Most people don’t think about where they keep their pills until they find a bottle of antibiotics that smells weird or a bottle of insulin that looks cloudy. But storing medications wrong doesn’t just mean wasting money-it can make your medicine less effective or even dangerous. The medication storage habits you use at home are the biggest reason why so many drugs expire before they should.
Why Your Medicine Expires Sooner Than It Should
Expiration dates aren’t random. They’re based on strict testing by drugmakers to prove the medicine will stay at 90-110% of its labeled strength until that date-if stored correctly. The U.S. Food and Drug Administration (FDA) requires this testing, and the data shows that most medicines last longer than the printed date-if they’re kept in the right environment.
But in real life, most homes are terrible for storing meds. The bathroom? Hot and steamy. The kitchen? Near the stove, where temperatures jump up and down. The drawer under the sink? Damp and dark. These places destroy pills and liquids faster than you think.
According to the CDC, 37% of premature medicine expiration happens because of poor storage. And humidity is the #1 killer-68% of cases involve moisture damage. Aspirin breaks down into vinegar-like acids. Liquid antibiotics grow bacteria. Insulin clumps. Eye drops become contaminated. All of it happens because of heat, light, and dampness.
Where NOT to Store Your Medications
Let’s be clear: your bathroom cabinet is the worst place for meds. During a hot shower, humidity spikes to 85-95%. A 2023 UCHealth study showed that aspirin stored in a bathroom cabinet degrades 300% faster than in a dry room. That means your painkiller might be half as strong by the time you need it.
The kitchen is almost as bad. If your meds sit near the stove, oven, or microwave, they’re exposed to temperature swings of more than 15°C in under 30 minutes. Swedish Medical Center’s 2022 research found that 42% of common antibiotics lost potency within 90 days under these conditions.
Even your bedroom dresser isn’t safe if it’s near a window that gets direct sun. UV light breaks down medications too. Amber prescription bottles block 97% of UV rays. Clear plastic bottles? Not so much.
