If you’re taking ritonavir for HIV treatment, you’re not alone in noticing changes in your mouth. Dryness, sores, or a strange taste aren’t just annoying-they’re common side effects. Many people assume these are minor, but they can lead to serious dental problems if ignored. Ritonavir doesn’t just work on viruses-it changes your mouth’s environment, making it easier for infections to grow and harder for your gums to heal.
Why Ritonavir Affects Your Mouth
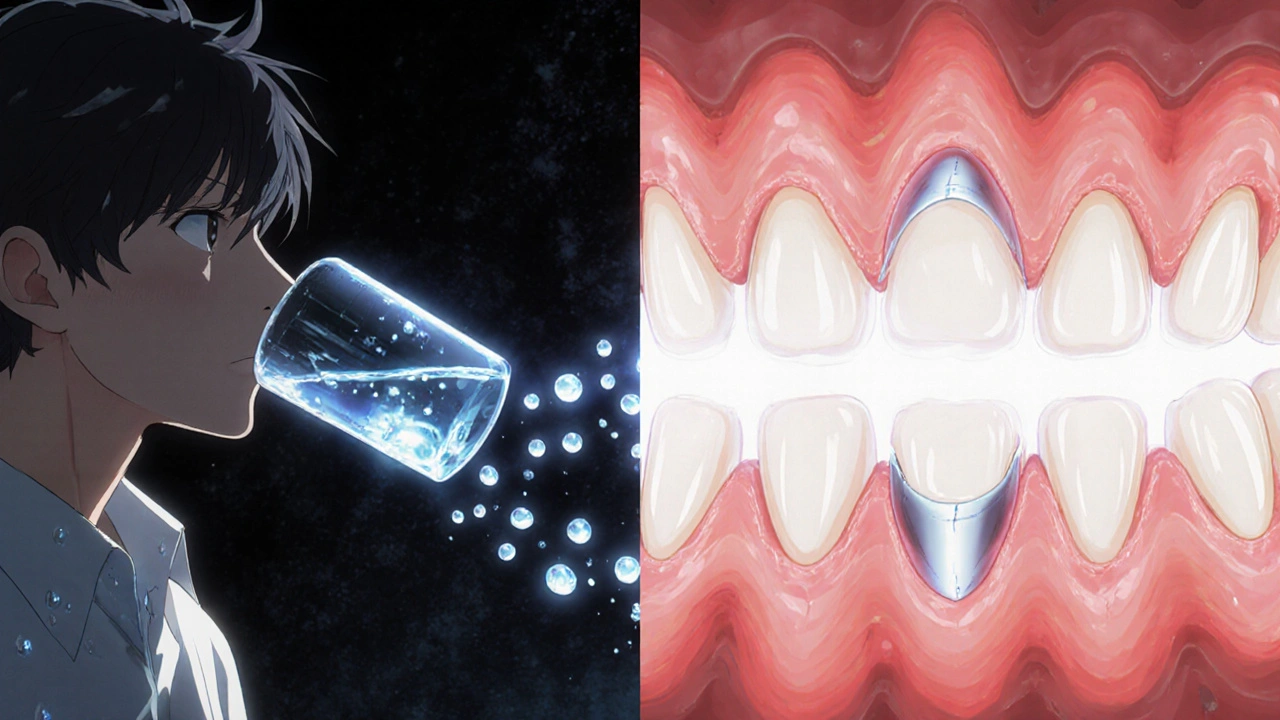
Ritonavir is a protease inhibitor, and while it blocks HIV from multiplying, it also affects how your body processes other substances. One big side effect is reduced saliva flow. Saliva isn’t just for comfort-it’s your mouth’s natural defense. It washes away food particles, neutralizes acids, and fights bacteria. When saliva drops, plaque builds up faster, gums swell, and cavities form more easily.
