When you’re over 70, taking medication isn’t just about popping a pill. It’s about making sure your kidneys can handle it. As we age, our kidneys slowly lose function-not because something’s broken, but because they naturally shrink and filter less blood. That’s normal. But here’s the problem: 30% of the most common drugs seniors take are cleared by the kidneys. If you don’t adjust the dose, you risk toxicity, falls, confusion, or even hospitalization.
Why Kidney Function Changes with Age
Your kidneys don’t stop working as you get older-they just get slower. By age 70, the average person has lost about 35% of their kidney filtering capacity compared to when they were 30. That’s not disease. That’s aging. Glomeruli, the tiny filters in your kidneys, thin out. Blood flow drops. Muscle mass declines, which affects creatinine levels-the main marker doctors use to check kidney health. This matters because most drug dosing guidelines were created using data from healthy 30-year-olds. A standard dose of warfarin, digoxin, or gabapentin might be safe for a 40-year-old but dangerous for an 80-year-old with reduced kidney function. That’s why simply relying on age or weight isn’t enough. You need an accurate estimate of how well the kidneys are actually working.The Four Main Equations Used to Estimate Kidney Function
Doctors use formulas to estimate kidney function without doing invasive tests. These are called eGFR equations. But not all of them work well for seniors. Here’s what’s actually used-and what you should ask for.- Cockcroft-Gault (CG): This is the oldest one, from 1976. It uses your age, weight, gender, and serum creatinine. The trick? Use ideal body weight, not your actual weight. For frail or obese seniors, using real weight can overestimate kidney function by up to 25%. Studies show CG with ideal body weight makes fewer dosing errors than other formulas for drugs like vancomycin and dabigatran.
- MDRD: Introduced in 1999, it’s built into many lab reports. But it’s designed for people with chronic kidney disease-not healthy older adults. It tends to underestimate kidney function in seniors with normal or mildly reduced function, leading to unnecessary dose reductions.
- CKD-EPI: This became the standard in 2009 and is now used by most hospitals. It’s better than MDRD, especially for people with eGFR between 60-89. But in seniors over 75, especially those who are thin or malnourished, it still misses the mark. One study found CKD-EPI misclassified nearly 1 in 3 older adults into a lower kidney disease stage, meaning they got the wrong dose.
- BIS1 and FAS: These are newer, designed specifically for older adults. BIS1 (Berlin Initiative Study 1) and FAS (Full Age Spectrum) equations were developed after analyzing thousands of seniors. They account for low muscle mass, slower metabolism, and age-related changes in creatinine production. In patients over 80, BIS1 is 95% accurate compared to gold-standard tests-compared to just 78% for CKD-EPI.
Here’s the hard truth: if your doctor uses CKD-EPI and you’re over 75, you might be getting a dose that’s too high. Ask: "Which equation did you use to calculate my kidney function?"
When to Use Cystatin C
