“Chloroquine.” The word probably sparks instant memories—if you’re old enough—of malarial fever and warnings about tropical travel. For those more up to date with news headlines, chloroquine is the same stuff that set off a worldwide frenzy in the early days of the Covid-19 pandemic. But where do hype and hysteria stop, and where does reality begin? Here’s what’s real, what’s rumor, and why this little chemical salt finds itself at the center of so many heated debates, even 80 years after its discovery.
What Is Chloroquine, And Why Was It Invented?
Chloroquine has been around—believe it or not—since the 1930s. This compound didn’t fall out of a lab by accident. Researchers were in a fierce race to replace natural quinine, the classic malaria treatment pulled from tree bark, because quinine was expensive and sometimes deadly. Chloroquine and its cousin hydroxychloroquine were synthetic breakthroughs. Imagine a scenario: a traveler in the 1950s bites by a mosquito, fevers up, and out comes chloroquine—the world’s new weapon against malaria. The pill worked. It wasn't perfect, but it was cheap, easy to use, and—get this—even made its way onto the World Health Organization’s List of Essential Medicines. That’s a short list of drugs every health system needs ready at all times.
But why did mosquitoes ruin the party? Over time, repeated and poorly managed use of chloroquine led to resistance. Plasmodium falciparum, the nastiest version of the malaria parasite, mutated enough to shrug off its effects in much of Africa and Southeast Asia. Before resistance became a crisis, though, chloroquine had helped millions. In fact, by the 1980s, more than a billion doses a year hit the world market. It even served as an anti-inflammatory for rheumatoid arthritis and lupus patients. The “miracle” claims weren’t new; the controversies just kept changing faces.
Through the decades, chloroquine has kept its place as a sort of medical legend. French explorer Jacques Cousteau reportedly carried it on his expeditions (and used it to much personal benefit). Even today, in regions where malaria responds to chloroquine, health ministries rely on it as first-line therapy because it’s reliable, cheap (sometimes less than $0.10 a dose), and well-understood after so many years. It’s more than just a drug; it’s a symbol of the evolution of modern medicine.
The Real Medical Uses of Chloroquine
The one area where no headline can mess with facts—chloroquine is first and foremost an antimalarial. Ask doctors in South America, parts of the Middle East, and even some Caribbean islands: when a patient comes in shivering with malaria, and the local parasites haven’t grown resistant, chloroquine is still their go-to. This isn’t just old doctors set in their ways—they often choose chloroquine because it’s effective, affordable, and can obliterate the Plasmodium vivax and Plasmodium ovale parasites better than most newer meds.
But here’s something people often miss: chloroquine isn’t just about malaria. Years before social media giants started worrying about fact-checking, rheumatologists in the US and Europe were prescribing the drug to people with lupus and rheumatoid arthritis. Why? Its anti-inflammatory properties tamp down on the immune system run wild. For some, it was the difference between moving their fingers in the morning or not. Even today, about 5% of US prescriptions for chloroquine and its sibling hydroxychloroquine go to autoimmune disease, not infection. Still, malaria is where chloroquine’s story always circles back—because that’s where the risks and rewards matter most.
Need a quick overview of where it’s most useful? Check out this simple table:
| Condition | Effectiveness | Notes |
|---|---|---|
| Malaria | High (if no resistance) | Main use, especially P. vivax and P. ovale |
| Lupus | Moderate | Used as an immune modulator |
| Rheumatoid Arthritis | Variable | Usually combined with other drugs |
| Covid-19 | Not recommended | Failed in clinical trials |
For anyone considering this drug, direct information is key. No matter how cheap or old a medication is, it only works where it’s supposed to. Chloroquine is no exception and shouldn't be used for conditions outside proven ones unless a doctor’s calling the shots—and that brings us to the most recent firestorm: Covid-19.

