Generic drugs make up 90% of all prescriptions filled in the U.S., but they account for just 23% of total drug spending. That sounds like a win-until you see the bill at the pharmacy counter. For many Americans, even a $15 monthly generic can be a hardship. The reason? The system isn’t broken-it’s complicated. And government control of generic prices isn’t about setting fixed prices like in Europe. It’s about layers of rebates, hidden discounts, and market competition that don’t always reach the patient.
How Generic Drug Prices Are Actually Set
The U.S. government doesn’t directly set the price of generic drugs. Instead, it uses a mix of rules that push prices down indirectly. The main tool? The Medicaid Drug Rebate Program (MDRP). Since 1990, drugmakers have had to pay rebates to Medicaid for every generic drug sold. The rebate is the bigger of two numbers: 23.1% of the Average Manufacturer Price (AMP) or the difference between AMP and the Best Price-the lowest price offered to any commercial buyer. This forces manufacturers to keep prices low if they want to sell to Medicaid, which covers 80 million Americans. These rebates aren’t just paperwork. In 2024, they totaled $14.3 billion, and 78% of that came from generics. But here’s the catch: those savings rarely go to the patient. Most of the rebate goes to state Medicaid programs, not the person holding the prescription.Medicare Part D and Out-of-Pocket Caps
For seniors on Medicare Part D, generic drug costs changed dramatically in 2025. Before, beneficiaries paid 25% coinsurance during the initial coverage phase. Now, thanks to the Inflation Reduction Act (IRA), the annual out-of-pocket cap is $2,000. That means if you take multiple generics, your spending stops at $2,000-even if your total drug costs are $10,000. Low-Income Subsidy (LIS) beneficiaries pay even less: between $0 and $4.90 per generic prescription. That’s a big relief for people on fixed incomes. But not everyone qualifies. And even with the cap, premiums and formulary changes can still surprise you. One woman in Florida paid $15 a month for generic lisinopril-until her pharmacy switched to a different manufacturer with a higher copay. She got a $90 bill. No warning. No notice.Why Generic Prices Still Fluctuate