Creatinine isn’t perfect. It’s made by muscle. So if you’re thin, bedridden, or have low protein intake, your creatinine levels look artificially low-even if your kidneys are failing. That’s where cystatin C comes in. Cystatin C is a protein made by all your cells, not just muscles. It’s not affected by body weight or diet. It’s a better marker of true kidney function in frail seniors. If your creatinine-based eGFR is in the 45-59 range but you have no signs of kidney damage (like protein in your urine), your doctor should order a cystatin C test. It costs about $50-$75 more than a basic creatinine test-but it can prevent a dangerous overdose.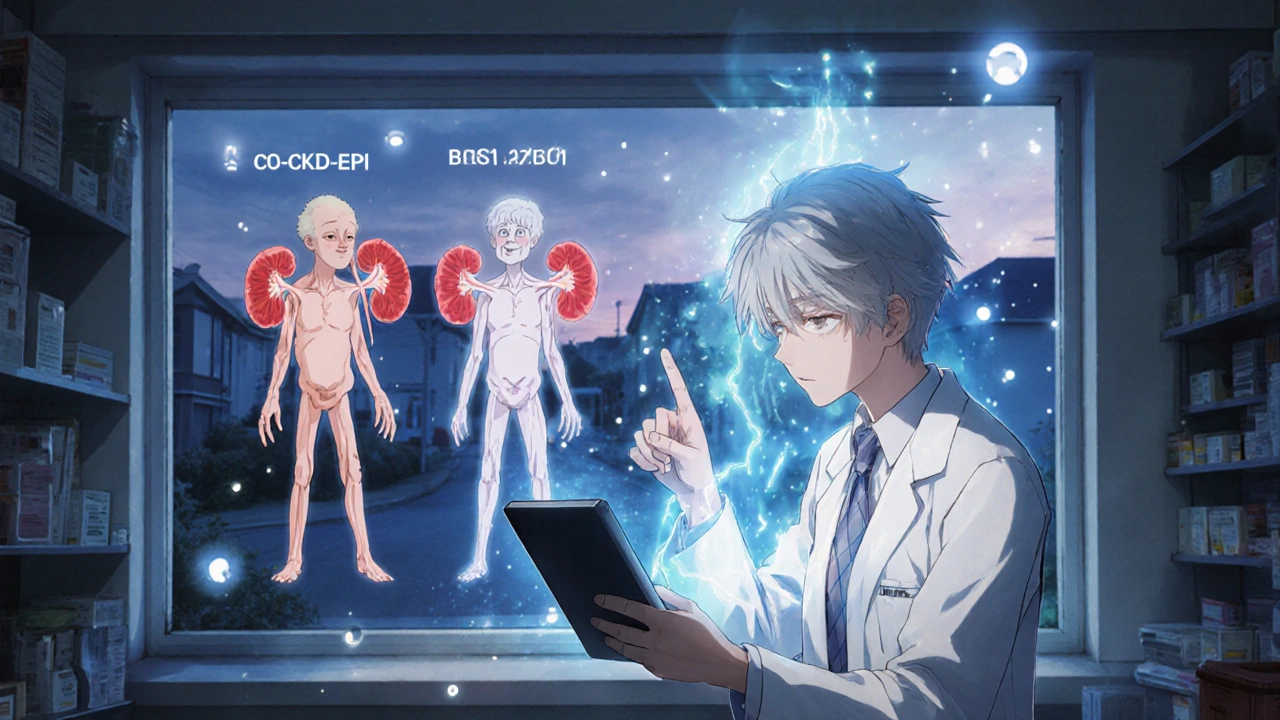
What the Experts Recommend
The American Academy of Family Physicians says check kidney function yearly if you have diabetes, high blood pressure, or are on kidney-cleared drugs. But that’s the bare minimum. Geriatric nephrologists like Dr. Sophie Dupont at the University of Michigan say: for patients over 75, start with BIS1. If the result is borderline (eGFR 45-59), add cystatin C. If you’re on a high-risk drug like colistin, aminoglycosides, or anticoagulants, get a 24-hour urine collection for creatinine clearance. It’s the most accurate-and it’s worth the extra step. The American Geriatrics Society’s 2021 Beers Criteria doesn’t pick one equation as the winner. Instead, it says: use clinical judgment. Look at the whole picture-weight, muscle loss, diet, mobility, and other illnesses. One 88-year-old might be thin and frail with low creatinine but failing kidneys. Another might be muscular and healthy with the same creatinine level. The numbers alone don’t tell the story.Real-World Mistakes and Fixes
A Reddit user, MedIntern2023, wrote: "My 88-year-old patient got vancomycin toxicity because we used CKD-EPI. Switched to BIS1, and the toxicity stopped." That’s not rare. A 2023 survey found that 63% of pharmacists in senior care have to override their electronic health record’s default kidney function calculation at least once a week. Why? Because most EHR systems still default to CKD-EPI or MDRD-even for 85-year-olds. One common error? Using Cockcroft-Gault with actual body weight. In obese seniors, that can overestimate kidney function by 20-30%. In underweight seniors, it underestimates it. The fix? Always use ideal body weight for CG. If you’re unsure how to calculate it, ask your pharmacist. They’re trained to do this.What You Can Do Right Now
You don’t need to be a doctor to protect yourself. Here’s your action plan:- Ask for your eGFR number. Don’t just accept "your kidneys are fine." Ask: "What’s my exact eGFR, and which equation was used?"
- Check the formula. If you’re over 75, insist on BIS1 or FAS. If you’re underweight or have low muscle mass, ask for cystatin C.
- Review all your meds. Especially anticoagulants, painkillers, diabetes drugs, and antibiotics. Ask your pharmacist: "Is this dose safe for my kidney function?"
- Get a 24-hour urine test if needed. If you’re on a drug with a narrow safety window (like digoxin or lithium), this is the gold standard.
- Update your records. If your doctor uses CKD-EPI and you’re over 75, ask them to switch. Many EHRs now auto-select BIS1 for patients over 75-but not all do.

