After a transplant, patients need to take immunosuppressive drugs for life. That’s not optional. Without them, the body attacks the new organ. But brand-name versions of these drugs can cost over $2,000 a month. For many, that’s impossible to afford. The good news? Generic versions now exist for nearly every key immunosuppressant-and they work just as well when used correctly.
What Are the Standard Immunosuppressive Combinations?
Most transplant patients take three drugs together: a calcineurin inhibitor, an antimetabolite, and a corticosteroid. This triple therapy is the gold standard. It’s not random-it’s based on decades of clinical data showing it keeps organs alive longer and reduces rejection.- Calcineurin inhibitors: Tacrolimus or cyclosporine. These block T-cells from attacking the transplant. Tacrolimus is now the most common, used in over 60% of kidney transplants.
- Antimetabolites: Mycophenolate mofetil (MMF) or mycophenolic acid (MPA). These stop immune cells from multiplying. MMF is the go-to for most new transplants.
- Corticosteroids: Prednisone. Used early after transplant to calm the immune system, but many centers now try to phase it out due to side effects like weight gain, diabetes, and bone loss.
How Much Money Do Generics Save?
The cost difference isn’t close. A month of brand-name tacrolimus (Prograf) costs $1,800-$2,200. The generic? $300-$400. That’s over 80% savings. Same with MMF: CellCept runs $1,200-$1,500 monthly. Generic MMF? $150-$250. For a patient on all three drugs, switching to generics can cut monthly costs from $4,000 to under $800. A 2023 study in Transplant International tracked 1,200 kidney transplant patients. Those on generics saved an average of $1,500 per month. Over five years? That’s over $90,000 in out-of-pocket savings. For Medicare patients, this matters even more-since Part D covers these drugs, lower costs mean less financial strain on the system.Do Generics Work as Well as Brand Names?
Yes-when monitored properly. Multiple studies confirm this. A 2022 analysis in the American Journal of Transplantation looked at over 8,000 kidney transplant patients. One-year graft survival was 95.1% for brand-name tacrolimus and 94.7% for the generic. The difference? Statistically meaningless. The FDA requires generics to be bioequivalent: they must deliver the same amount of drug into the bloodstream as the brand, within a range of 80% to 125%. For most drugs, that’s fine. But for immunosuppressants, that range is wide. Tacrolimus has a narrow therapeutic window. Too little? Rejection. Too much? Kidney damage or infection. That’s why switching isn’t just a pharmacy change-it’s a medical process. Blood levels must be checked more often during the first 3-6 months. Some patients need dose tweaks. A 2021 survey of 127 transplant centers found 18% saw a temporary spike in rejection episodes after switching to generics. But those cases dropped sharply once TDM (therapeutic drug monitoring) protocols were tightened.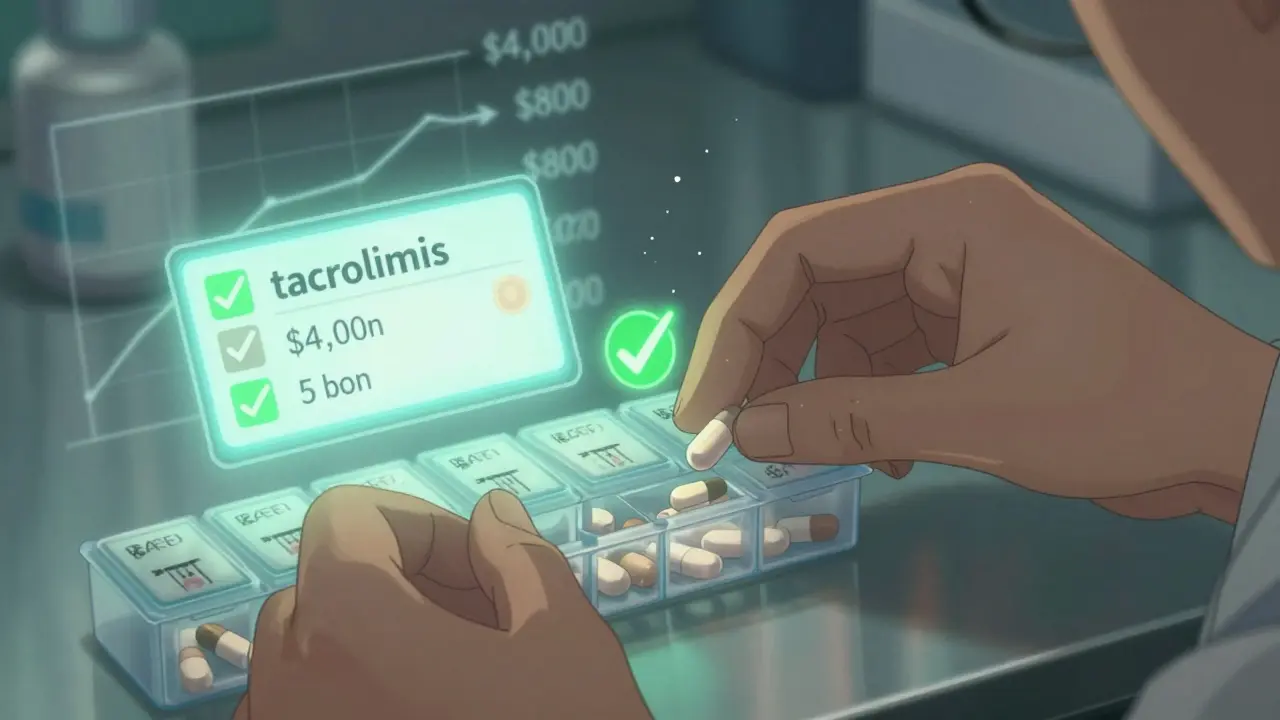
