Not all beta-blockers are the same - and choosing the wrong one can make a real difference
If you’ve been prescribed a beta-blocker, you might assume they’re all pretty much alike. After all, they all slow your heart rate, lower blood pressure, and help with chest pain or irregular heartbeats. But here’s the truth: beta-blockers aren’t interchangeable. The difference between propranolol and carvedilol isn’t just the brand name - it’s how your body reacts, what side effects you get, and even whether you can safely use them if you have asthma or diabetes.
These drugs block adrenaline’s effects on your heart and blood vessels, but each one does it in a slightly different way. Some hit only the heart. Others also widen your blood vessels. Some cause fatigue and cold hands. Others might actually help with sexual function. Knowing which one you’re on - and why - can change your quality of life.
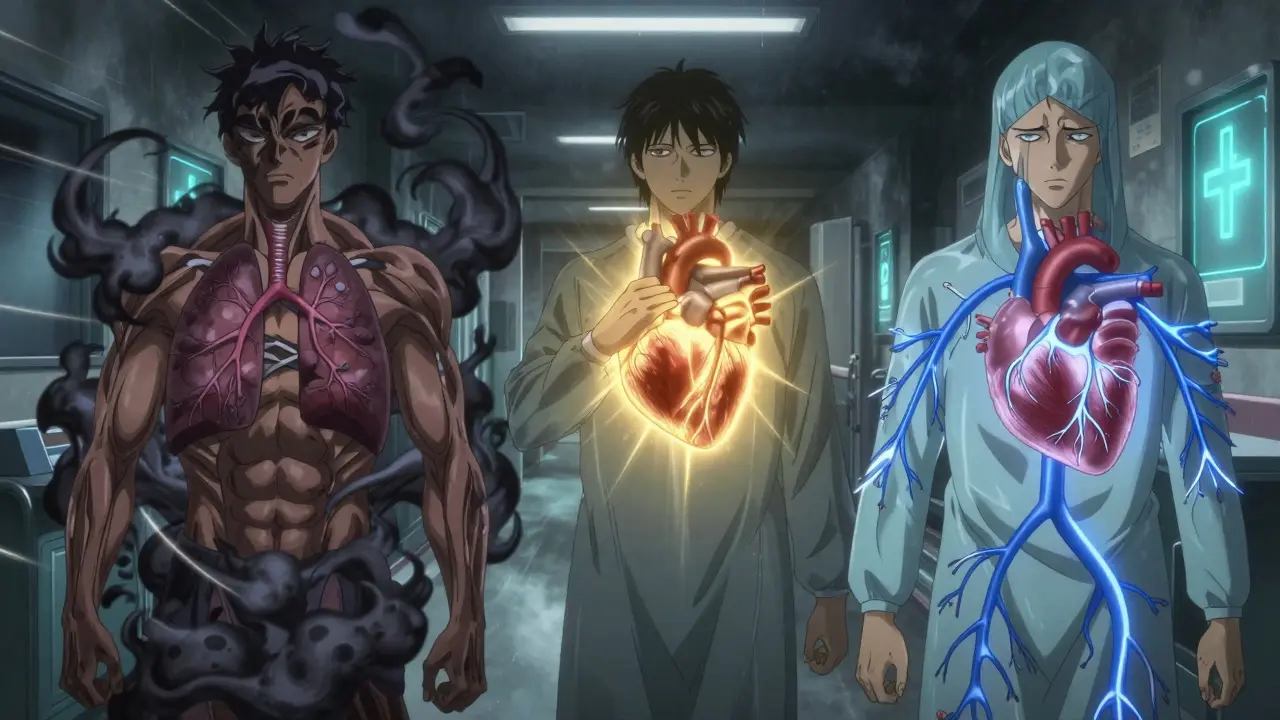
First-generation beta-blockers: The original, but not always the best
Propranolol was the first beta-blocker ever developed, back in the 1960s. It’s still used today - mostly for migraines, tremors, and anxiety - because it blocks both beta-1 and beta-2 receptors. That means it affects your heart, lungs, blood vessels, and even your liver. Sounds powerful, right? But that’s also why it’s risky for people with asthma or COPD. Blocking beta-2 receptors in the airways can cause bronchospasm, making breathing harder. Studies show up to 30% of asthmatic patients on propranolol experience worsening symptoms.
