip in, and the skin becomes dry, tight, and sensitive. This is why even mild products can cause burning or stinging after prolonged use.
Studies show that even three days of using a potent steroid can begin altering skin structure. Changes might not be visible yet, but the damage is already happening at the cellular level. The stratum corneum-the outermost layer-starts to lose its cohesion. Cells don’t stick together properly. This leads to poor barrier function and increased vulnerability to infections.
What Skin Atrophy Actually Looks Like
Skin atrophy doesn’t always mean obvious thinning. Early signs are subtle: fine lines that look like wrinkles, but aren’t caused by aging. These are called “elephant wrinkles”-deep, crepey folds that appear on the face, inner arms, or thighs. They don’t fade when you stretch the skin, unlike normal wrinkles. Other signs include:
- Visible blood vessels (telangiectasia) because the skin is too thin to hide them
- Purple or red patches (purpura) from minor bumps that cause bruising
- Stretch marks (striae) that look like silvery lines, especially on the abdomen or thighs
- Acne-like bumps or rosacea-like redness around the mouth or nose
These changes are most common on thin-skinned areas: the face, eyelids, neck, armpits, groin, and skin folds. Children and older adults are at higher risk because their skin is naturally thinner. Even low-potency steroids can cause atrophy in these areas if used daily for more than two weeks.
Once stretch marks form, they’re permanent. The collagen loss is irreversible. But early atrophy-before striae appear-can improve. Studies show that after stopping steroids and using barrier repair creams, skin thickness can increase by up to 30% within 12 weeks. But only if you stop using the steroid.
Why Infections Follow Skin Atrophy
Thinner skin isn’t just fragile-it’s defenseless. The skin’s natural immune guards-Langerhans cells and antimicrobial peptides-get suppressed by corticosteroids. This creates the perfect environment for infections to take hold.
Fungal infections like candidiasis are common. You’ll see red, scaly patches with tiny pustules around the edges, often in moist areas like the groin or under the breasts. Bacterial infections, especially from Staphylococcus aureus, can cause impetigo-yellow crusts, oozing sores, and spreading redness. Viral infections like herpes simplex can flare up and become severe, with large, painful blisters that don’t heal normally.
One 2021 review of over 8,000 patients found that 5.8% developed rosacea-like redness, 4.3% got perioral dermatitis (a rash around the mouth), and 3.1% developed acneiform eruptions from long-term steroid use. These aren’t allergies-they’re direct side effects of immune suppression.
What makes it worse? Using steroids on broken skin. People with eczema often apply steroids to cracked, bleeding areas. That’s when bacteria and fungi slip in deeper. In some cases, infections become systemic-spreading to the bloodstream. That’s rare, but it happens.

Potency, Area, and Duration: The Three Risk Factors
Not all steroids are the same. They’re ranked from Class I (most potent) to Class VII (least potent). In the UK and US, Class I-IV steroids (like clobetasol, betamethasone, and hydrocortisone 2.5%) carry the highest risk. Class V-VII (like hydrocortisone 1%) are safer for short-term use.
But potency isn’t the only factor. Where you apply it matters. The face, eyelids, and genitals absorb steroids 3 to 5 times faster than the back or arms. That’s why dermatologists never recommend strong steroids on the face-even for severe eczema.
Duration is the biggest trigger. Using a potent steroid for more than two weeks on the face, or more than four weeks on the body, dramatically increases risk. A 2020 study found that 17% of long-term users developed visible atrophy. That’s nearly 1 in 5 people.
And here’s the catch: many people don’t realize they’re using a strong steroid. Some over-the-counter creams in the UK and US still contain hydrocortisone 2.5%-a Class IV steroid. Labels don’t always say “potent.” They say “for severe itching.” People use it daily for months. That’s how the problem grows quietly.
What Happens When You Stop: Topical Steroid Withdrawal
Stopping steroids after long-term use isn’t simple. The skin doesn’t just bounce back. It rebels. This is called Topical Steroid Withdrawal (TSW). It’s not addiction-it’s a rebound inflammation caused by the skin’s sudden lack of suppression.
The pattern is predictable. Within days to a week after stopping, the skin turns bright red. It burns. It itches. It feels like a sunburn that won’t quit. Then it flakes. Then it flares again. Each flare gets shorter, but the recovery periods get longer. For someone who used steroids for six months, withdrawal can last 6 to 12 months. For those who used them for years, it can take over two years.
Reddit communities with over 4,000 members report the same symptoms: burning face syndrome, skin shedding like snake skin, and extreme sensitivity to water, sweat, and even clothing. Many say they can’t wear makeup, use soap, or go outside without severe discomfort.
