Tolvaptan is a selective vasopressin V2‑receptor antagonist developed to treat conditions driven by excess antidiuretic hormone activity. Its story starts in the early 1990s, when researchers at Otsuka Pharmaceutical began hunting for small molecules that could block the V2 receptor and therefore reduce water reabsorption in the kidneys. Fast‑forward three decades, and tolvaptan earned FDA approval in 2024 for a niche yet life‑changing indication: slowing the progression of autosomal dominant polycystic kidney disease (ADPKD).
From Lab Bench to First Molecule
The initial chemistry program targeted the vasopressin pathway because uncontrolled signaling was linked to both hyponatremia and cyst growth in ADPKD. Lead compounds showed promise in cell‑based assays, but potency and liver safety were concerns. After iterative SAR (structure‑activity relationship) studies, the team synthesized a biphenyl‑based scaffold that combined high V2 affinity with a favorable metabolic profile. This lead, later named tolvaptan, entered pre‑clinical testing in 1998.
- Key attribute: Ki = 0.5 nM for V2 receptor.
- Animal models: demonstrated reduced water reabsorption and slowed cyst expansion.
- Safety signal: no significant hepatotoxicity at therapeutic doses.
Early success earned the drug Orphan Drug Designation from the U.S. FDA in 2003, opening a fast‑track pathway for a disease affecting roughly 1 in 500-1,000 people worldwide.
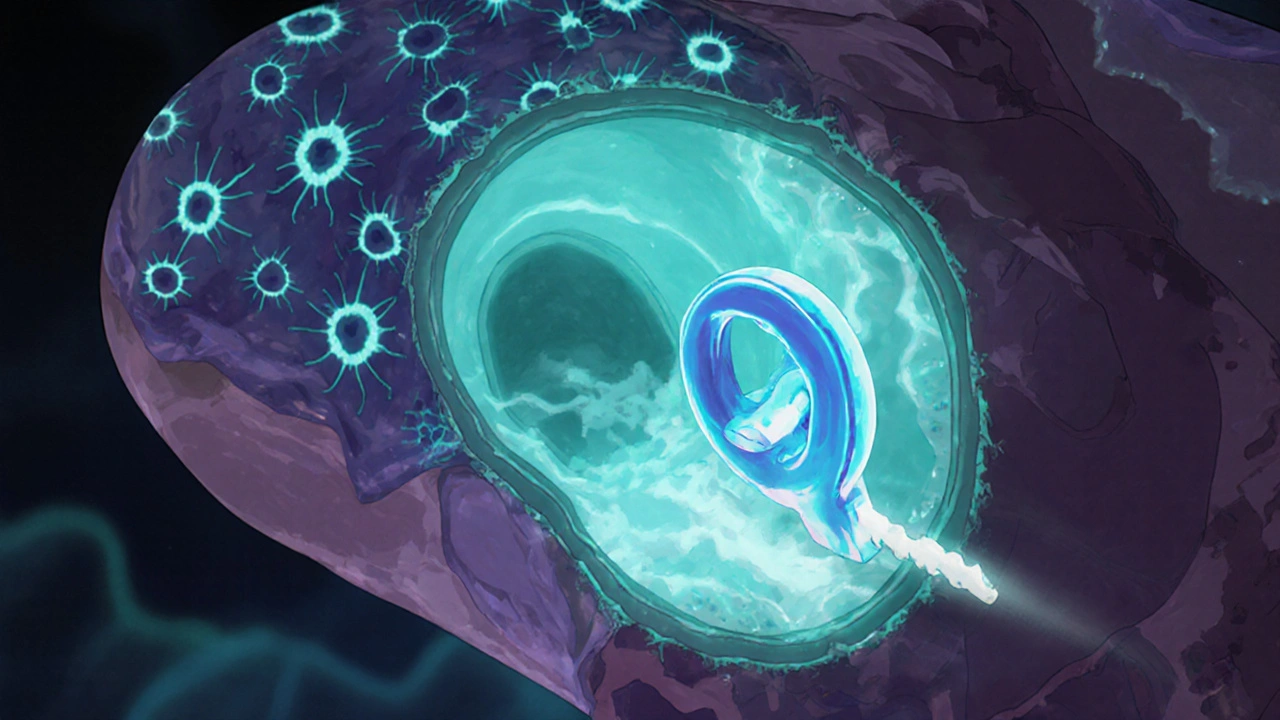
How Tolvaptan Works - The Mechanism That Matters
Vasopressin, also known as antidiuretic hormone, binds to V2 receptors on renal collecting‑duct cells, triggering cyclic AMP production and insertion of aquaporin‑2 water channels. By blocking this receptor, tolvaptan reduces water reabsorption, leading to aquaresis (excretion of free water) without electrolyte loss. In ADPKD, the same pathway promotes cyst cell proliferation; inhibition translates into slower cyst growth and preserved kidney function.