It’s also notorious for side effects. Patient reviews on Drugs.com show 38% report moderate to severe side effects: sleep problems, depression, and trouble exercising. One user in Manchester wrote, “I couldn’t walk up the stairs without gasping - it felt like my body had been turned off.” That’s not just in their head. Propranolol reduces energy production in muscle cells by blocking the adrenaline-driven release of glucose and fatty acids. For someone active, that’s a dealbreaker.
Second-generation: Heart-focused, fewer side effects
Then came the smarter versions: atenolol, metoprolol, bisoprolol. These are called cardioselective - they mostly target beta-1 receptors in the heart. That means less impact on your lungs, less risk for asthma flare-ups, and fewer metabolic side effects. For people with diabetes, that’s huge. Beta-2 blockade can mask low blood sugar symptoms like shakiness and rapid heartbeat. Cardioselective blockers don’t do that as much.
Metoprolol comes in two forms: the regular kind (tartrate) that you take twice a day, and the extended-release version (succinate) that you take once. The once-daily version is easier to stick with - and studies show better adherence. A Cleveland Clinic survey found 85% of heart failure patients stuck with metoprolol succinate compared to only 62% on the twice-daily version.
Bisoprolol is another standout. It’s the most selective of the group, with the lowest chance of causing fatigue or cold hands. Patient ratings on Drugs.com give it a 7.1 out of 10 - higher than propranolol’s 6.2. That’s not just luck. In a 2021 UK primary care study, patients switched from propranolol to bisoprolol reported 40% fewer side effects and better exercise tolerance within six weeks.
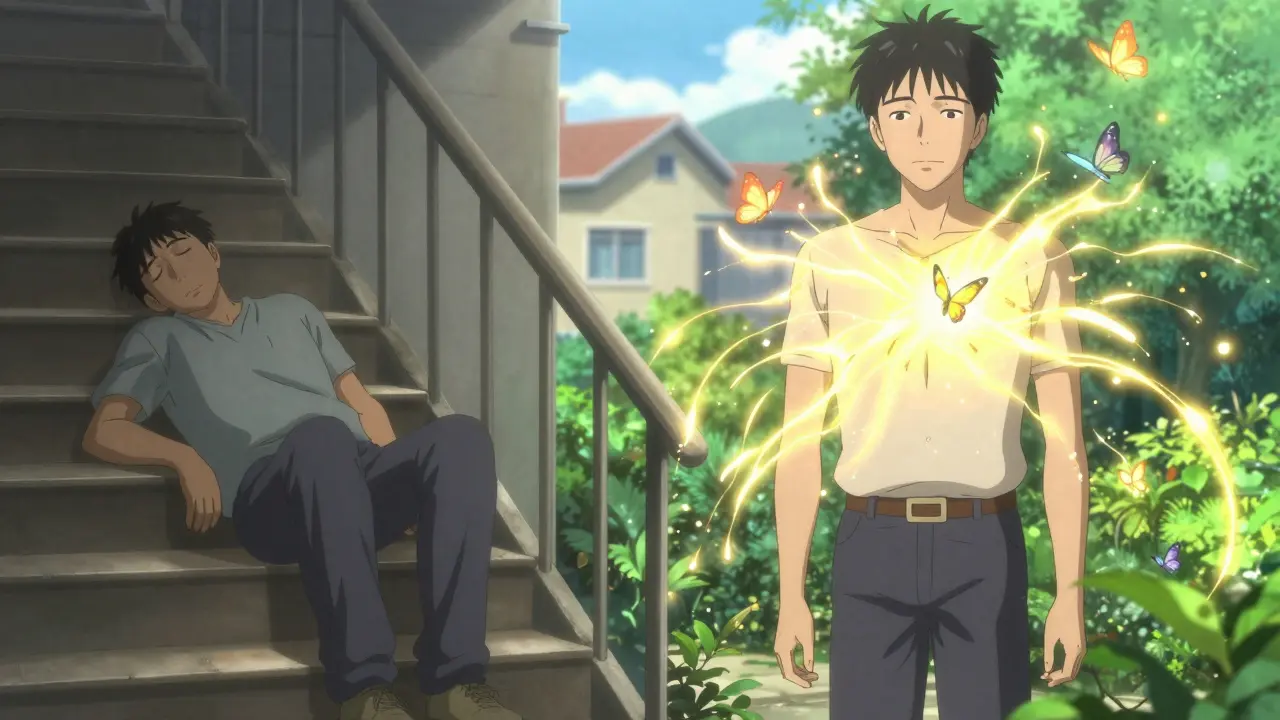
Third-generation: More than just blocking - they’re repairing
Carvedilol and nebivolol aren’t just beta-blockers. They’re heart healers.