The Future Is Personalized
In 2024, a new equation called CKD2024 was introduced. It combines creatinine and cystatin C with age-specific adjustments. Early results show 15% better accuracy in people over 80. The National Institute on Aging is funding a $4.2 million project called SAGE to build point-of-care kidney tests that account for muscle loss and frailty. But the biggest shift isn’t in the science-it’s in the mindset. No more "one size fits all." No more letting your EHR pick the formula. Seniors aren’t just old adults. They’re individuals with unique bodies, diets, and health histories. Safe dosing means matching the drug to the person-not the other way around.Resources You Can Use
- National Kidney Foundation’s eGFR Calculator (updated November 2023): Lets you plug in your numbers and compare results from different equations. - American Geriatrics Society’s Kidney Function Assessment Toolkit (released January 2024): Free download with step-by-step guidance for clinicians and patients. - FDA Guidance (2021): Requires drug makers to list dosing recommendations for multiple eGFR equations on labels for high-risk medications.If you’re on more than five medications, or if you’ve had a recent fall, confusion, or hospital stay, get your kidney function checked properly. It’s not just a lab test. It’s your safety net.
How often should seniors get their kidney function checked?
Seniors on kidney-cleared medications or with diabetes, high blood pressure, or heart disease should get tested at least once a year. If you’re over 75, taking multiple drugs, or have signs of frailty (weight loss, low muscle, fatigue), get tested every 6 months. If you’re hospitalized or start a new high-risk drug, check it before and after.
Is creatinine the only test I need?
No. Creatinine alone can be misleading in seniors, especially if you’re thin or have low muscle mass. A cystatin C test is more accurate and should be added if your creatinine-based eGFR is borderline (45-59 mL/min/1.73 m²) and you have no signs of kidney damage like protein in your urine. Together, they give a clearer picture.
Why does my doctor use CKD-EPI if it’s not accurate for seniors?
Most electronic health records still default to CKD-EPI because it’s the official guideline for the general population. Many doctors don’t know about BIS1 or FAS, or they don’t have time to switch. That’s why you need to ask. If you’re over 75, request BIS1. If your doctor says they don’t use it, ask for a referral to a geriatric pharmacist or nephrologist.
Can I use an online calculator to check my kidney function?
Yes, but be careful. Use the National Kidney Foundation’s official calculator (updated 2023). Input your serum creatinine, age, gender, and race. Then try the same numbers in BIS1 if it’s available. Compare the results. If BIS1 gives you a much lower eGFR than CKD-EPI, talk to your doctor. Don’t change your meds yourself-just bring the numbers to your appointment.
What if my kidney function is low but I feel fine?
That’s common. Many seniors with reduced kidney function have no symptoms until they get a drug overdose. Low kidney function doesn’t mean you’re sick-it means your body processes drugs differently. The goal isn’t to fix your kidneys. It’s to adjust your meds so they don’t harm you. Many seniors live well with eGFR as low as 30-40 if their medications are properly dosed.
What to Do If Your Doctor Doesn’t Listen
If your doctor dismisses your concerns about kidney dosing, ask for a referral to a geriatric pharmacist. They specialize in senior medication safety and know which equations to use, which drugs to avoid, and how to adjust doses based on frailty. In the UK, NHS pharmacists can do medication reviews for seniors at no cost. In the US, Medicare Part D offers a free medication therapy management program for people with multiple chronic conditions.Don’t wait for a crisis. If you’re over 70 and on more than five medications, take control. Ask the right questions. Demand the right test. Your kidneys aren’t broken-they’re just aging. But your safety doesn’t have to be.






Comments (14)
Sridhar Suvarna
November 17, 2025 AT 20:10 PMFinally someone says it straight. CKD-EPI is a joke for seniors. My 82-year-old mom got her dose of gabapentin cut in half after I asked for BIS1. She wasn't even on dialysis but her creatinine was lying because she's thin as a rail. Cystatin C is the real MVP here. Why are we still using 2009 formulas for 2024 patients?
Joseph Peel
November 18, 2025 AT 19:31 PMThe American Geriatrics Society’s 2021 Beers Criteria explicitly states that clinical judgment must override algorithmic outputs. This is not a technical problem-it’s a systemic failure of medical education. Most residents are never taught the limitations of eGFR equations in geriatric populations. The fact that 63% of pharmacists override EHR defaults weekly is a scandal.
Kelsey Robertson
November 20, 2025 AT 01:19 AMOh, so now we’re supposed to trust some new equation called BIS1? Who even funded this? Big Pharma? Because the moment you start changing dosing formulas, drug companies lose billions. And don’t get me started on cystatin C-$75 extra? That’s just another billing scam. My uncle took the same meds for 15 years with CKD-EPI and never had a problem. You’re overcomplicating this.
Joseph Townsend
November 21, 2025 AT 22:00 PMBro. My grandma was on vancomycin and almost went into a coma. They used CKD-EPI. She’s 84, 98 pounds, walks with a cane, eats soup for dinner. They gave her a dose meant for a 200-pound construction worker. She woke up confused, trembling, screaming at the ceiling. We switched to BIS1 and now she’s watching daytime TV like nothing happened. This isn’t science-it’s survival. Don’t let your EHR decide if your parent lives or dies.