And don’t leave pills in your car. Summer temperatures inside a parked car can hit 60°C. That’s enough to melt capsules, warp tablets, and ruin liquid medicines in hours.
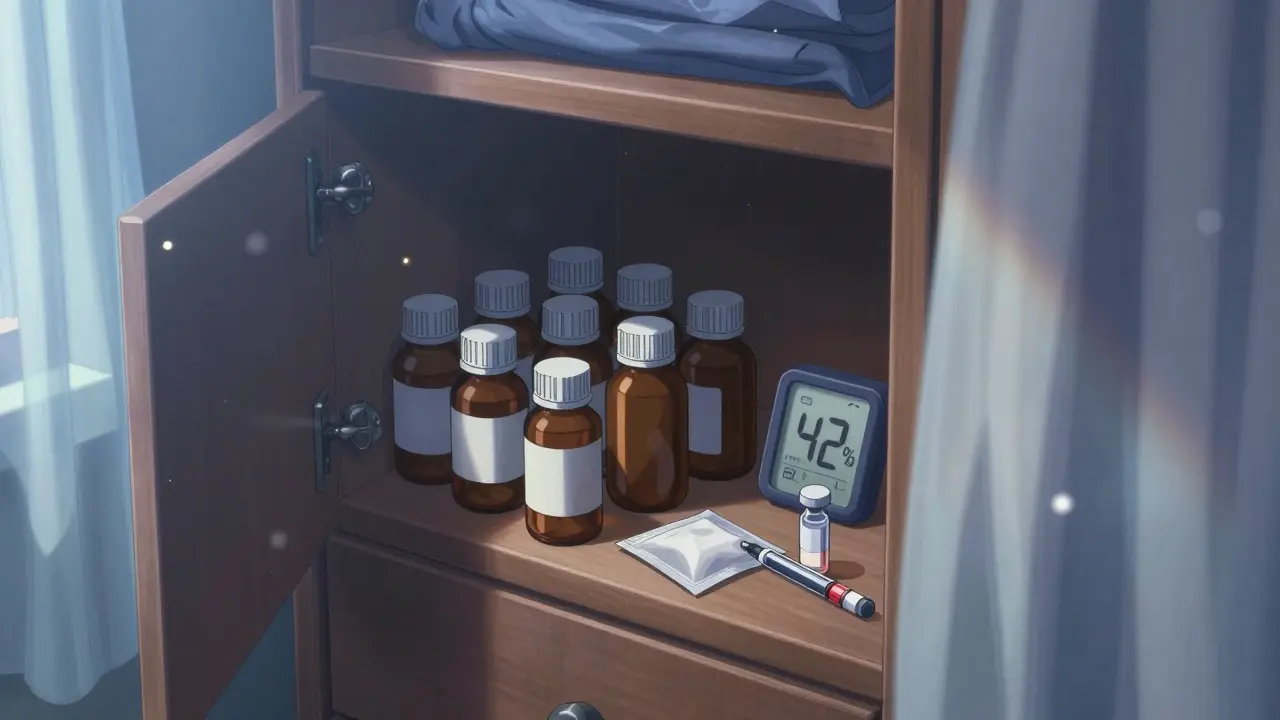
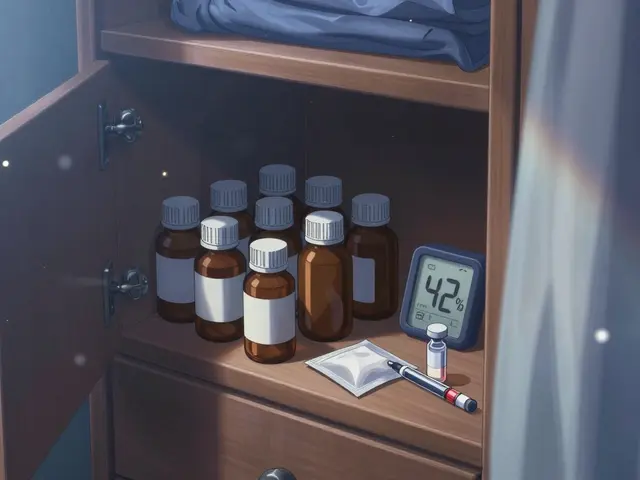
Where You SHOULD Store Your Medications
The best spot is a cool, dry, dark place-away from heat, moisture, and light. A locked cabinet in a bedroom closet, a drawer in a bedroom dresser, or a shelf in a hallway cabinet all work well. The ideal temperature is 20-25°C (68-77°F), with humidity below 60%.
Use a simple hygrometer (a $10 device that measures humidity) to check your storage spot. If it’s above 60%, move your meds. If it’s below 45%, you’re golden.
Keep everything in its original container. Those bottles aren’t just for looks-they’re designed to protect. Amber glass blocks UV light. Child-resistant caps keep kids out. Labels show storage instructions, lot numbers, and expiration dates. Taking pills out of their bottles and tossing them into a pill organizer? Fine for daily use-but only if you refill it weekly and keep the original bottle safely stored.

Special Cases: Insulin, Nitroglycerin, Eye Drops, and More
Some medicines have strict rules that can’t be ignored.
Insulin: Unopened insulin must stay refrigerated between 2-8°C. Once opened, it can sit at room temperature (up to 25°C) for up to 28 days. But never leave it in the fridge door-temperature changes there can ruin it. Store it in the middle shelf.
Nitroglycerin: These tablets are super sensitive to light and heat. Keep them in the original dark glass bottle, tightly closed, and away from windows. Replace the bottle every 3-6 months, even if it’s not empty-potency drops fast.
Eye drops: Once opened, most last only 28 days. After that, they can grow dangerous bacteria like Pseudomonas aeruginosa. The American Society of Health-System Pharmacists says 78% of expired eye drops are contaminated. Write the open date on the bottle with a marker.
Liquid antibiotics: Some need refrigeration. Always check the label. If it says “keep refrigerated,” don’t leave it on the counter. If it says “discard after 14 days,” throw it out-even if it looks fine.
