Why Electrolyte Imbalances Matter More Than You Think
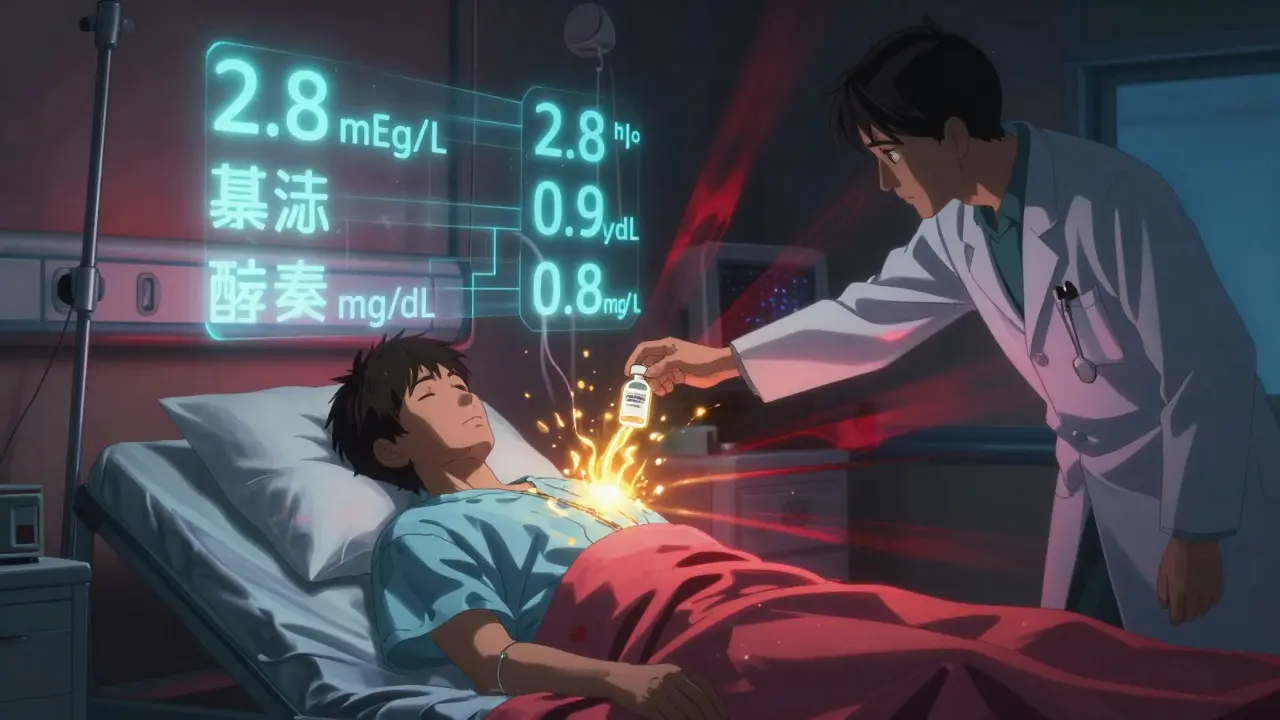
When your potassium drops below 3.0 mEq/L, your heart can start skipping beats. If phosphate falls under 1.0 mg/dL, your lungs might stop working properly. And if magnesium dips too low, even giving potassium won’t fix the problem. These aren’t rare lab quirks-they’re life-or-death issues that happen every day in hospitals, especially in people with kidney disease, heart failure, or those on diuretics.
Electrolytes like potassium, phosphate, and magnesium don’t just float around doing nothing. They control nerve signals, muscle contractions, energy production, and fluid balance. When they’re out of range, the body doesn’t adapt gracefully-it starts to shut down. The good news? These imbalances are often preventable-and treatable-if you know what to look for and when to act.
Normal Ranges and When to Worry
Here’s what normal looks like, and when things turn dangerous:
- Potassium: Normal is 3.2-5.0 mEq/L. Anything below 3.0 mEq/L or above 6.5 mEq/L needs immediate action.
- Magnesium: Normal is 1.7-2.2 mg/dL. Below 1.0 mg/dL is critical; above 2.5 mg/dL can cause paralysis or breathing trouble.