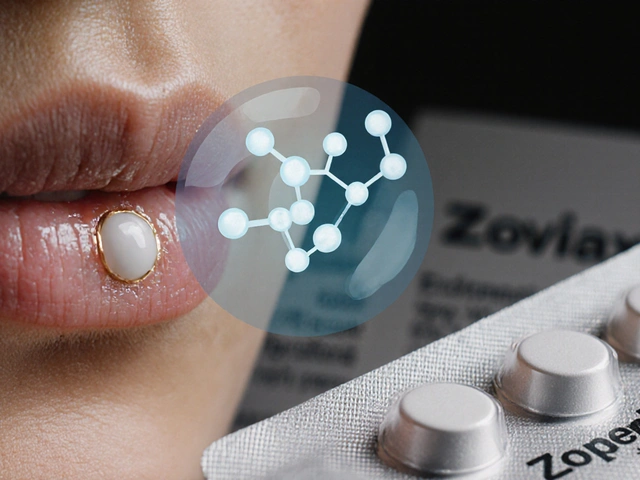
Covid-19, Controversy, and the Chloroquine Craze
Let’s cut to the chase. In early 2020, when the world was scrambling for any hope against Covid-19, chloroquine—and even more so, hydroxychloroquine—became household names, not because of new research, but because of speculation, rumors, and viral tweets. Certain high-profile leaders praised the drug. Suddenly, pharmacists got swamped by folks demanding a medication that, for the virus, hadn’t even been fully studied yet. In some countries, stocks of the drug vanished overnight. Some desperate people bought chloroquine meant for aquarium cleaning.
But did it work for Covid-19? Not really. Major clinical trials like the RECOVERY trial in the UK, the US National Institutes of Health studies, and efforts run in Brazil looked for evidence. The best answer after all that data? No significant difference in patients who took the drug versus those who didn’t. Worse, the risks climbed for certain groups. Abnormal heart rhythms became a concern, especially when doctors tried mixing chloroquine with other antivirals or antibiotics. The FDA, after a quick initial green light under emergency use, slammed the brakes and recommended against general use for Covid-19.
This isn’t just stuffy research talk—people actually got hurt. Data from CDC poison control centers showed calls about chloroquine exposures doubled in the weeks after it hit the headlines. If you want a cautionary tale on viral misinformation, this drug wrote the book. Since then, chloroquine’s back on the shelf for Covid-19, at least in the US and EU. It remains a stark lesson: even familiar drugs come with unknown risks when used out of their specialty zone.
Still, some good came out of all the noise. The pandemic reminded a lot of folks—patients and doctors alike—that off-label use is both powerful and dangerous. The trust that chloroquine built for malaria over decades? It doesn’t translate instantly to new diseases. Even so, research continues. Labs haven’t given up looking for fresh uses for this molecule. But for now, if someone claims chloroquine is a magic bullet? That’s hype, not help.
Side Effects, Risks, and Safe Use Tips
Chloroquine is not candy. Just because it’s old doesn’t mean it’s safe for everyone. The most common side effects? A bitter taste in your mouth (no surprise—just try crushing a tablet), mild nausea, and a tendency to upset your belly. Still, those are manageable for most. What matters more are the big risks if you take too much or have certain conditions.
The biggest scares show up in the heart and the eyes. Chloroquine, especially after months or years of use, can damage the retina, leading to permanent vision loss. The chance isn’t huge, but it’s serious enough that eye checks—think of them as your insurance policy—are essential for anyone on long-term treatment. Forget those, and you might not realize anything’s wrong until your sight’s already fading.
Heart rhythms are the other danger zone. Chloroquine can prolong the QT interval (basically, it messes with your heart’s electrical signals). For most healthy people, a few courses of the drug won’t hurt. But combine it with other meds that affect the heart—certain antibiotics or antidepressants, for example—and you could wind up in a hospital with serious arrhythmias. It’s why docs check your medication list and sometimes your EKG before starting high doses.
There are other rare but scary reactions, too, like sudden muscle weakness or severe allergic skin reactions. Here’s a checklist of who should NOT take chloroquine without specialist advice:
- People with known retinal or vision problems
- Anyone with a history of serious heart arrhythmias or family history of sudden cardiac death
- Children under age 6 (risk of overdose is high—doses for malaria are tightly weight-based)
- People with epilepsy or a history of severe psychiatric disorders; chloroquine can worsen these
- Anyone already taking medicines that prolong the QT interval
So what are some concrete safety tips for anyone prescribed chloroquine?