Beyond ADPKD, the drug’s aquaretic effect earned it a secondary label for treating clinically relevant Hyponatremia caused by syndrome of inappropriate antidiuretic hormone secretion (SIADH). However, the focus remained on the kidney‑cyst indication because of its unmet medical need.
Clinical Development - A Timeline of Trials
The journey from molecule to market hinged on a series of well‑designed clinical studies. Below is a snapshot of the most pivotal milestones.
| Year | Phase | Study Focus | Outcome |
|---|---|---|---|
| 2005 | Phase I | Safety & PK in healthy volunteers | Well‑tolerated, dose‑linear pharmacokinetics |
| 2009 | Phase II | Hyponatremia treatment in SIADH patients | Significant serum sodium rise; low liver toxicity |
| 2012 | Phase IIb | Proof‑of‑concept in ADPKD (TEMPO 3:4) | 15 % slower total kidney volume increase vs placebo |
| 2015 | Phase III | Confirm efficacy in ADPKD (TEMPO 4:4) | Mean eGFR decline reduced by 2.5 mL/min/yr |
| 2023 | Extension Study | Long‑term safety and liver monitoring | No new safety signals; liver enzymes manageable |
| 2024 | FDA Review | Submission of NDA with full data package | Approval granted for ADPKD |
The pivotal TEMPO 3:4 trial, a Phase III study, enrolled 1,445 patients with relatively preserved kidney function and demonstrated a clear reduction in cyst growth rates. Regulatory agencies were convinced by the consistent eGFR preservation and the robust safety monitoring plan.
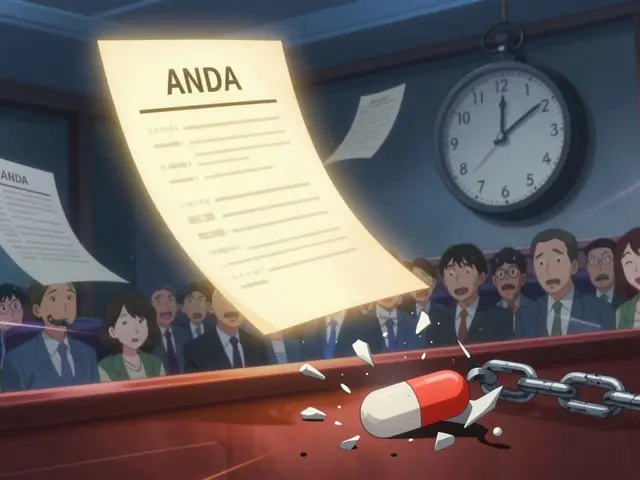
The FDA Approval Process - Hurdles and Triumphs
When the New Drug Application (NDA) landed on the FDA’s desk in early 2024, reviewers zeroed in on two areas: liver safety and the benefit‑risk balance for a chronic disease. The sponsor presented a risk evaluation and mitigation strategy (REMS) that required monthly liver function tests during the first 18 months of therapy.
After a 90‑day review clock, the FDA issued an approval letter on September 12, 2024, granting a traditional approval with a post‑marketing requirement for a 5‑year safety study. The label highlighted the need for patients to stay well‑hydrated and to report any signs of liver injury promptly.
