

When looking at Prednisone Comparison, a side‑by‑side look at how prednisone stacks up against other steroids, dosing schemes, and safety considerations. Also known as prednisone dosage guide, this comparison helps patients and providers decide when the drug fits best and where alternatives might work better.
At the core of any prednisone comparison is the drug itself. Prednisone, a synthetic glucocorticoid that reduces inflammation and suppresses immune activity is prescribed for conditions ranging from asthma to autoimmune disorders. Because it’s so versatile, clinicians often tweak the dose, the schedule, and the tapering speed. That’s why understanding Corticosteroids, the broader drug class that includes prednisone, methylprednisolone, and dexamethasone matters: each member has a unique potency, half‑life, and side‑effect fingerprint. When you compare prednisone to its cousins, you’ll see that potency (measured in milligrams of glucocorticoid activity) directly influences how quickly symptoms improve, but it also dictates the risk of adverse effects like weight gain, mood swings, or bone loss. In practice, a prednisone comparison often hinges on three semantic triples: **Prednisone comparison encompasses dosage variations**, **Prednisone requires careful tapering**, and **Side effects influence steroid choice**. These relationships guide doctors in picking the right strength, duration, and follow‑up plan.
Beyond the drug itself, a solid prednisone comparison must address the practical steps of tapering and monitoring. A gradual reduction—sometimes called a taper—helps the adrenal glands resume natural cortisol production and minimizes withdrawal symptoms. Studies show a taper rate of 5‑10% per week works well for most moderate courses, but high‑dose or long‑term users may need a slower, personalized plan. The tapering process also intertwines with side‑effect management. Side effects, the unwanted reactions such as hyperglycemia, hypertension, and osteoporosis that can arise from steroid therapy are not static; they evolve with dose changes. For example, a patient on 40 mg daily will experience more pronounced blood‑sugar spikes than someone on 5 mg, making diabetes monitoring a must. Likewise, bone health becomes a concern after several weeks of high‑dose therapy, prompting calcium, vitamin D, and possibly bisphosphonate use. By mapping these side effects to specific dosage thresholds, the prednisone comparison becomes a tool for proactive risk reduction rather than a reactionary checklist.
Finally, any thorough prednisone comparison should explore alternative steroids and non‑steroidal options that might offer similar benefits with fewer drawbacks. Methylprednisolone, for instance, has a slightly higher anti‑inflammatory potency per milligram and a shorter half‑life, which can be advantageous for short‑burst treatments. Dexamethasone is far more potent and often reserved for severe cases, but its long‑acting nature raises the bar for tapering complexity. On the non‑steroidal side, biologics like TNF‑alpha inhibitors or JAK inhibitors can replace chronic prednisone use in conditions like rheumatoid arthritis, cutting down on steroid‑related side effects altogether. Understanding where these alternatives fit within the broader treatment landscape turns a simple dosage chart into a strategic roadmap for long‑term health.
In the sections that follow, you’ll find articles that dive deeper into each of these areas: detailed dosage tables, step‑by‑step taper guides, side‑effect monitoring checklists, and side‑by‑side reviews of common steroid alternatives. Use this curated knowledge to tailor your therapy, ask the right questions at your next appointment, and stay ahead of potential complications. The collection below offers practical insights to help you make informed decisions about prednisone and its place in your treatment plan.
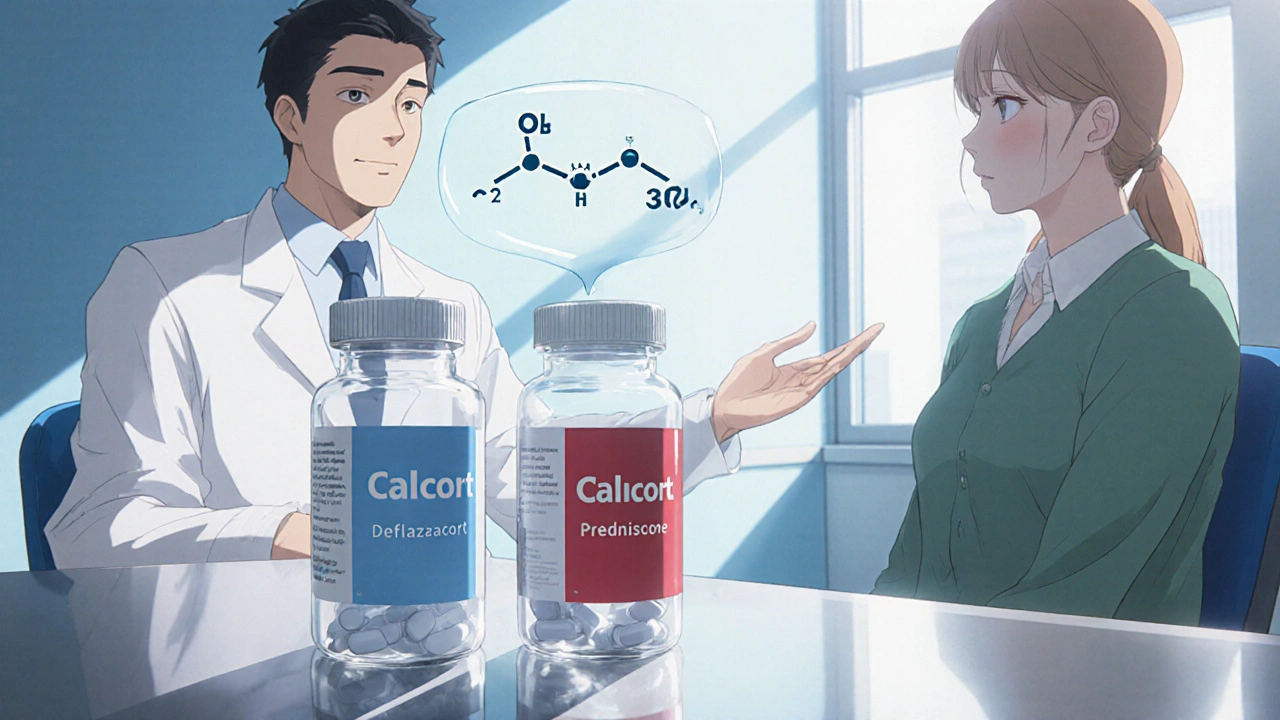
A detailed comparison of Calcort (Deflazacort) with prednisone, methylprednisolone and hydrocortisone, covering potency, dosing, side effects and best use cases.