Studies show that up to 40% of people on ritonavir report dry mouth, and nearly 30% develop oral thrush-a fungal infection that looks like white patches on the tongue or inner cheeks. These aren’t rare accidents. They’re direct results of how ritonavir interacts with your immune system and oral microbiome.
Common Oral Side Effects You Should Watch For
- Oral thrush: White, creamy patches that bleed when scraped. Often mistaken for food residue.
- Dry mouth (xerostomia): Constant need to sip water, trouble swallowing dry foods, cracked lips.
- Bad taste or metallic flavor: Persistent even after brushing. Can reduce appetite and nutrition.
- Gum inflammation: Red, swollen, or bleeding gums-even without brushing too hard.
- Increased cavities: Especially near the gum line or on the roots of teeth.
These symptoms don’t always show up right away. Some people notice them after a few months. Others don’t see changes until a routine dental checkup reveals early bone loss around teeth. That’s why waiting for pain isn’t smart.
Five Daily Habits to Protect Your Teeth and Gums
Managing oral health on ritonavir isn’t about doing more-it’s about doing the right things consistently.
- Brush with fluoride toothpaste twice a day-but don’t rush. Spend two full minutes, especially along the gumline. Use a soft-bristled brush. Hard bristles can damage already sensitive gums.
- Floss daily-even if your gums bleed. That bleeding means plaque is there. Flossing removes it before it hardens into tartar. If traditional floss is hard to handle, try water flossers or interdental brushes.
- Use a saliva substitute or sugar-free gum-look for products with xylitol. Chewing gum for 10-15 minutes after meals stimulates saliva and reduces acid. Avoid sugary gums-they feed cavity-causing bacteria.
- Rinse with alcohol-free mouthwash-alcohol dries out your mouth even more. Choose one labeled for dry mouth or sensitive gums. Some contain chlorhexidine, which helps control thrush, but only use it if your dentist recommends it.
- Drink water constantly-keep a bottle with you. Sip all day, especially after taking your dose. Avoid sugary drinks, coffee, and energy drinks. They feed bacteria and worsen dryness.

What to Avoid
Some habits that seem harmless can make things worse.
- Don’t use mouthwashes with alcohol-they strip moisture and irritate sores.
- Avoid sticky snacks-candies, dried fruit, and granola bars cling to teeth and stay there for hours.
- Don’t skip dental cleanings-even if your mouth feels fine. You need professional cleanings every 3-4 months, not every 6.
- Don’t ignore bleeding gums-it’s not normal. It’s a sign of early gum disease, which can lead to tooth loss.
- Don’t use whitening products-they contain harsh abrasives and peroxides that can damage enamel already weakened by dry mouth.
When to See Your Dentist
Don’t wait for pain. Schedule an appointment if you notice:
- White patches that won’t wipe off
- Red, swollen gums that bleed easily
- Loose teeth or changes in how your bite feels
- Sores that last longer than two weeks
- Constant bad taste or smell that brushing doesn’t fix
Bring your medication list to every dental visit. Dentists need to know you’re on ritonavir because it affects healing and can interact with local anesthetics or antibiotics. Some dentists aren’t familiar with HIV meds-so be ready to explain.
Work With Your Medical Team
Your HIV provider and dentist should talk to each other. Ask your doctor if switching to another antiviral might help your mouth. Not everyone can switch, but some alternatives like darunavir or atazanavir have lower rates of oral side effects. If your current regimen is working well for your viral load, your doctor might suggest adding a saliva-stimulating medication like pilocarpine-though it’s not common.
Also, check your vitamin D and calcium levels. Low levels are common in people on long-term HIV treatment and can weaken jawbone and teeth. A simple blood test can tell you if you need supplements.
Real-Life Example: Maria’s Story
Maria, 52, started ritonavir in 2022. By 2024, she had three new cavities and painful thrush. She thought it was just aging. Then she saw a dentist who specialized in HIV care. The dentist found her saliva flow was 60% lower than normal. Maria started using a prescription-strength fluoride gel nightly, chewed xylitol gum after meals, and switched to a non-alcohol rinse. Within three months, her sores cleared. Her next checkup showed no new decay.