- Phosphate: Normal is 2.5-4.5 mg/dL. Below 1.0 mg/dL risks respiratory failure. Above 4.5 mg/dL can cause calcium to drop dangerously low.
These numbers aren’t just guidelines-they’re red flags. A potassium level of 2.8 mEq/L in someone on lisinopril and furosemide? That’s not just low-it’s a ticking time bomb for arrhythmias. A phosphate level of 0.8 mg/dL in a diabetic patient after insulin therapy? That’s refeeding syndrome waiting to happen.
The Hidden Link: Why Magnesium Comes First
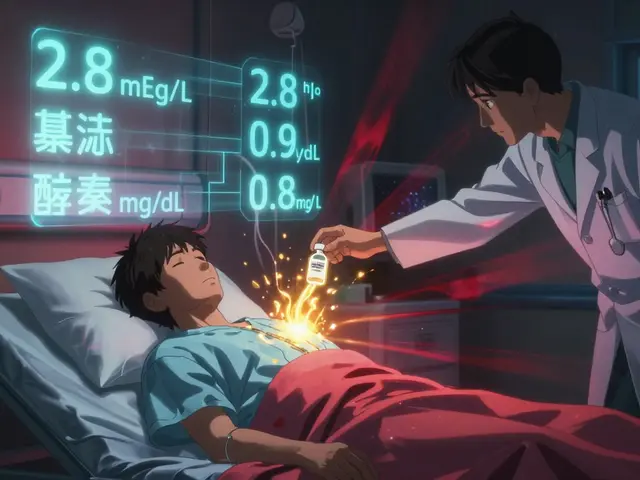
Here’s a fact most clinicians still miss: you can’t fix low potassium if magnesium is also low.
When magnesium is under 1.7 mg/dL, your kidneys keep flushing out potassium no matter how much you give. It’s like trying to fill a bucket with a hole in the bottom. That’s why guidelines from the American Heart Association and the European Society of Cardiology now say: check magnesium before treating hypokalemia.
Studies show that in patients with both low potassium and low magnesium, giving only potassium has a 60% failure rate. But when magnesium is replaced first-typically with 4 grams of IV magnesium sulfate over 30-60 minutes-the potassium response improves dramatically. And it’s not just about potassium. Low magnesium also makes low calcium stubborn to correct. So if someone’s not responding to calcium gluconate, check magnesium.
How to Replace Potassium Safely
Replacing potassium sounds simple-just give some KCl, right? Wrong. Too fast, and you can stop someone’s heart. Too slow, and they stay at risk.
For mild hypokalemia (3.0-3.4 mEq/L), oral potassium chloride (20-40 mEq daily) is safe and effective. But if the level is below 3.0 mEq/L, especially with symptoms like muscle weakness or ECG changes, you need IV. Here’s the rule:
- Peripheral IV: Max 10 mEq/hour. Never more.
- Central line: Max 40 mEq/hour, only in ICU or monitored settings.
- Each 20 mEq of IV KCl raises serum potassium by about 0.25 mEq/L.
Always monitor potassium levels at 1, 2, 4, 6, and 24 hours after starting IV replacement. And never, ever give potassium as a bolus. Ever.
For patients on dialysis or with kidney failure, potassium binders like patiromer or sodium zirconium cyclosilicate (approved by NICE in early 2023) are now first-line for chronic hyperkalemia. They’re safer than old-school kayexalate and don’t cause bowel necrosis.

Phosphate: The Silent Crisis in Critical Care
Phosphate gets ignored until someone can’t breathe. That’s because hypophosphatemia often shows up in ICU patients after they’re stabilized-after insulin, after refeeding, after iron infusions.
The FDA issued a safety alert in 2020 about ferric carboxymaltose, an IV iron drug used for anemia. It can cause phosphate levels to crash within days, even in people with normal kidneys. Now, every time someone gets this drug, labs should be checked at day 3 and day 7.
For treatment:
- Oral: 8 mmol elemental phosphorus per dose (like Neutra-Phos or K-Phos Neutral).
- IV: 7.5 mmol in 250 mL D5W over 4-6 hours. Never faster.
- Never give more than 7.5 mmol in 24 hours unless levels are below 0.5 mg/dL.