Which Generic Combinations Are Most Common?
The most popular combo? Generic tacrolimus + generic MMF. It’s used in 64% of new kidney transplants. Why? Proven safety, predictable results, and low cost. But there are other options gaining traction:- Tacrolimus + Sirolimus: This combo avoids steroids and MMF. It’s especially useful for patients with high rejection risk or those who develop cancer after transplant. A 2019 study from the University of Maryland found lung transplant patients on this combo lived nearly two years longer on average than those on tacrolimus + MMF.
- Corticosteroid-Sparing Regimens: Using tacrolimus + sirolimus without prednisone cuts post-transplant diabetes risk by 31%, according to a 2024 review in Transplantation Reviews. That’s huge-diabetes is one of the most common long-term complications.
- MPA instead of MMF: Mycophenolic acid is the acid form of MMF. It’s absorbed differently and sometimes preferred for patients with GI issues. Generic MPA became available in 2020.
What Are the Real-World Problems?
Despite the savings, switching isn’t always smooth. Here’s what patients and providers actually deal with:- Bioavailability differences: Generic manufacturers use different fillers and coatings. One batch of generic tacrolimus might absorb slightly differently than another-even if both are FDA-approved. That’s why most transplant centers insist on sticking with one generic brand. Switching between generic makers can cause blood levels to swing.
- Drug interactions: Immunosuppressants play well with almost nothing. Antibiotics, antifungals, even grapefruit juice can change how they work. A 2023 study found 67% of patients on multiple generics had at least one dangerous interaction. Pharmacists now review every new medication.
- Monitoring burden: After switching, patients often need blood tests every two weeks for the first two months, then monthly. That means more clinic visits, more lab fees, more stress. One pharmacist told the Journal of Pharmacy Practice they saw 30% more visits in the first six months after switching patients to generics.
- Patient anxiety: Many patients fear generics are “inferior.” Reddit threads and patient forums are full of stories. One user, ‘TransplantSurvivor89,’ reported three rejection episodes after switching to generic tacrolimus. Another, ‘KidneyWarrior2020,’ said they’ve been on generic MMF for three years with zero issues. Both are real. The difference? Monitoring.
How Do You Switch Safely?
There’s no rush. The process takes time-and structure.- Start with new transplants: Most centers now begin all new patients on generics. It’s easier than switching someone stable.