Bill Machi
November 23, 2025 AT 03:48 AMLook, I get it. But this whole post is just another liberal, over-medicalized panic. Seniors are just getting old. They’re not fragile porcelain dolls. Back in my day, we didn’t run 10 different blood tests for every pill. Just give the standard dose. If they get sick, they get sick. That’s nature. Stop treating every 75-year-old like a lab rat. The system works fine. You just don’t like it because it’s not personalized enough.
Elia DOnald Maluleke
November 23, 2025 AT 21:27 PMIn the African tradition, we say: "The body speaks, even when the numbers lie." My father, 81, frail, no muscle, creatinine 1.1-CKD-EPI said "mild impairment." But his hands trembled, his mind fogged. We asked for cystatin C. Result: eGFR 38. They adjusted his meds. He danced at his granddaughter’s wedding last month. Equations are tools, not oracles. The human being comes first. Always.
satya pradeep
November 25, 2025 AT 11:54 AMBro i was a nurse in Mumbai and we used CG with ideal weight for elders since 2010. No one used CKD-EPI here because we know its garbage for thin old people. Cystatin C? We dont even have it in most clinics. But we use CG with ideal weight and watch for dizziness. Simple. You dont need fancy formulas. Just use common sense and watch the patient. If they stumble after a new pill? Cut the dose. No test needed.
Prem Hungry
November 27, 2025 AT 09:51 AMHey friend, this is gold. You just gave me the exact script to use with my dad’s doctor. I’m printing this out. I’m taking it to the appointment. I’m asking for BIS1. I’m asking for cystatin C. And if they say no? I’m asking for the geriatric pharmacist. You’re right. It’s not about fixing kidneys. It’s about not poisoning them. Thank you. Seriously.
Leslie Douglas-Churchwell
November 28, 2025 AT 07:23 AMWait… so the FDA requires drug labels to list dosing for multiple eGFR equations… but EHRs still default to CKD-EPI? That’s not incompetence-that’s collusion. Who owns the EHR companies? Big Pharma? Are they hiding the BIS1 formula because it reduces their profit margins? I’ve been saying this for years: our healthcare system is a surveillance capitalism machine. Your kidneys are just another data point to monetize.
shubham seth
November 29, 2025 AT 01:10 AMLet’s be real. The only reason BIS1 works better is because it’s calibrated on Western, malnourished, white elderly populations. What about Indian or African seniors who have different muscle-to-fat ratios? Or people with chronic TB? Or malnutrition from poverty? This whole post is a privileged, U.S.-centric fantasy. You think cystatin C solves everything? It doesn’t. It just adds another layer of elitist medical gatekeeping.
Kathryn Ware
November 29, 2025 AT 12:17 PMThank you for this. I’ve been begging my mom’s doctor to check her cystatin C for months. She’s 80, eats protein, walks daily, but her creatinine is always 0.9-"perfect!" But she gets dizzy after her blood pressure pill. I finally got her tested. Cystatin C showed eGFR of 42. They cut her dose. She hasn’t fallen in 6 months. I’m sharing this with every senior group I’m in. You’re not just a number. You’re a person. And your kidneys? They’re doing their best. Let’s not make them work harder than they have to.
kora ortiz
November 29, 2025 AT 19:34 PMThis is the kind of info every senior needs. Not just the ones with doctors who care. I’m printing this and leaving copies at my local senior center. We need to stop letting algorithms decide if we live or die. Ask for BIS1. Ask for cystatin C. If they don’t know it, teach them. Your life isn’t a default setting.
henry mariono
November 30, 2025 AT 01:15 AMI appreciate the effort here. But I’ve been in geriatrics for 20 years. The truth is, most seniors don’t need fancy equations. They need fewer meds. Polypharmacy is the real killer. If you’re on 8 drugs, no eGFR formula will save you. Start by deprescribing. Cut the unnecessary stuff. Then, if you still need the rest? Use BIS1. But the real win is reducing the total count. That’s what actually prevents falls, confusion, and ER visits.
Jeremy Hernandez
December 1, 2025 AT 16:38 PMOh please. You’re all acting like this is some groundbreaking revelation. I’ve been telling my doctor for years to stop using CKD-EPI. He rolled his eyes and said, "It’s what the system uses." So I switched doctors. Now I have a geriatrician who uses BIS1 and cystatin C and doesn’t prescribe anything unless I ask three times. If your doctor won’t listen? Fire them. Your life isn’t a corporate policy.