- Stick to the exact dose and schedule—don’t double up if you miss a pill.
- Never crush or chew, if you can avoid it. The taste is punishing for a reason.
- If you’re going to travel to a malaria area, get a checkup before and after. Malaria can hide in the liver even after symptoms clear.
- Get baseline and periodic eye exams if you’re using the drug for months at a time.
- Keep out of reach of kids—just a couple of tablets can be fatal for a small child.
Chloroquine isn’t out of the medical toolbox yet, and in the right hands, it still does good. The trick is to separate old legends and viral rumors from hard science and safe practice. If there’s one thing this medicine should teach us, it’s that every pill tells a story—and getting the details right matters more than ever.








Comments (11)
Dominic Ferraro
July 10, 2025 AT 13:31 PMChloroquine has been a staple antimalarial for decades. Its low cost makes it accessible in low‑resource settings. When parasites remain sensitive, the drug clears infection quickly. The same chemistry also dampens immune activity in lupus patients. This dual use illustrates why doctors keep it in formularies. However the safety profile demands respect. Overdose can trigger heart rhythm problems. Prolonged use may lead to retinal toxicity. Regular eye exams catch changes before vision loss occurs. Baseline ECGs identify those at risk of QT prolongation. Patients with pre‑existing heart disease should avoid high doses. Children must receive weight‑based dosing to prevent toxicity. Mixing chloroquine with other QT‑extending drugs raises danger. During the pandemic many took it without medical supervision. The lesson is clear use it under a clinician’s guidance.
Jessica Homet
July 18, 2025 AT 18:19 PMWow another re‑hash of the chloroquine circus. The media turned a decent antimalarial into a celebrity punchline and nobody bothered to fact‑check anything. You can see how cheap hype inflates risk perception while actual data stays buried. It’s frustrating how quickly the public latches onto half‑truths. Honestly, the whole saga is a textbook case of misinformation run amok.
mitch giezeman
July 26, 2025 AT 23:07 PMGreat summary! I’d add that clinicians often check retinal health before prescribing long‑term hydroxychloroquine, which is the safer cousin. For malaria‑free regions, the drug’s role is mostly limited to autoimmune therapy. It’s also worth noting that resistance monitoring is ongoing in endemic areas. If you’re considering travel, a quick consult can tailor the right prophylaxis.
Kelly Gibbs
August 4, 2025 AT 03:55 AMInteresting read, thanks.
KayLee Voir
August 12, 2025 AT 08:43 AMThanks for the thorough rundown, it really helps put the safety considerations into perspective. I appreciate the reminder about eye exams and ECG checks before starting treatment. It’s easy to overlook those steps when a drug has such a long history. Your balanced approach makes the info accessible without sounding alarmist.
Bailey Granstrom
August 20, 2025 AT 13:31 PMThe hype was a disaster, plain and simple.
Melissa Corley
August 28, 2025 AT 18:19 PMlol who even cares about some old French pill? us americans got better meds already 🙄 i think the whole chloroquine thing was just a media stunt 🤔 besides, why should we listen to foreign scientists when we have our own experts?? btw that table in the article is kinda whack tbh 😂
Kayla Rayburn
September 5, 2025 AT 23:07 PMLove how the article lays out the pros and cons without the usual sensationalism. It’s a solid read for anyone weighing treatment options. Keep up the good work, the balanced tone makes it easy to digest.
Dina Mohamed
September 14, 2025 AT 03:55 AMWow, what a comprehensive guide, and I must say, the level of detail is impressive, especially the sections on cardiac risks, retinal toxicity, and the historical context of chloroquine, which really help us understand why this drug remains relevant, and the clear recommendations for monitoring, such as baseline ECGs and regular eye exams, are incredibly valuable, keep up the great work, everyone!
Kitty Lorentz
September 22, 2025 AT 08:43 AMi felt the article was good its clear but could use more info on dosing for kids and maybe some real world examples
inas raman
September 30, 2025 AT 13:31 PMHey folks, great job on breaking down the facts! Remember, staying informed is the best defense, so keep reading and sharing reliable sources. Let’s keep the conversation going and help each other stay safe.