Generic drugs are supposed to be cheap because multiple companies make them. But when only one or two manufacturers are left, prices spike. In 2024, the generic version of pyrimethamine (Daraprim) jumped 300% after competitors exited the market. There’s no price ceiling. No government intervention. Just market failure. This happens often in niche drugs-like those for rare conditions or older medications with low profit margins. The FDA approved over 1,200 generics in 2024, but many of those are for popular drugs like statins or blood pressure meds. For the rest? Manufacturers walk away. And when competition disappears, so does the price drop.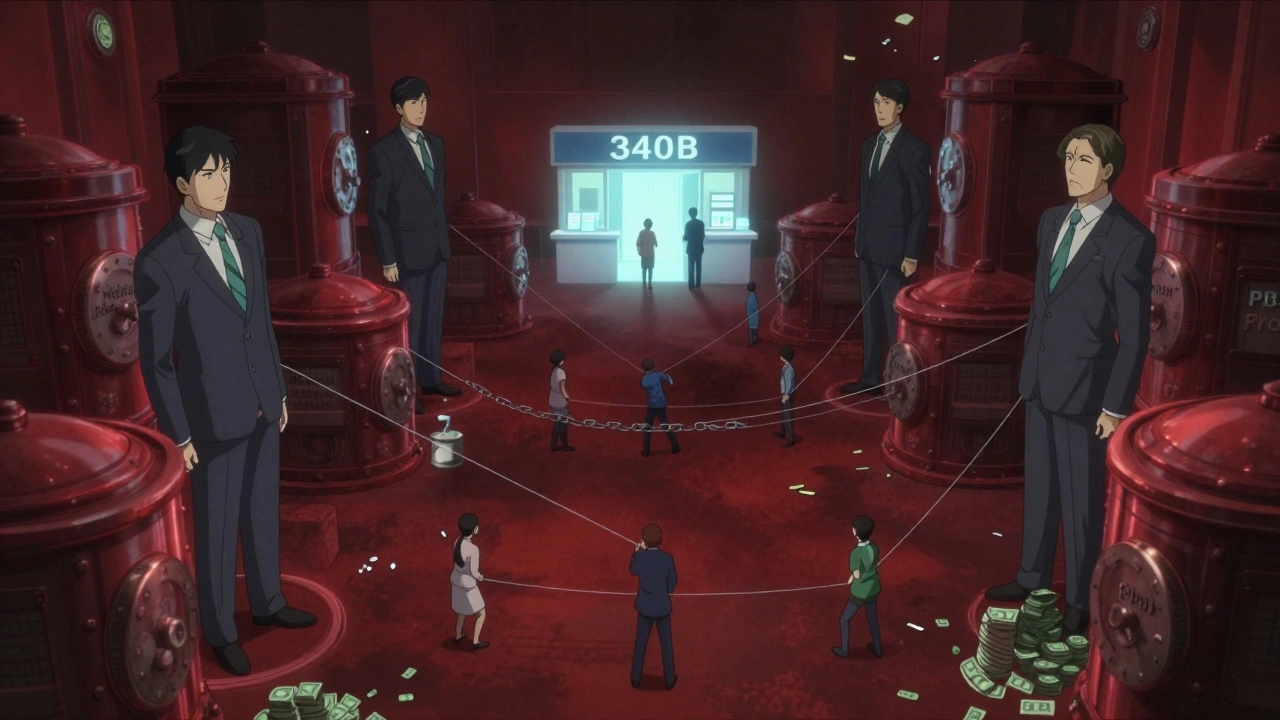
The 340B Program: Hidden Savings for the Vulnerable
One of the most effective-but least known-programs is 340B. It requires drugmakers to sell outpatient medications at steep discounts to hospitals and clinics that serve low-income patients. The average discount? 20% to 50% below AMP. Community health centers report that 87% of patients stick to their meds because they can finally afford them. But here’s the twist: 340B doesn’t apply to retail pharmacies. So if you’re not treated at a qualifying clinic, you won’t see those savings. And while the program saves millions, it’s under legal attack from drugmakers who claim it’s being misused. The government defends it as essential care.What’s Changing in 2026 and Beyond
The biggest shift isn’t about controlling all generics-it’s about picking a few. Starting in 2026, Medicare will begin negotiating prices for 10 high-cost drugs each year. The first round included brand-name drugs like insulin and blood thinners. But in 2027, for the first time, generic versions of apixaban (Eliquis) and rivaroxaban (Xarelto) will be on the list. That’s huge. These two drugs alone cost Medicare $40.7 billion in 2025. Analysts predict prices for these generics could drop 25% to 35% after negotiation. That’s not because the government is setting prices-it’s because Medicare is using its buying power to force a discount, just like the VA does. The VA already gets 40% to 60% off generics. Why can’t Medicare?Why the U.S. Pays More Than Other Countries