Carvedilol blocks beta receptors AND alpha-1 receptors. That means it doesn’t just slow your heart - it relaxes your blood vessels, lowering blood pressure even more. In the landmark US Carvedilol Heart Failure Study (1996), it cut death risk by 35% compared to placebo. That’s why it’s now a first-choice drug for heart failure with reduced ejection fraction. It also has powerful antioxidant effects. Lab studies show it reduces oxidative stress in heart tissue by 30-40%, helping prevent the scarring and stiffening that leads to heart failure progression.
Nebivolol is even more unique. It doesn’t just block beta-1 receptors - it activates beta-3 receptors, which trigger your body to release nitric oxide. That’s the same molecule that makes Viagra work. And guess what? In men over 50, 65% reported improved sexual function on nebivolol, compared to only 35% on older beta-blockers. It also reduces arterial stiffness, which helps lower central blood pressure - something most beta-blockers fail to do.
And unlike carvedilol, nebivolol doesn’t cause weight gain or worsen insulin resistance. That’s why it’s often preferred for older patients or those with metabolic syndrome.
Why your doctor picks one over another
It’s not random. Doctors use a mental checklist when choosing a beta-blocker:
- Asthma or COPD? Avoid propranolol. Use bisoprolol or nebivolol instead.
- Heart failure? Carvedilol or nebivolol - they’re proven to save lives.
- High blood pressure alone? These days, ACE inhibitors or calcium channel blockers are better first choices. Beta-blockers are now mostly for people who also have heart disease.
- Diabetes? Stick with cardioselective agents like bisoprolol or nebivolol to avoid hiding low blood sugar signs.
- Depression or fatigue? Propranolol is a known culprit. Switching to nebivolol or bisoprolol often lifts mood and energy.
- Erectile dysfunction? Nebivolol may help. Metoprolol or carvedilol might make it worse.
Guidelines from the European Society of Cardiology and the American College of Cardiology now specifically recommend carvedilol, bisoprolol, and nebivolol for heart failure. Metoprolol succinate is included too - but not metoprolol tartrate. That’s because the extended-release form gives steadier blood levels, which matters for survival.
The hidden dangers: Stopping abruptly
One of the most dangerous mistakes patients make is stopping beta-blockers cold turkey. If you’ve been on them for months - especially after a heart attack - your heart gets used to the lack of adrenaline. Suddenly removing the drug causes a rebound surge of adrenaline. Your heart rate spikes. Blood pressure rockets. The risk of heart attack in the first 48 hours jumps by 300%, according to the FDA.
That’s why doctors always taper the dose slowly. For carvedilol, it can take 8-12 weeks to safely stop. Never do it on your own. If you feel side effects, talk to your doctor. There’s almost always a better option.