There’s no cure for TSW. Only time and careful skin care help. The key is to stop completely-not taper slowly. Tapering can prolong withdrawal. But stopping cold turkey is terrifying. That’s why medical supervision matters.
How to Prevent and Treat Steroid-Induced Skin Damage
Prevention is easier than repair. Here’s what works:
- Use the lowest strength possible. Start with hydrocortisone 1% unless your doctor says otherwise.
- Limit use to 5-7 days on the face, 14 days on the body. Never use potent steroids for more than two weeks without a break.
- Avoid applying to broken skin. Only use on intact, inflamed areas.
- Never use on the face unless prescribed. Even then, use the weakest option and for no longer than 5 days.
- Protect skin from the sun. UV rays break down collagen faster. Use SPF 50+ daily, even indoors.
If atrophy has already happened, stop the steroid. Then focus on repair:
- Use barrier creams with ceramides, cholesterol, and free fatty acids in a 3:1:1 ratio. These mimic the skin’s natural lipids. Clinical trials show 68% improvement in barrier function after 8 weeks.
- Apply moisturizers right after bathing, while skin is damp.
- Avoid fragrances, alcohol, and harsh soaps. They worsen irritation.
- Consider non-steroidal alternatives like crisaborole or tapinarof for eczema. These are FDA-approved and don’t cause atrophy.
For infections, treat them directly. Antifungals for yeast, antibiotics for bacteria. Steroids won’t help-and they’ll make it worse.
The Future: Safer Alternatives Are Coming
Pharma companies are working on steroid alternatives that reduce inflammation without damaging skin. One promising approach is “dual-soft” glucocorticoid agonists-molecules that calm inflammation but don’t block collagen production. Early lab results show they’re just as effective as traditional steroids but cause 80% less atrophy.
The NIH is testing a new cream that combines low-dose corticosteroids with fibroblast growth factor. In Phase II trials, it cut atrophy rates by 63% over 12 weeks. That’s a game-changer.
By 2028, the global market for steroid-sparing treatments is expected to hit $3.8 billion. Demand is rising because patients are demanding safer options. And doctors are finally listening.
Topical corticosteroids are powerful tools. But they’re not harmless. Used right, they heal. Used wrong, they hurt. The key isn’t fear-it’s awareness. Know the risks. Know the signs. And never use them longer than you need to.
Can skin atrophy from steroids be reversed?
Yes, early skin atrophy can improve after stopping steroids and using barrier repair creams with ceramides, cholesterol, and fatty acids. Studies show up to 30% improvement in skin thickness within 12 weeks. But once stretch marks (striae) form, the damage is permanent because collagen fibers are destroyed.
How long does topical steroid withdrawal last?
Withdrawal lasts as long as the steroid was used. For someone who used steroids for 3 months, symptoms may last 4-8 months. For those who used them for years, recovery can take 18-36 months. Each flare gets shorter, but the healing periods between flares get longer. Patience and gentle skin care are essential.
Is hydrocortisone 1% safe for long-term use?
Hydrocortisone 1% is considered low potency and is generally safe for short-term use (up to 2 weeks). But even this can cause atrophy if used daily on thin skin (like the face or genitals) for more than 4 weeks. Always follow your doctor’s instructions and never use it continuously without breaks.
Can I use steroid creams on my child’s eczema?
Yes, but with caution. Children’s skin is thinner and absorbs more steroid. Use only the weakest strength needed (usually hydrocortisone 0.5%-1%), apply sparingly, and limit to 5-7 days at a time. Avoid strong steroids (Class I-IV) unless under strict medical supervision. Always pair with moisturizers to protect the skin barrier.
What should I do if my skin gets worse after stopping steroids?
This is likely topical steroid withdrawal. Stop all steroids immediately. Focus on gentle skin care: fragrance-free moisturizers, cool compresses, and avoiding triggers like heat and sweat. Do not restart steroids-it will delay recovery. See a dermatologist experienced in TSW. They can help manage symptoms and rule out infections.
Are there any non-steroid treatments for eczema?
Yes. Topical calcineurin inhibitors like tacrolimus and pimecrolimus are FDA-approved for eczema and don’t cause skin thinning. Newer options include crisaborole (a PDE4 inhibitor) and tapinarof (a natural aryl hydrocarbon receptor agonist). These are effective for mild to moderate eczema and can be used long-term without atrophy risk.
Next Steps: What to Do Now
If you’re using a topical steroid:
- Check the label. Is it Class I-IV? If yes, and you’ve used it for more than 2 weeks, talk to your doctor.
- Look at your skin. Are there red patches, visible veins, or deep wrinkles? These are warning signs.
- Start using a ceramide-based moisturizer daily. It won’t fix everything, but it will help protect your skin.
- Never use steroids on the face unless prescribed-and even then, use the lowest dose for the shortest time.