Her secret? Consistency. Not perfection. She didn’t brush perfectly every day-but she never skipped it.
Final Thoughts: Your Smile Matters
Oral health isn’t just about looks. It’s about eating, speaking, and feeling confident. Poor dental health can lead to infections that spread to your heart or lungs-especially risky if your immune system is already managing HIV. Taking care of your mouth isn’t an extra task. It’s part of your treatment plan.
Start today. Pick one habit from the list above and stick with it for a week. Then add another. You don’t need to fix everything at once. But if you do nothing, your mouth will keep getting worse. And that’s something you can control.
Can ritonavir cause permanent damage to teeth?
Ritonavir itself doesn’t directly destroy teeth, but the side effects-like dry mouth and reduced saliva-create conditions where cavities and gum disease can progress quickly. Without proper care, this can lead to permanent tooth loss or bone damage in the jaw. The damage isn’t from the drug alone, but from how it changes your mouth’s environment over time.
Is it safe to get dental work done while taking ritonavir?
Yes, it’s safe-but you must tell your dentist you’re on ritonavir. The drug can interact with certain antibiotics and painkillers, and it may slow healing after surgery. Your dentist may need to adjust medications or schedule procedures differently. Never skip telling your dental team about your HIV meds.
How often should I see a dentist if I’m on ritonavir?
Every 3 to 4 months. Standard 6-month visits aren’t enough. With reduced saliva and higher risk of infection, you need more frequent cleanings and checkups. Your dentist may recommend professional fluoride treatments or antimicrobial rinses to prevent decay and thrush.
Can I use over-the-counter dry mouth products?
Yes, but choose carefully. Look for products labeled for dry mouth that contain xylitol, carboxymethylcellulose, or hydroxyethylcellulose. Avoid anything with alcohol, sugar, or citric acid. Brands like Biotene, Oasis, or Xerostom are designed for people on medications like ritonavir. Always check with your pharmacist if you’re unsure.
Does switching HIV medications help with oral side effects?
Sometimes. Some newer HIV drugs, like darunavir or bictegravir, have lower rates of dry mouth and oral thrush. But switching isn’t always possible-it depends on your viral load, resistance history, and other health factors. Talk to your HIV specialist before making any changes. The goal is to keep your virus under control while improving your quality of life-including your oral health.









Comments (10)
Neil Mason
October 29, 2025 AT 05:15 AMBeen on ritonavir for 5 years and this post hit home. I used to hate flossing but now I do it every night like clockwork. Started using Biotene spray and my tongue doesn’t feel like sandpaper anymore. Also switched to a soft brush and stopped using Listerine. Big difference.
My dentist didn’t even know about the 3-4 month rule till I told her. Now she sends me reminders. You gotta be your own advocate.
Andrea Gracis
October 29, 2025 AT 22:46 PMi didnt even know dry mouth from meds could cause cavities like that. i thought it was just being thirsty. my gums have been bleeding for months and i just thought i was brushing too hard. wow. gonna try the xylitol gum today. thanks for this.
Matthew Wilson Thorne
October 31, 2025 AT 12:50 PMFluoride gel nightly? Overkill. Most people just need basic hygiene and hydration. The real issue is dental access, not toothpaste.
Also, ‘don’t ignore bleeding gums’-yes. But saying ‘see a dentist every 3 months’ is a clinic’s revenue strategy, not medical necessity.
April Liu
October 31, 2025 AT 13:44 PMYou’re not alone!! 💪 I was terrified to tell my dentist I was on HIV meds… but once I did, she gave me a free fluoride treatment and even called my doctor to coordinate care. That’s the kind of provider you want.
