

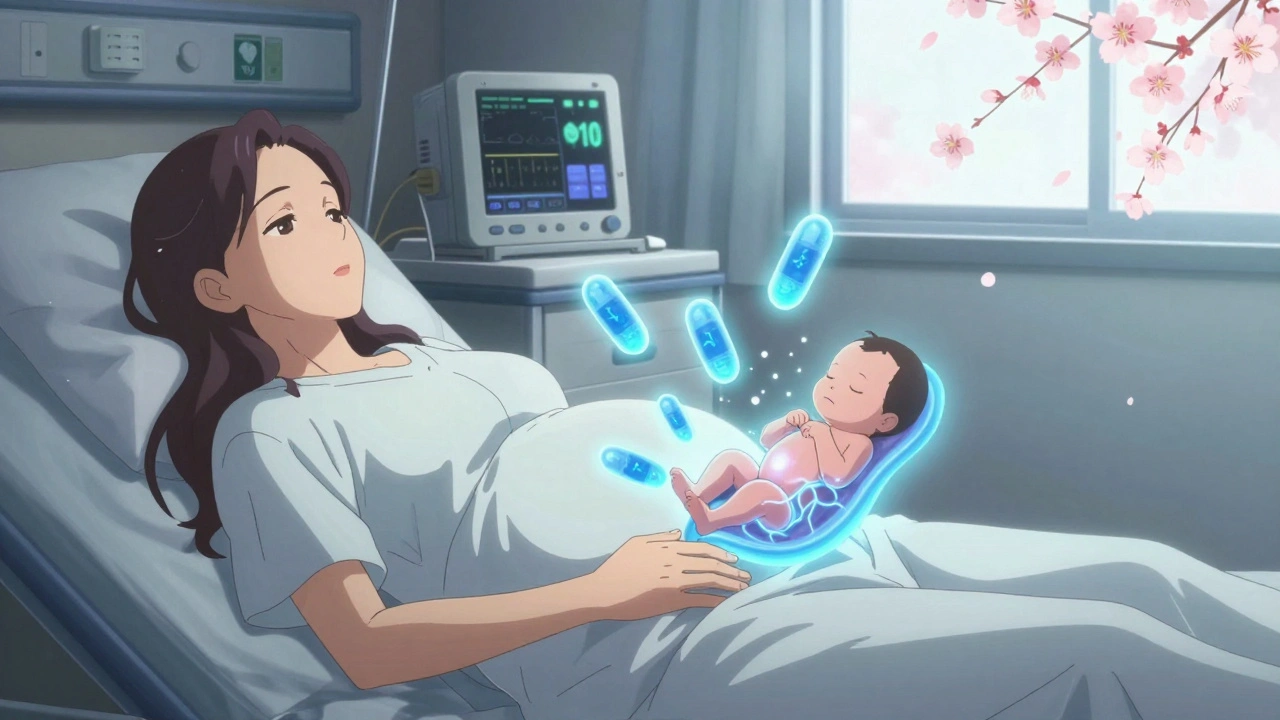
When someone takes opioids during pregnancy, a class of powerful pain-relieving drugs that include prescription painkillers and illegal substances like heroin. Also known as narcotics, these drugs cross the placenta and directly affect the developing fetus, leading to serious, long-lasting consequences. This isn’t just about addiction—it’s about how a baby’s nervous system adapts to drugs before birth, often resulting in life-altering withdrawal after delivery.
The most common outcome is neonatal abstinence syndrome, a group of problems a newborn experiences when withdrawing from exposure to opioids in the womb. Also known as NAS, it causes tremors, seizures, feeding trouble, and extreme crying—sometimes requiring weeks of hospital care. Studies show that up to 60% of babies exposed to opioids in utero develop NAS, and the severity depends on the type, dose, and timing of exposure. It’s not just about street drugs either—prescriptions like oxycodone, hydrocodone, or methadone carry the same risks if used without careful medical oversight.
That doesn’t mean every pregnant person on opioids needs to stop cold turkey. Abruptly quitting can trigger miscarriage or premature labor. The safest path forward often involves medication-assisted treatment, using FDA-approved drugs like methadone or buprenorphine to stabilize the mother and reduce harm to the baby. Also known as MAT, this approach is backed by the CDC and American College of Obstetricians and Gynecologists as the gold standard for managing opioid dependence in pregnancy. These medications don’t cure addiction, but they help avoid the dangerous rollercoaster of withdrawal and relapse, giving both mother and baby a better shot at health.
Many people worry about judgment or losing custody if they admit to opioid use. But the goal today isn’t punishment—it’s support. Doctors, nurses, and social workers are trained to help, not report. Talking early means getting better care: prenatal monitoring, mental health services, and connections to community programs that make a real difference.
And while opioids are often used for pain, there are safer options for managing chronic pain during pregnancy—like physical therapy, acupuncture, or non-opioid meds like acetaminophen. Even if you’ve been on opioids before pregnancy, there’s still time to switch to a safer plan. The key is to act, not hide.
Below, you’ll find real, practical guides from trusted sources on how opioids affect newborns, what treatment looks like, how to spot warning signs, and what alternatives actually work. No fluff. No fear-mongering. Just clear, evidence-based info to help you make informed choices—for yourself and your baby.
Opioid use during pregnancy requires careful medical management. Learn the risks of withdrawal, how MAT with methadone or buprenorphine helps, what to expect with neonatal withdrawal, and why breastfeeding is often safe.