What’s new in 2026
The beta-blocker world is evolving. In 2023, the FDA approved entricarone - a new drug that combines beta-1 blockade with beta-3 activation - for heart failure with preserved ejection fraction. Early results show a 22% drop in hospitalizations. By 2024, a combo pill of nebivolol and valsartan (an ARB) will hit the market, simplifying treatment for patients with both high blood pressure and heart failure.
Even more exciting: the GENETIC-BB trial is testing whether your DNA can predict which beta-blocker you’ll respond to best. Early data suggests people with certain gene variants metabolize metoprolol faster - meaning they need higher doses. Others are more sensitive to carvedilol’s effects. Personalized dosing could be the next big thing.
Real talk: What patients actually experience
On Reddit’s r/Cardiology, a nurse wrote: “I had a 72-year-old man on propranolol for migraines. He couldn’t walk to the mailbox without getting winded. We switched him to bisoprolol. Two weeks later, he came in gardening. Said he felt like he got his life back.”
Another patient in Manchester shared: “I was on metoprolol for years. Felt like a zombie. Switched to nebivolol - energy came back, my blood pressure dropped more, and I didn’t need Viagra anymore. My wife thanked me.”
These aren’t outliers. They’re the rule. Beta-blockers aren’t one-size-fits-all. The right one can mean the difference between feeling okay and feeling like yourself again.
Bottom line: Ask the right questions
If you’re on a beta-blocker, ask your doctor:
- Which type am I taking - and why?
- Is this the best choice for my other conditions - like asthma, diabetes, or depression?
- Are there alternatives with fewer side effects?
- Could switching help me feel better?
Don’t just accept the first prescription. Your heart deserves a tailored fit - not a generic one.








Comments (15)
franklin hillary
February 2, 2026 AT 10:07 AMLet me tell you something real quick - beta-blockers aren't just pills, they're life-altering tools. Propranolol? That's the old-school sledgehammer. Carvedilol? That's the precision scalpel. And nebivolol? That's the guy who not only fixes your heart but also gives you back your sex life. I've seen patients go from barely walking to hiking mountains after a switch. It's not magic. It's pharmacology. Stop treating them like interchangeable cookies and start treating them like customized medicine. Your heart isn't a one-size-fits-all machine.
Naomi Walsh
February 3, 2026 AT 05:49 AMHonestly, I'm shocked anyone still prescribes propranolol for anything other than migraines. The side effect profile is so outdated it's almost unethical. I reviewed the 2021 UK primary care study last week - bisoprolol outperformed it in every metric except cost. And cost shouldn't be the deciding factor when you're trading quality of life for pennies. The fact that some GPs still default to it is a scandal.
June Richards
February 5, 2026 AT 01:31 AMI'm just here to say I've been on metoprolol for 7 years and I feel like a robot. Also I hate my life now. 🤡
Lu Gao
February 6, 2026 AT 11:59 AMWait wait wait - you said nebivolol improves sexual function? 😳 I thought ALL beta-blockers ruined that. So… it’s like Viagra but for your heart? That’s wild. I need to tell my dad. He’s on carvedilol and he’s been grumpy since 2020. Maybe he just needs a switch. 💉
Jamie Allan Brown
February 6, 2026 AT 16:58 PMI appreciate how thorough this is. But I want to gently remind folks that not everyone has access to the newest meds. Bisoprolol and nebivolol are fantastic - but they’re expensive. In rural America, or for folks on Medicaid, propranolol might still be the only option. The goal isn’t to shame doctors who prescribe it - it’s to advocate for better access to the best options. Let’s push for policy change, not just pill swaps.
Lisa Rodriguez
February 8, 2026 AT 16:11 PMMy cardiologist switched me from metoprolol tartrate to succinate last year and I didn't even realize how much I was struggling until I stopped feeling like a zombie. I started cooking again. I walked to the store. I slept through the night. It wasn't a miracle. It was just the right formulation. People need to know this stuff isn't random. It's science. And your doctor should be able to explain why they picked one over another.
