

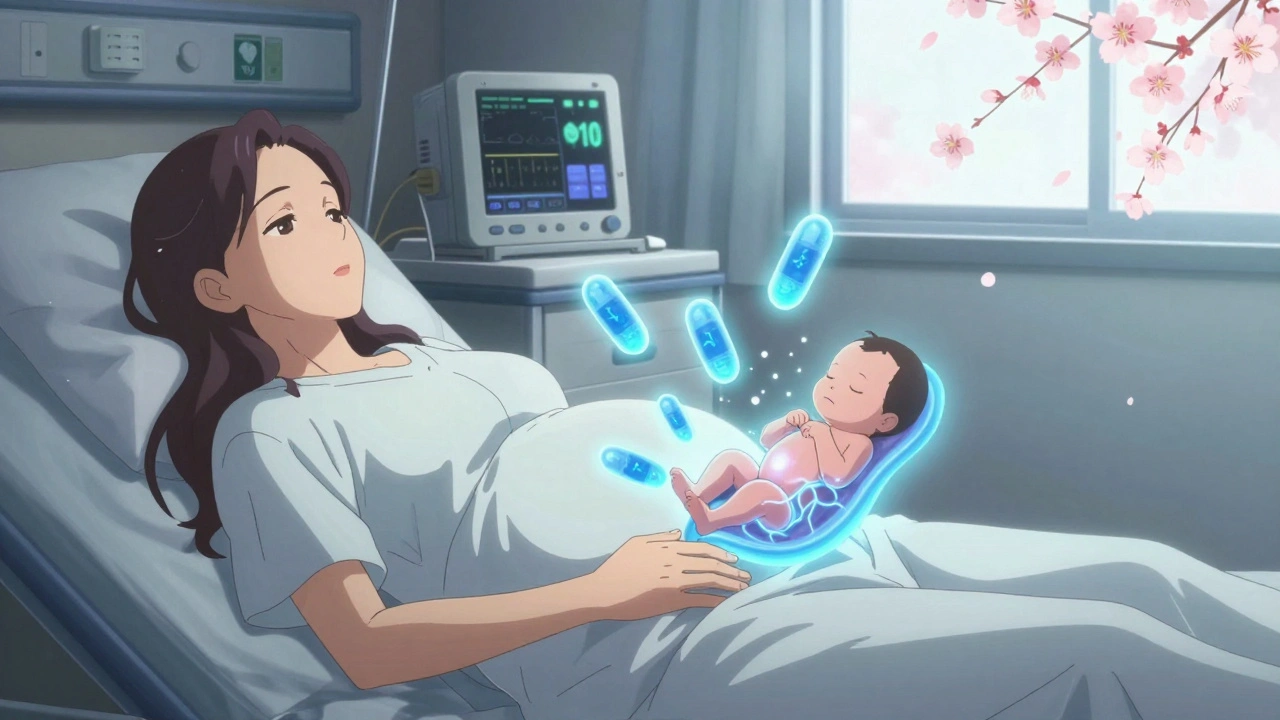
When someone is pregnant and living with opioid use disorder, a chronic condition where the use of opioids like heroin or prescription painkillers becomes compulsive and harmful. Also known as substance use disorder, it affects thousands of pregnant people each year—and medication-assisted treatment is the most effective way to manage it. MAT isn’t just about reducing cravings—it’s about giving both mother and baby a real chance at health. Unlike quitting cold turkey, which can trigger dangerous withdrawal and even miscarriage, MAT uses FDA-approved medications to stabilize the body and support a safer pregnancy.
Buprenorphine, a partial opioid agonist used to treat addiction without causing the same highs or respiratory risks as full opioids is now the first-choice medication for MAT in pregnancy. It’s safer than methadone for most patients, causes less neonatal abstinence syndrome (NAS), and allows more flexibility in dosing and care. Methadone, a full opioid agonist with decades of use in pregnancy is still used, especially when buprenorphine isn’t available or doesn’t work well. Both are proven to reduce the risk of preterm birth, low birth weight, and stillbirth. The goal isn’t to replace one drug with another—it’s to give the body a steady, controlled dose so it doesn’t go into shock, allowing the fetus to develop normally.
Many people still believe MAT in pregnancy is just swapping one addiction for another. That’s a myth. Studies show babies born to mothers on MAT have better outcomes than those born to mothers who quit abruptly or used street drugs. MAT doesn’t mean you’re not trying hard enough—it means you’re choosing science over stigma. You’re not just protecting yourself—you’re protecting your baby’s brain, lungs, and heart.
What you won’t find in most online guides is how MAT fits into real life: how to find a provider who doesn’t judge, how to manage appointments while working or caring for other kids, how to handle family pressure to go "drug-free." That’s why the posts below cover everything from how buprenorphine crosses the placenta to what to expect during labor, how to spot early signs of NAS in newborns, and how to talk to your OB-GYN without feeling ashamed. You’ll also find advice on avoiding dangerous drug interactions—like mixing MAT meds with benzodiazepines or alcohol—and how to stay on track when life gets messy. This isn’t theoretical. These are the tools real people use to survive and thrive.
Opioid use during pregnancy requires careful medical management. Learn the risks of withdrawal, how MAT with methadone or buprenorphine helps, what to expect with neonatal withdrawal, and why breastfeeding is often safe.