The U.S. pays 1.3 times more for generic drugs than other wealthy countries. Canada, the U.K., and Germany don’t wait for competition to lower prices-they negotiate directly. The U.K.’s NICE sets prices based on health outcomes. Germany checks if a drug is worth more than what it costs. The U.S. just lets the market decide. Critics say this approach is inefficient. A 2025 study found that if Medicare negotiated generic prices like the VA, the U.S. could save $12.7 billion over ten years. That’s not enough to fix the whole system, but it would help millions of seniors.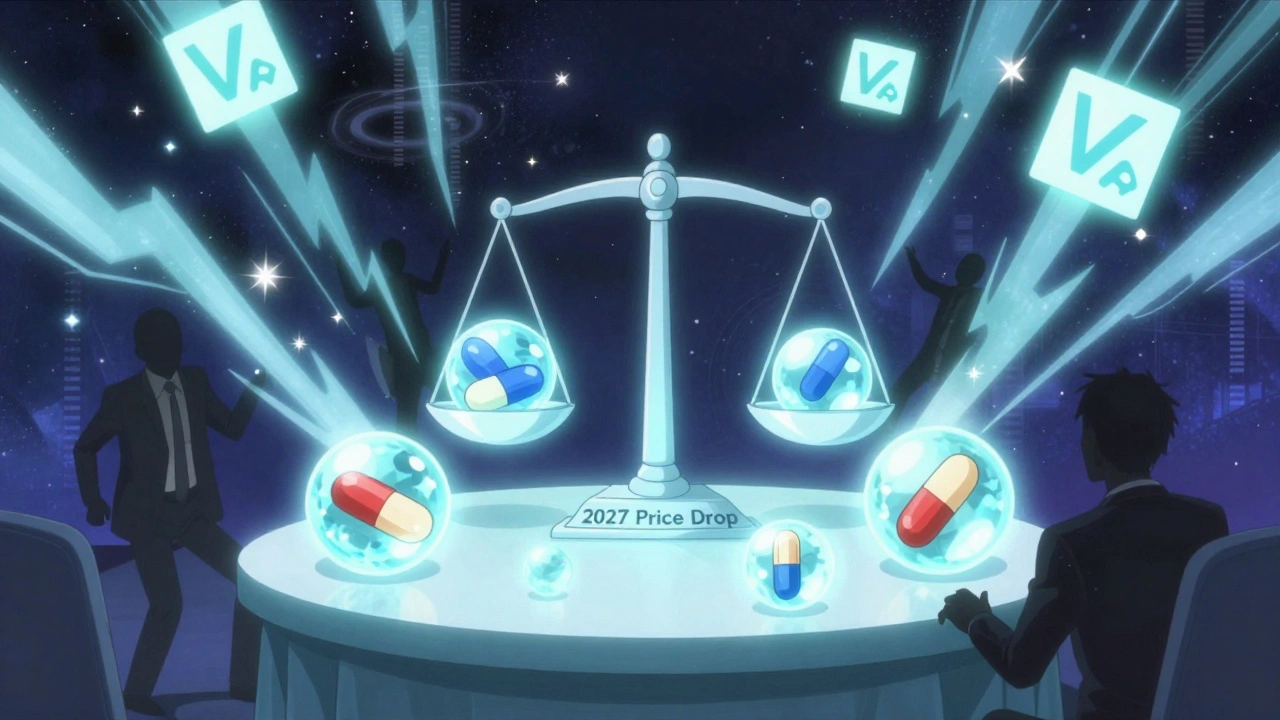
Who’s Really Behind the Price?
Pharmacy Benefit Managers (PBMs) are the middlemen between drugmakers, insurers, and pharmacies. They negotiate rebates, set formularies, and collect fees. But here’s the problem: 68% of the “savings” from rebates never reach the patient. PBMs keep the money as profit or use it to lower premiums-while patients still pay high copays. A 2025 Senate report found that many generic drugs are priced high on purpose, so PBMs can show “big discounts” later. It’s a shell game. The patient sees a $50 copay. The pharmacy gets $30. The PBM collects $20 in rebate. But the patient still paid $50.What Patients Can Do Right Now
You can’t control the system-but you can work around it.- Use the Medicare Plan Finder tool to compare Part D plans. Don’t just pick the cheapest premium-check the copay for your specific generics.
- Ask your pharmacist if there’s a lower-cost generic alternative within the same class. Sometimes, a different manufacturer costs half as much.
- If you’re on Medicaid or qualify for LIS, make sure you’re enrolled. You could be paying $0.
- Check if your local clinic participates in the 340B program. You might be able to fill prescriptions there for far less.
- Use mail-order pharmacies. They often have lower copays for 90-day supplies.








Comments (1)
Michael Campbell
December 1, 2025 AT 20:40 PMThis whole system is rigged. PBMs are the real villains - they’re the ones sucking the blood out of your wallet while pretending to save you money. I’ve seen it with my own eyes. $50 copay? That’s just the tip of the iceberg. The government’s just playing along. Wake up, people.
They don’t want you to know how deep this goes. It’s not about healthcare. It’s about control.