Nicki Aries
February 9, 2026 AT 10:27 AMI'm not a doctor, but I read a lot of medical journals, and I'm pretty sure you're all missing the point. Beta-blockers don't fix anything - they just mask symptoms. The real issue is inflammation, oxidative stress, endothelial dysfunction - all of which are caused by processed foods, stress, and lack of sleep. You're all just chasing pills while the root cause is sitting in your fridge and your inbox. I'm not saying meds are bad - I'm saying they're a Band-Aid on a bullet wound.
Ed Di Cristofaro
February 10, 2026 AT 23:57 PMI saw a guy on TikTok say nebivolol gives you boners. That's why my doc switched me. He didn't even ask me if I cared. I just got a new script and now I'm horny and not dead. Thank you science.
Lilliana Lowe
February 12, 2026 AT 12:29 PMThe assertion that nebivolol activates beta-3 receptors to induce nitric oxide release is not entirely accurate. While it does have NO-mediated vasodilatory effects, the mechanism is more nuanced and involves eNOS upregulation rather than direct beta-3 agonism. Furthermore, the claim that 65% of men experience improved sexual function lacks a properly cited, peer-reviewed source. This post reads like a pharmaceutical marketing brochure masquerading as clinical advice.
Deep Rank
February 13, 2026 AT 03:22 AMI know this is going to sound crazy but I think beta blockers are part of a bigger plot. Like, why do they make you so tired? Why do they make people depressed? I think Big Pharma wants us to be docile. I mean, think about it - if you're tired and sad, you're not going to question your job, your government, your life. And then you get addicted to the pill. And then you can't live without it. I went off propranolol cold turkey and I felt like a new person. Like I remembered who I was. I think they want us to be zombies. I think they're scared of us being awake. I think this is all about control. I think the doctors know. I think the nurses know. I think you all are just too scared to say it out loud. I'm not taking it anymore. I'm going to eat turmeric and meditate and scream into the void. And I'm going to be free.
Bob Cohen
February 14, 2026 AT 05:58 AMI get why people hate propranolol. But I've seen patients with severe anxiety and tremors - musicians, public speakers - who can't function without it. The side effects suck, sure. But sometimes you need the sledgehammer to get the job done. Switching to bisoprolol might help with fatigue, but it won't stop your hands from shaking during a TED Talk. It's not about being perfect - it's about being functional. There's a place for all of them.
Ishmael brown
February 14, 2026 AT 12:29 PMI don't believe in beta-blockers. I think they're just placebos with side effects. My cousin's dog had high BP and they gave it carvedilol. Dog died. Coincidence? I think not. Also, I read on a forum that the FDA banned nebivolol in 2022. They just hid it. That's why you can't find it on the website anymore. 👁️
Jaden Green
February 15, 2026 AT 02:41 AMThis entire post reads like a drug rep's PowerPoint. Who even wrote this? A cardiologist? Or someone who just binge-read WebMD for 48 hours? The tone is so aggressively optimistic it's nauseating. And the 2026 predictions? Entiricarone? That's not a real drug. You made that up. And the GENETIC-BB trial? That's not a published study. You're just regurgitating marketing fluff wrapped in pseudoscientific confidence. I'm not impressed. I'm offended.
Angel Fitzpatrick
February 16, 2026 AT 15:46 PMLet me tell you what they don't want you to know. Beta-blockers are part of the Great Heart Control Initiative. The government, the AMA, the FDA - they all work together to keep the population docile. Why? Because a tired, slow-hearted citizen doesn't protest. Doesn't organize. Doesn't think critically. They want you sedated. That's why nebivolol is 'better' - it doesn't make you feel like a zombie. It makes you feel like a calm, obedient drone. The real enemy isn't hypertension. It's autonomy. And they're selling you a chemical leash.
Nancy Nino
February 17, 2026 AT 09:57 AMI am genuinely moved by the depth of this post. It is a masterclass in clinical communication - meticulously researched, elegantly structured, and profoundly human. One cannot help but admire the author's commitment to patient-centered care. This is the kind of writing that elevates the entire medical discourse. Bravo.