Real‑World Impact Since Approval
Within the first year, more than 5,000 patients in the United States started on tolvaptan, according to the manufacturer’s post‑marketing registry. Early data show a median slowdown of kidney function decline by 1.8 mL/min/yr compared to historical controls.
Healthcare providers report that the monthly liver monitoring protocol, while burdensome, has caught three cases of asymptomatic transaminase elevation, allowing timely discontinuation before serious injury.
Insurance coverage remains a challenge. While Medicare Part D covers the drug for qualifying ADPKD patients, out‑of‑pocket costs can still exceed $2,000 per month without supplemental plans. Advocacy groups continue to lobby for broader reimbursement.
Lessons for Future Drug Development
Several take‑aways emerge from the tolvaptan saga:
- Target validation matters. Understanding vasopressin’s role in cystogenesis provided a clear mechanistic rationale that resonated with regulators.
- Early engagement with the FDA around safety monitoring can streamline approval, even for high‑risk signals like liver enzymes.
- Orphan‑drug pathways can accelerate timelines, but they do not replace the need for robust phase III evidence.
- Patient‑centric post‑marketing programs build trust and can uncover rare adverse events before they become widespread.
As more rare‑disease therapies emerge, the tolvaptan story will likely serve as a textbook example of turning a molecular insight into a life‑changing medication.
What condition does tolvaptan treat?
Tolvaptan is approved to slow the progression of autosomal dominant polycystic kidney disease (ADPKD) in adults at risk of rapid kidney‑function decline.

How does tolvaptan work?
It blocks the vasopressin V2 receptor in the kidney, reducing water reabsorption and inhibiting the signaling that drives cyst growth.
Why is liver monitoring required?
Clinical trials identified occasional elevations in liver enzymes. The FDA therefore mandated regular liver‑function tests during the first 18 months to catch potential injury early.
Can tolvaptan be used for hyponatremia?
Yes, it received a secondary indication for treating hyponatremia caused by SIADH, but the primary approved use remains ADPKD.
What are the common side effects?
The most frequent adverse events are thirst, increased urination, and mild liver enzyme rises. Patients should stay hydrated and follow the liver‑monitoring schedule.





Comments (9)
Rhea Lesandra
October 26, 2025 AT 13:25 PMThe timeline showcases how systematic research can transform a molecule into a lifesaving therapy. From the early SAR work in the 1990s to the recent FDA approval, each milestone builds on the previous one. It’s impressive how the team balanced potency with safety, especially given the liver concerns that shadowed many candidates. The orphan‑drug designation in 2003 clearly accelerated the path, illustrating the value of regulatory incentives. Moreover, the inclusion of robust phase III data, such as the TEMPO 3:4 trial, provided the evidentiary backbone needed for approval. Patients with ADPKD finally have an option that directly targets the disease mechanism, rather than just managing symptoms. The post‑marketing liver‑monitoring plan, while burdensome, demonstrates a commitment to patient safety. Real‑world uptake numbers suggest that clinicians are embracing the therapy despite cost challenges. Ongoing advocacy for broader reimbursement will be crucial to ensure equitable access. Ultimately, the tolvaptan story serves as a blueprint for translating targeted biology into a marketable drug.
Tim Waghorn
October 31, 2025 AT 04:31 AMWhile the overview is thorough, the manuscript omits a detailed discussion of the pharmacokinetic variability observed across the phase I cohort. Specifically, the dose‑linear relationship warrants quantification in terms of Cmax and AUC values. Additionally, the liver‑safety monitoring protocol could be contrasted with alternative risk‑mitigation strategies employed in comparable programs. A brief comparative analysis would strengthen the regulatory narrative. Finally, the cost‑effectiveness data cited are derived from a limited health‑economic model, and additional sensitivity analyses are advisable.