Watch for rebound hyperphosphatemia after correction-it can trigger tetany or calcification. And remember: phosphate and calcium are partners. When phosphate drops, calcium rises. When you fix phosphate, calcium can crash. Check both.
Hypermagnesemia: Rare, But Deadly
High magnesium is uncommon outside of kidney failure or overdose (like too much Epsom salt or magnesium-based antacids). But when it happens, it’s serious.
At 2.5-5 mg/dL, you see nausea, flushing, and low blood pressure. Above 5 mg/dL, reflexes disappear. Above 7 mg/dL, the heart can stop.
Treatment is straightforward:
- Stop all magnesium sources.
- Give 10-20 mL of 10% calcium gluconate IV over 5-10 minutes to reverse neuromuscular blockade.
- Use IV furosemide if kidneys are working to flush it out.
- If levels are above 10 mg/dL or the patient is in respiratory distress-get on dialysis.
Don’t wait for symptoms. If a patient with CKD stage 4 or 5 gets a magnesium infusion, check levels 2 hours later.
Monitoring: The 1-2-4-6-24 Rule
Electrolyte correction isn’t a one-and-done deal. It’s a marathon of lab checks.
After treating hyperkalemia, you must check potassium at:
- 1 hour
- 2 hours
- 4 hours
- 6 hours
- 24 hours
Why? Because insulin and glucose shift potassium into cells temporarily. The real level comes back up in 6-12 hours. If you stop monitoring too soon, you’ll think the problem’s fixed-until the patient codes.
Same goes for phosphate. After IV replacement, check levels at 6 and 12 hours. And always check calcium when phosphate is low or being replaced.

Who’s at Risk? The High-Risk Groups
These patients need routine electrolyte checks:
- Those on diuretics (especially loop diuretics like furosemide)
- People with chronic kidney disease (stages 3-5)
- Patients on ACE inhibitors, ARBs, or spironolactone
- Diabetics starting insulin or recovering from DKA
- Malnourished or post-op patients
- Anyone getting IV iron (ferric carboxymaltose)
- Patients on long-term PPIs (linked to low magnesium)
At Vanderbilt University Medical Center, adding routine electrolyte panels to electronic order sets for these groups cut electrolyte-related deaths by 18.7% in just one year. Simple. Effective.
What’s New in 2026?
The field has moved fast since 2020:
- Point-of-care electrolyte testing in ERs now cuts time to treatment by 37 minutes.
- New phosphate binders for kidney patients reduce hypophosphatemia risk without sacrificing phosphate control.
- Genetic testing for renal electrolyte handling is entering phase 3 trials-soon, we might tailor potassium doses based on a patient’s DNA.
- AI-driven alerts in EHRs now flag patients at risk for refeeding syndrome or drug-induced hypophosphatemia before labs even come back.
These aren’t futuristic ideas-they’re in use now in major hospitals. The goal? Prevent the crisis before it starts.
Final Takeaway: Think in Systems, Not Just Numbers
Don’t treat potassium in isolation. Don’t fix magnesium without checking calcium. Don’t give phosphate without watching for rebound.
Electrolytes don’t work alone. They dance together. One out of balance pulls the others down. The best clinicians don’t just read labs-they see the pattern. They know that a low potassium in a heart failure patient isn’t just about the diuretic-it’s about the low magnesium, the low phosphate, and the recent iron infusion.
Check them all. Replace them right. Monitor them close. That’s how you turn a dangerous imbalance into a solved problem.





Comments (14)
Doreen Pachificus
January 5, 2026 AT 00:51 AMI've seen so many residents overlook magnesium when treating low K+. It's crazy how often you give KCl and it just... doesn't stick. Like pouring water into a colander. This post nailed it.
Especially in heart failure patients on spironolactone. You fix the K+, then two hours later it's back down. Magnesium first. Always.
Stephen Craig
January 6, 2026 AT 22:56 PMElectrolytes are the silent orchestra. One instrument out of tune and the whole piece collapses.
Roshan Aryal
January 8, 2026 AT 04:14 AMThis is what happens when you let American medical guidelines become gospel. In India we treat potassium the old way - with clinical judgment, not lab numbers. You think a 2.8 K+ is a crisis? We see 2.1 and keep working. The body adapts. Your algorithms don't.