How to Track Expiration Dates (Without Forgetting)
People forget. That’s normal. But forgetting leads to taking expired meds-or worse, throwing away perfectly good ones.
One simple fix: assign one person in the household to check meds every month. Just open the cabinet, look at each bottle, and note the expiration date. Use a permanent marker to write the date on a sticky note and stick it to the front of the bottle.
Or use a color-coding system. Red dots = expires this year. Blue dots = next year. Green dots = two years out. The University of Wisconsin’s Research Animal Resources Center used this method and cut expired meds by 63% in their facility.
Smart pillboxes like MedMinder Pro can help too. They monitor temperature and humidity and send alerts if conditions go out of range. They’re not cheap, but for someone on multiple daily meds, they’re worth it.
Signs Your Medicine Has Gone Bad
You don’t need a lab to tell if your medicine is still good. Look for these red flags:
- Tablets or capsules that are cracked, discolored, or sticky
- Pills that smell like vinegar (aspirin breaking down)
- Liquid meds with particles, cloudiness, or sediment
- Eye drops that change color or smell odd
- Insulin that looks cloudy or has clumps when it should be clear
If you see any of these, don’t risk it. Even if the expiration date hasn’t passed, the medicine may no longer be safe or effective.

What to Do With Old or Expired Medications
Never flush pills down the toilet or toss them in the trash. The CDC says 55% of households do this, and it pollutes water and puts meds in the hands of kids or pets.
Instead, use a drug take-back program. The DEA runs National Prescription Drug Take Back Day twice a year. The next one is October 26, 2024. There are over 11,000 collection sites across the U.S.-pharmacies, police stations, hospitals. Find yours at deas.gov/takebackday.
If you can’t wait, mix pills with coffee grounds or cat litter, seal them in a plastic bag, and throw them in the trash. This makes them unappealing and unusable.
What’s Changing in Medication Storage
The industry is catching on. Merck’s new heat-stable insulin, approved in December 2023, can last 56 days at 30°C-huge for people without reliable refrigeration. New prescription labels now include simple icons showing storage needs: a snowflake for refrigeration, a sun with a line through it for light-sensitive meds.
Pharmacies are starting to hand out silica-gel packs inside pill bottles. These tiny packets absorb moisture and keep humidity low. Trials at the University of Wisconsin show they cut humidity inside bottles by 45%.
And the World Health Organization says better storage education could save $14.3 billion globally by 2030. Right now, rural households are hit hardest-41% faster degradation because they lack climate-controlled spaces. But awareness is growing.
Final Tip: Keep It Simple
You don’t need a lab to store meds safely. Just remember this:
- Keep them cool and dry-not hot or damp
- Leave them in their original bottles
- Check expiration dates monthly
- Throw out anything that looks or smells weird
- Use take-back programs, don’t flush or trash them
Proper storage doesn’t take much time-but it saves money, keeps you safe, and ensures your medicine works when you need it most.
Can I still use medicine after its expiration date?
The expiration date is the last day the manufacturer guarantees full strength and safety. While some studies (like the FDA’s Shelf Life Extension Program) show certain medications remain effective years past expiration when stored perfectly, this doesn’t apply to typical home conditions. Heat, humidity, and light degrade drugs fast. Don’t risk it-especially with antibiotics, insulin, or heart meds. If it’s expired, replace it.
Is it safe to store pills in a pill organizer?
Yes-but only if you refill it weekly and keep the original bottle in a cool, dry place. Pill organizers expose meds to air and light, which can break them down. Also, some pills (like nitroglycerin) lose potency quickly once removed from their original container. Use organizers for convenience, not long-term storage.
Do I need to refrigerate all liquid medications?
No. Only refrigerate liquids if the label says so. Common ones that need refrigeration include some antibiotics, insulin, and eye drops. Others, like cough syrup, are fine at room temperature. Always check the label or ask your pharmacist. If you’re unsure, keep it cool-it won’t hurt.
What happens if I take expired medicine?