- Use one generic manufacturer: Don’t let the pharmacy switch brands. Ask for the same generic every time.
- Check blood levels before and after: Get a baseline level on the brand drug. Then test again 7-10 days after switching. Adjust dose if needed.
- Monitor for 3-6 months: Weekly or biweekly checks at first. Then monthly. Track symptoms: fever, fatigue, swelling, or dark urine could signal rejection or toxicity.
- Involve the pharmacist: Transplant pharmacists are trained in these drugs. They know interactions, dosing quirks, and which generics work best.

What’s Changing in 2025?
The field is moving fast. Here’s what’s new:- Interchangeable biosimilars: In May 2023, the FDA approved the first interchangeable biosimilar for belatacept (Nulojix). This could cut costs by 40% for patients on advanced regimens.
- KDIGO guidelines update: The 2024 guidelines now recommend generic sirolimus as a first-line option for high-risk kidney transplant patients.
- Withdrawal protocols: Early trials are testing whether some patients can stop all immunosuppressants after a few years using a special induction drug (alemtuzumab) followed by generic tacrolimus and sirolimus. It’s still experimental-but promising.
- Manufacturing quality: The FDA found 12% of generic tacrolimus batches failed dissolution testing in 2022. That’s why centers are pushing for tighter oversight and single-source sourcing.
Who Should Avoid Generics?
Not everyone. Patients with:- History of rejection after switching
- Unstable blood levels despite monitoring
- Severe GI issues affecting absorption
- Complex drug interactions (e.g., multiple antifungals or antivirals)
Final Thoughts
Generic immunosuppressants aren’t a compromise. They’re a breakthrough. They’ve made lifelong transplant care affordable for thousands who couldn’t otherwise afford it. The data shows they work. The savings are undeniable. But they’re not plug-and-play. Success depends on careful monitoring, consistent sourcing, and educated patients. The goal isn’t just to save money. It’s to save lives. And generics, when used right, do both.Are generic immunosuppressants as effective as brand names?
Yes, when used with proper therapeutic drug monitoring. Large studies show no significant difference in graft survival between brand and generic tacrolimus, MMF, or sirolimus. The FDA requires generics to be bioequivalent, and real-world data from transplant centers confirms equivalent outcomes-when dosing is carefully managed.
Why do some patients have rejection after switching to generics?
Rejection after switching is rare but can happen due to small differences in how the body absorbs the drug. Generic versions may have slightly different fillers or coatings, which can affect absorption speed. Without close blood level monitoring, these differences can lead to under-dosing. Most rejection episodes occur in the first 90 days and are preventable with biweekly blood tests and dose adjustments.
Can I switch between different generic brands?
It’s not recommended. Even though all generics meet FDA standards, each manufacturer uses different inactive ingredients. Switching brands can cause your drug levels to fluctuate, increasing the risk of rejection or toxicity. Most transplant centers require patients to stay on the same generic manufacturer for consistency.
What’s the difference between MMF and MPA?
Mycophenolate mofetil (MMF) is a prodrug that converts to mycophenolic acid (MPA) in the body. MPA is the active form. Generic MMF and MPA are both available. MPA is sometimes preferred for patients with stomach issues, as it’s absorbed differently and may cause less nausea. Both are equally effective when dosed correctly.
Do generics increase the risk of side effects?
The side effects-like tremors, high blood pressure, or diarrhea-are the same as with brand names because they’re caused by the same active drug. However, if blood levels fluctuate due to poor absorption or switching brands, side effects can become more frequent or severe. Consistent dosing and monitoring reduce this risk.
How often should I get blood tests after switching to generics?
In the first 30 days after switching, blood tests should be done every 7-14 days. After that, monthly checks are usually sufficient if levels are stable. Your doctor will adjust this based on your history, the specific drugs you’re taking, and whether you’ve had any recent changes in other medications.
Are there financial assistance programs for generic immunosuppressants?