Charlotte N
January 8, 2026 AT 23:57 PMI'm so glad someone finally said it about magnesium... I've been saying this for years but no one listens... like literally no one... I had a patient last week... K was 2.7... gave 80 mEq KCl... nothing... then we gave 4g MgSO4... K jumped to 3.9 in 90 minutes... why is this not standard??
bob bob
January 9, 2026 AT 19:15 PMThis is the kind of stuff that actually saves lives. Not flashy new drugs or AI alerts - just remembering the basics. I wish med school taught this like it was breathing. Instead we memorize 500 drug side effects and forget the body’s wiring.
Vicki Yuan
January 11, 2026 AT 14:43 PMThe 1-2-4-6-24 monitoring rule is non-negotiable. I once had a patient coded at 18 hours because we stopped checking after 6. We thought the insulin had done its job. It didn’t. The potassium came roaring back. Don’t be that team.
Uzoamaka Nwankpa
January 12, 2026 AT 06:12 AMI used to work in an ICU where they gave IV potassium at 50 mEq/hr. No one died. But everyone was terrified. And then one night, a nurse cried because she thought she killed someone. This post should be mandatory reading for every nurse, every resident, every attending. We are so scared of doing harm we forget how to heal.
Abhishek Mondal
January 13, 2026 AT 05:35 AMYou claim magnesium is the key... but have you ever considered that Western medicine is fundamentally flawed? The body doesn’t need IV magnesium sulfate - it needs ancestral diets, sunlight, and reduced pharmaceutical interference. You’re treating symptoms with chemicals while ignoring root causes. This is why patients are sicker than ever.
Terri Gladden
January 14, 2026 AT 13:13 PMOMG I JUST HAD A PATIENT LIKE THIS LAST WEEK!!! I THOUGHT I WAS GOING TO LOSE HER!!! SHE WAS ON LISINOPRIL AND FUROSEMIDE AND HER K WAS 2.6 AND SHE WAS WEAK AND HER ECG WAS WILD AND THEN WE FOUND HER MG WAS 1.1 AND WE GAVE MAG AND SHE WAS FINE BY MORNING I CRIED I WAS SO RELIEVED
Jennifer Glass
January 14, 2026 AT 15:06 PMI’ve been in nursing for 18 years and this is still the most overlooked thing. Magnesium isn’t just a ‘bonus’ electrolyte - it’s the foundation. I’ve watched so many patients get passed over because someone thought, ‘Oh, they’re just low K, give some KCl.’ No. You fix the leak first.
Also - thank you for mentioning the IV iron link. I’ve seen two cases now where phosphate crashed after ferric carboxymaltose. No one connects it.
Joseph Snow
January 15, 2026 AT 00:37 AMThis is textbook NIH-funded groupthink. You cite AHA and ESC guidelines like they’re scripture. But what about the studies showing IV magnesium has no significant impact on potassium retention in 40% of cases? And who funded the ‘AI alerts’ you’re promoting? Big Pharma. The real crisis is overmedicalization - not under-treated electrolytes.
Jack Wernet
January 16, 2026 AT 02:45 AMThank you for this comprehensive and clinically grounded summary. The emphasis on systemic thinking - rather than isolated lab values - reflects the highest standard of medical reasoning. This is precisely the kind of nuanced, evidence-based perspective that should be taught in all clinical rotations.
Catherine HARDY
January 17, 2026 AT 01:38 AMYou know who really controls these guidelines? The dialysis companies. They profit from potassium binders. They profit from IV magnesium. They profit from endless lab draws. The real reason they push this 1-2-4-6-24 rule? To keep you billing. They don’t care if you’re exhausted. They care about your CPT codes.
Chris Cantey
January 17, 2026 AT 05:22 AMWe’re all just trying to survive the algorithm. The machine tells us to check magnesium. The machine tells us to monitor K every hour. The machine says ‘don’t bolus.’ But what if the machine is wrong? What if the patient’s body knows better than the EHR? I’ve seen patients stabilize without any intervention. Maybe we’re the problem.