Start small-pick ONE thing. I did water sipping first. Then floss. Then xylitol gum. You got this. No perfection needed, just consistency. ❤️
Kika Armata
October 31, 2025 AT 19:17 PMLet’s be honest-this article is barely scratching the surface. The real problem is the pharmaceutical industry’s complete disregard for long-term mucosal health in antiretroviral design. Ritonavir is a metabolic disruptor, not just a protease inhibitor. It alters CYP3A4 kinetics, which cascades into salivary gland hypofunction, dysbiosis, and ultimately, periodontal bone resorption.
And yet, the ‘five daily habits’? Pathetic. You need molecular-level interventions: saliva flow modulators, probiotic oral biofilms, pH-neutralizing rinses with zinc lactate. Xylitol gum is a Band-Aid for a broken femur.
Also, ‘don’t use whitening products’? Obviously. But why stop there? Avoid all acidic beverages. Even sparkling water is erosive. And why is vitamin D mentioned as an afterthought? It’s foundational. You need serum levels above 50 ng/mL, not ‘check your levels.’
And Maria? Her story is anecdotal. We need longitudinal cohort studies. Until then, this is just wellness propaganda dressed as clinical guidance.
Sara Mörtsell
October 31, 2025 AT 20:56 PMEveryone’s so focused on brushing and flossing but no one talks about the real enemy: sugar. Even ‘healthy’ snacks-dates, granola, kombucha-they’re all sugar bombs. And the dental industry? They’ll sell you a $300 fluoride tray while ignoring that your coffee with 3 sugars is rotting your roots.
Also, why do we assume dentists know anything about HIV? My last one asked if I was ‘on the new pill’ like it was a trend. I had to explain protease inhibitors like I was talking to a 12-year-old.
And don’t get me started on ‘alcohol-free mouthwash’-most of those are just water with mint flavor. Use salt water. Free. Effective. No marketing BS.
Rhonda Gentz
November 1, 2025 AT 13:36 PMIt’s funny how we treat the mouth like it’s separate from the body. But it’s not. It’s the first organ of digestion, the mirror of immune health, the gateway to systemic inflammation. Ritonavir doesn’t ‘cause’ dry mouth-it reveals a vulnerability we’ve ignored for decades.
Saliva isn’t just moisture. It’s immunity in liquid form. Antibodies, lysozyme, lactoferrin-all silenced by this drug. We’re not fixing a symptom. We’re compensating for a systemic imbalance.
And yet, we still think brushing harder will fix it. We treat the body like a machine you can clean with toothpaste. But it’s not. It’s a conversation. Between you, your meds, your microbes, your history.
Maybe the real question isn’t ‘how to protect your smile’-but ‘how to listen to what your body is telling you.’
Alexa Ara
November 2, 2025 AT 09:36 AMI just started ritonavir last month and was freaking out about the dry mouth. This post gave me so much hope. I tried the xylitol gum today and it actually tasted good? Who knew?
Also, I started carrying a water bottle everywhere-even to bed. It’s weird but I feel like my tongue isn’t stuck to the roof of my mouth anymore. Small wins, right?
You’re all doing better than you think. Keep going. One sip, one brush, one day at a time.
Olan Kinsella
November 4, 2025 AT 05:27 AMThey say ‘your mouth is your mirror’… but what if your mirror is broken? What if the drug you take to live is slowly turning your smile into a graveyard of cavities and white patches?
I lost two teeth last year. Not from candy. Not from age. From silence. I didn’t tell anyone. Thought it was ‘just part of being sick.’
Now I carry Biotene everywhere. I floss like my life depends on it. And I scream at my dentist when she says ‘come back in six months.’
You think you’re alone? You’re not. But silence kills faster than the virus.
Kat Sal
November 4, 2025 AT 12:01 PMLove this. I’m a nurse and I’ve seen too many people ignore their mouths because they’re ‘focused on surviving.’ But surviving isn’t living if you can’t eat your favorite food or smile without shame.
Start with water. Then floss. Then gum. That’s it. Don’t overwhelm yourself. And if you slip? Just start again tomorrow. No guilt. No shame. You’re doing better than you know.