Yes. While brand-name manufacturers used to offer the best patient support, 65% of generic manufacturers now provide copay assistance programs. Companies like Teva, Sandoz, and Mylan offer cards that can reduce monthly costs to under $10 for eligible patients. Always ask your pharmacist or transplant coordinator about available programs.





Comments (11)
Nicole Beasley
December 28, 2025 AT 11:29 AMOMG I switched to generic tacrolimus last year and my kidney’s still kicking 😭💸 Like, I was terrified but my docs said it’s fine and now I’m saving $1,500/month?? I’m literally crying happy tears. Also, my pharmacist gave me a free coupon for $5 a month?? 🤯
sonam gupta
December 28, 2025 AT 12:52 PMIndia makes 70 of the worlds generics and you still worry about quality USA thinks money is medicine
Julius Hader
December 29, 2025 AT 16:40 PMLook I get the savings but if your life depends on this drug why gamble with some factory in Bangladesh that probably uses the same packaging as your phone charger? I know people who lost grafts because they switched. Its not worth it. I'd rather pay the extra $1,800 than bury my kid.
Vu L
December 30, 2025 AT 15:52 PMYeah sure the studies say they work the same but have you seen the FDA batch failure rates? 12% of generic tacrolimus doesn't even dissolve properly. That's not a drug thats a potato with a label. Also why is no one talking about how the pharmacy swaps brands without telling you? I found out mine changed because my tremors got worse. They didn't even warn me.
James Hilton
January 1, 2026 AT 07:50 AMGenerics are the only reason I'm still alive. The US healthcare system is a joke but at least someone made the smart move and let us buy the same damn drug for 1/5 the price. Meanwhile rich folks are still crying about their $2,000 Prograf bottles like it's a luxury watch. 🤡
Mimi Bos
January 2, 2026 AT 00:09 AMi just switched to generic mmf and my stomach feels better but i keep forgetting to take my blood test and now i think i might be getting sick?? help??
Payton Daily
January 2, 2026 AT 02:52 AMThink about it. The body is a temple. The soul knows the difference between a brand and a knockoff. You think God cares if your kidney lasts 5 years or 15? No. But He sees the arrogance of trying to cut corners on life itself. These generics are like feeding your child store-brand baby food because you're too cheap to buy the organic stuff. It's not science. It's spiritual neglect.
And don't tell me about bioequivalence. That's just corporate jargon for 'we hope it works'. The body isn't a math problem. It's a miracle. And miracles don't come with a barcode.
I know a man who died because he trusted the FDA. His last words were 'I just wanted to save money'. That's not a tragedy. That's a sin.
oluwarotimi w alaka
January 3, 2026 AT 13:38 PMUSA always blame generics but who really controls the pharma? Big pharma from USA and europe they let generics in only when they own the company. You think teva or sandoz are independent? They are subsidiaries. They want you to think its cheaper but its still the same system. And why do you think the FDA approved so many bad batches? To keep you dependent on the system. Wake up.
Samantha Hobbs
January 3, 2026 AT 15:42 PMHey I just had a transplant last month and I’m on generics - but I’m scared to switch pharmacies because my cousin’s friend’s neighbor had a rejection after changing brands. Should I just ask my doctor to lock me into one specific generic? Like, can I even do that??
Kelsey Youmans
January 5, 2026 AT 00:11 AMThank you for presenting this information with such clarity and rigor. The data supporting the efficacy of generic immunosuppressants, when paired with rigorous therapeutic drug monitoring, is both compelling and reassuring. It is imperative that patients are not only informed of their options but also empowered to engage in shared decision-making with their clinical teams. The financial relief afforded by generics is not merely economic-it is profoundly human.
Sydney Lee
January 5, 2026 AT 12:30 PMLet’s be honest: the only reason generics are even being discussed is because the American healthcare system has collapsed into a grotesque parody of itself. We are now reduced to debating whether a $300 pill can save a life, while CEOs cash in on $2,000 brand-name bottles. This isn’t medicine. It’s a moral bankruptcy dressed in lab coats. And yet somehow, we’re supposed to be grateful that the system lets us live at all? How pathetic.