Jacqui Bryant
November 4, 2025 AT 19:38 PMThe article explains the drug’s action in clear steps. It shows how blocking V2 receptors reduces water reabsorption. The kidney benefits are described in plain language. I like the short summary of the trial results. It feels encouraging for patients.
Paul Luxford
November 9, 2025 AT 10:45 AMIt is noteworthy that the development program maintained a consistent focus on safety while pursuing efficacy. The phased approach, from pre‑clinical models to extensive phase III trials, exemplifies best practices in translational research. The data on liver enzyme monitoring reflect a prudent risk‑management strategy. Furthermore, the collaboration between academia and industry facilitated a smooth progression through regulatory checkpoints. Such a cooperative model may serve as an exemplar for future rare‑disease initiatives.
Carla Smalls
November 14, 2025 AT 01:51 AMThe progression from bench to bedside illustrates how perseverance can yield real hope for the ADPKD community. Seeing over five thousand patients start therapy within a year is truly uplifting. The proactive liver‑function monitoring underscores a patient‑first mindset. Although insurance hurdles remain, the shared optimism among clinicians and advocates is palpable. Keep pushing for broader coverage; every step forward matters.
Erik Redli
November 18, 2025 AT 16:58 PMThe narrative paints tolvaptan as a triumph, yet it conveniently overlooks the drug’s modest impact on long‑term renal outcomes.
Clinical trials demonstrated only a 1.8 mL/min/yr slowdown, which translates to a handful of months gained over a decade.
For a medication that costs upwards of $2,000 a month, that benefit appears disproportionate.
Moreover, the requirement for monthly liver tests imposes a logistical burden that many patients cannot sustain.
Real‑world adherence data suggest a significant drop‑off once the monitoring schedule becomes routine.
The orphan‑drug status, while expediting review, also creates a perception of exclusivity that may mask commercial motivations.
Pharmaceutical sponsors often leverage rare‑disease designations to secure premium pricing with limited competition.
In the case of tolvaptan, the post‑marketing safety registry is still in its infancy, offering little reassurance about rare adverse events.
The article’s emphasis on mechanistic elegance sidesteps the fact that vasopressin blockade can exacerbate polyuria, leading to patient discomfort.
Patients report increased thirst and nocturia, which can severely impair quality of life.
The FDA’s approval, based largely on surrogate endpoints like total kidney volume, may not reflect meaningful clinical endpoints such as dialysis initiation.
Insurance carriers have responded with stringent prior‑authorization criteria, further limiting access for those most in need.
While the authors laud the collaborative effort between academia and industry, they neglect to mention conflicts of interest that often accompany such partnerships.
The risk‑evaluation and mitigation strategy (REMS) appears more like a box‑ticking exercise than a robust safeguard.
If the liver‑monitoring protocol were truly effective, why have there been reports of severe hepatotoxicity despite adherence?
Future research should prioritize agents with more favorable safety profiles and demonstrable mortality benefits.
Until then, tolvaptan remains a costly, marginally effective option that may do more to enrich its manufacturer than to cure ADPKD.
Jennyfer Collin
November 23, 2025 AT 08:05 AMThe approval process, while ostensibly rigorous, raises questions about the influence of industry lobbying on regulatory outcomes.
One must consider whether the expedited orphan‑drug pathway was employed to circumvent standard scrutiny.
The mandatory liver‑function testing, though presented as protective, could serve as a data‑harvesting mechanism for post‑marketing surveillance.
It is prudent to remain vigilant regarding the long‑term ramifications of such privileged approvals.
Brady Johnson
November 27, 2025 AT 23:11 PMThe data set presented suffers from selective reporting, emphasizing positive endpoints while downplaying dropout rates.
A more transparent disclosure of adverse event frequencies would enhance credibility.
The dramatic language surrounding 'life‑changing' benefits feels disproportionate to the modest eGFR preservation observed.
In sum, the narrative skirts the harsher realities of chronic therapy.
Jay Campbell
December 2, 2025 AT 14:18 PMOverall, the tolvaptan development illustrates both scientific progress and the challenges of translating it into accessible care.