Taking expired medicine usually won’t poison you-but it might not work. Antibiotics can fail, leading to worse infections. Painkillers may not relieve pain. Epinephrine auto-injectors (like EpiPens) can lose potency, putting someone at risk during an allergic reaction. The danger isn’t usually toxicity-it’s ineffectiveness.
How can I tell if my medicine is still good if the label is faded?
Call your pharmacy. They can look up your prescription history and tell you the original expiration date. If you can’t reach them, check for physical signs: discoloration, odd smells, clumping, or particles. If anything looks off, throw it out. It’s not worth the risk.








Comments (10)
Amber Lane
January 20, 2026 AT 02:33 AMI used to keep my pills in the bathroom until my mom caught me and made me move them. Now I have a little bin in my bedroom drawer. No more weird smells or sticky aspirin.
Roisin Kelly
January 20, 2026 AT 14:49 PMOf course the government says it’s fine to store meds anywhere. They don’t care if you die from weak antibiotics. Big Pharma wants you to keep buying new bottles. That’s why they don’t tell you about the real storage rules.
Coral Bosley
January 20, 2026 AT 15:15 PMHumidity is the silent killer of medicine. I used to think it was just a myth until my insulin turned into a gelatinous mess after leaving it in the kitchen for a week. Now I keep it in a sealed Tupperware with silica packs. It’s not glamorous, but it works.
And don’t even get me started on those damn pill organizers. They look cute on Instagram but they’re basically little death traps for your meds. Light, air, time-they’re all conspiring against you.
I’ve started labeling every bottle with the date I opened it. Even my cat knows not to knock over the amber bottles anymore.
Also, if your eye drops smell like regret, throw them out. No exceptions.
Kevin Narvaes
January 21, 2026 AT 12:58 PMpeople think expiration dates are like a warranty but theyre not. its more like a ‘dont blame us if this stops working’ notice. i had a 5 year old epipen that still worked fine but i threw it out anyway because the label said so. dumb.
also why do pharmacies still use clear plastic bottles? its like they want your meds to die.
Jerry Rodrigues
January 22, 2026 AT 01:28 AMSimple advice: cool, dry, dark. That’s it. No need to overthink it. I use a shoebox in my closet. Works fine.
Uju Megafu
January 23, 2026 AT 06:01 AMOf course you’re telling people to store meds in their bedrooms. But what about people who live in apartments with no closet? Or in places where the AC breaks for weeks? You’re not addressing the real issue-poverty. The system is designed to make poor people waste money on medicine they can’t afford to replace.
And don’t even get me started on how pharmacies charge $100 for a bottle of insulin while the cost to produce it is $3. This isn’t about storage. This is about greed.
Jarrod Flesch
January 24, 2026 AT 19:45 PMJust added silica gel packs to my pill bottles after reading this. Total game changer. Also, I put a little humidity reader next to my meds-keeps me honest. 🌡️
And yes, the bathroom is a no-go zone. I used to keep my nitro there because it was convenient. Now I keep it in a ziplock with a silica pack in my nightstand. No more panic attacks from expired meds.
Barbara Mahone
January 26, 2026 AT 12:01 PMThe CDC data on humidity-related degradation is well-documented and consistently replicated. Storing medications in environments exceeding 60% relative humidity significantly accelerates hydrolytic degradation of ester-containing compounds such as aspirin and nitroglycerin. Original packaging is not incidental-it is engineered for stability.
For those using pill organizers, weekly refills are optimal. Prolonged exposure to ambient air and light compromises the integrity of many formulations, especially those with photosensitive active ingredients.
Kelly McRainey Moore
January 27, 2026 AT 10:10 AMI started writing the open date on my eye drops with a Sharpie and it changed everything. No more guessing. Also, my partner and I do a monthly check together-makes it feel less like a chore and more like taking care of each other.
Stephen Rock
January 28, 2026 AT 13:09 PMWow. So much effort for something that should be free. Why don’t drug companies make heat-stable meds the standard instead of forcing us to become amateur pharmacists? This whole system is designed to keep you anxious and buying more