

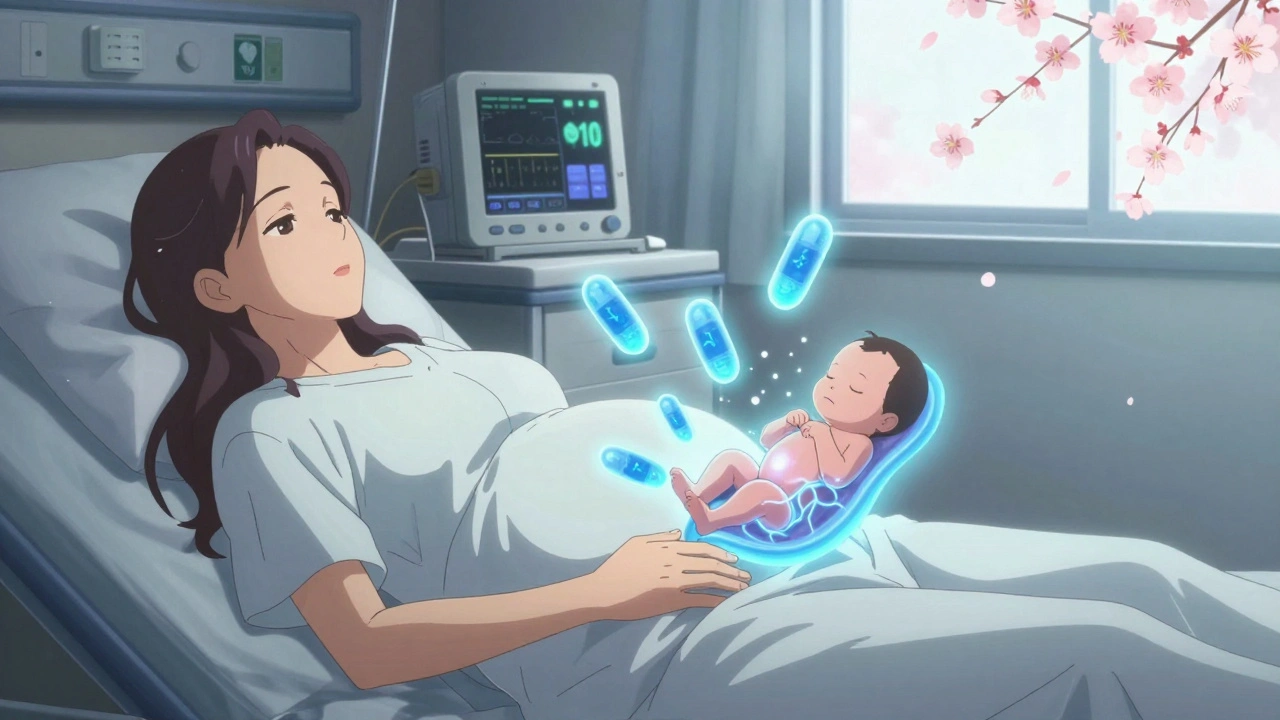
When someone is pregnant and using opioids, buprenorphine, a partial opioid agonist used to treat opioid use disorder. Also known as Subutex or Suboxone, it is one of the two main medications approved for use during pregnancy to help manage addiction safely. Unlike quitting cold turkey—which can trigger miscarriage or preterm labor—buprenorphine stabilizes brain chemistry, reduces cravings, and lowers the risk of overdose. It’s not a cure, but it gives both mother and baby a much better shot at a healthy outcome.
One of the biggest concerns with any opioid during pregnancy is neonatal abstinence syndrome, a group of problems that occur in newborns exposed to opioids before birth. Babies born to mothers on buprenorphine can still experience withdrawal symptoms like tremors, excessive crying, feeding trouble, and sleep issues. But studies show these symptoms are often milder and shorter-lived than with methadone. The American College of Obstetricians and Gynecologists recommends buprenorphine as a first-line option because it’s easier to manage, has fewer side effects, and lets moms stay more alert and involved in early care.
It’s not just about the drug—it’s about the whole system. medication-assisted treatment, a combination of FDA-approved medication and counseling. Works best when paired with prenatal care, mental health support, and social services. Many women on buprenorphine also take other meds—like antidepressants or prenatal vitamins—and interactions matter. You can’t just take it and hope for the best. Regular check-ins with a provider who knows opioid treatment in pregnancy are non-negotiable.
Some people worry buprenorphine is just swapping one addiction for another. That’s not true. It’s medical care, like insulin for diabetes. The goal isn’t to get off it by the third trimester—it’s to keep mom stable so the baby grows right and the birth goes smoothly. Cutting back too early increases relapse risk, which is far more dangerous than staying on a controlled dose.
What about breastfeeding? Yes, it’s usually safe. Small amounts of buprenorphine pass into breast milk, but babies rarely show signs of sedation or withdrawal. In fact, breastfeeding may even help ease withdrawal symptoms after birth. The key is consistency: same dose, same schedule, same provider. No sudden changes.
There’s no perfect answer, but the data is clear: staying on buprenorphine under medical supervision is safer than using street opioids or trying to quit alone. The real risk isn’t the medication—it’s the lack of support. If you’re pregnant and using opioids, you’re not failing. You’re fighting. And help exists.
Below, you’ll find real, practical guides on how buprenorphine affects newborns, how to manage side effects during pregnancy, what to ask your doctor, and how other moms have navigated this path—without judgment, without fluff, just facts that matter.
Opioid use during pregnancy requires careful medical management. Learn the risks of withdrawal, how MAT with methadone or buprenorphine helps, what to expect with neonatal withdrawal, and why breastfeeding is often safe.