If you’ve stopped and your skin is burning or flaring: don’t panic. This is common. It will pass. But don’t reach for the steroid again. You’re not weak-you’re healing. And you’re not alone.




Comments (15)
Conor Murphy
January 28, 2026 AT 04:54 AMI used a steroid cream for my eczema for like 6 months straight... didn't realize it was causing my face to look like crumpled paper. When I stopped, my skin went full nuclear red. Burned for months. But honestly? I'm glad I quit. My skin's finally healing, slow as hell but it's healing. 🙏
Paul Taylor
January 28, 2026 AT 21:33 PMPeople need to understand that steroids are not skincare they are medical tools like a chainsaw you dont use it to trim hedges and you dont use it daily for years and expect your skin to stay intact the body has memory and your skin remembers every time you overuse it and then it fights back hard
Kirstin Santiago
January 30, 2026 AT 16:13 PMI didn't know hydrocortisone 2.5% was even considered potent until I read this. I've been using it daily for my dry patches on my neck for over a year. No wonder I have these weird purple lines now. Time to switch to ceramide cream and give my skin a break.
Kathy McDaniel
February 1, 2026 AT 01:37 AMomg i thought i was just getting old but my eyelids are so thin now i can see the veins and i keep getting yeast rashes under my nose i just thought it was stress but this makes total sense im gonna stop the cream today
Patrick Merrell
February 1, 2026 AT 02:20 AMThis is why Big Pharma wants you addicted to steroids. They make billions off people who can't stop. The real cure? Avoid them entirely. Your skin doesn't need chemicals to heal. Nature does it better. 🤷♂️
Conor Flannelly
February 1, 2026 AT 18:10 PMThere's a quiet tragedy here. We treat skin like a problem to be solved, not a living organ to be respected. Corticosteroids don't heal-they silence. And silence, when prolonged, becomes a kind of death. The skin doesn't scream when it's dying. It just gets thinner. And quieter. And then it's too late.
Marian Gilan
February 2, 2026 AT 14:17 PMThey're hiding the truth. The FDA knows steroid withdrawal is real but they don't warn people because then people would stop buying. I saw a doctor who said 'it's just eczema flaring' but my skin was shedding like a snake. This is chemical warfare on your body. They don't want you to know how deep this goes.
Desaundrea Morton-Pusey
February 3, 2026 AT 09:27 AMI'm so tired of this 'natural healing' nonsense. You think your skin is gonna fix itself? I had a flare so bad I couldn't sleep. I used the cream and I felt human again. If you want to suffer, go ahead. I'll take my steroid and my peace of mind.
Murphy Game
February 4, 2026 AT 16:04 PMThe real danger isn't the cream. It's the people who post this stuff online. They scare new moms into avoiding steroids for their kids. Then the eczema gets worse. Then they end up in the ER. You're not helping. You're enabling reckless parenting.
John O'Brien
February 6, 2026 AT 14:48 PMBro I went full TSW after 10 months of steroid cream on my arms. Skin was raw, peeling, burning like I’d been dipped in acid. I thought I was dying. But I stopped cold turkey. 14 months later? I’ve got better skin than I did at 20. No joke. It’s brutal but it’s worth it.
Kegan Powell
February 8, 2026 AT 13:22 PMWe're all just trying to find balance. Your skin isn't broken. It's just overwhelmed. Steroids are like putting a bandaid on a broken leg. It stops the pain but the bone stays snapped. Ceramides? That's the cast. Slow. Boring. But it actually rebuilds. I've been using the 3:1:1 cream for 3 months. My skin finally feels like skin again
April Williams
February 10, 2026 AT 13:06 PMI'm calling BS on this whole 'withdrawal' thing. It's just people being dramatic. If you can't handle a little redness, maybe you shouldn't have used the cream in the first place. I've been using hydrocortisone for 15 years and I'm fine. Your skin is weak, not poisoned.
Harry Henderson
February 10, 2026 AT 18:23 PMSTOP USING STEROIDS. NOW. If you're reading this and you're still using that cream on your face-put it down. Walk away. Go buy a ceramide moisturizer. Your skin is begging you. Don't wait until you can't wear a shirt without it sticking to your wounds. You got this.
suhail ahmed
February 11, 2026 AT 06:28 AMIn India we call this 'steroid face'-people use it to lighten skin and end up with shiny, thin, vein-covered cheeks. It’s a cultural epidemic. My aunt used it for 12 years. Now her skin cracks like old leather in winter. No cream fixes that. Only time. And regret.
Candice Hartley
February 12, 2026 AT 00:59 AMI had no idea. I just thought my skin was dry. Now I know why it burns when I wash my face. I'm switching to plain petroleum jelly tonight. No more creams. Just peace.