It’s 2025, and more Americans than ever are taking SSRIs. About 1 in 8 adults uses one of these antidepressants - fluoxetine, sertraline, escitalopram - to manage depression, anxiety, or OCD. But behind the numbers is a quiet, growing danger: serotonin syndrome. This isn’t a rare side effect. It’s a medical emergency that can turn a simple medication combo into a life-threatening situation. And most people have no idea it’s even possible.
What Exactly Is Serotonin Syndrome?
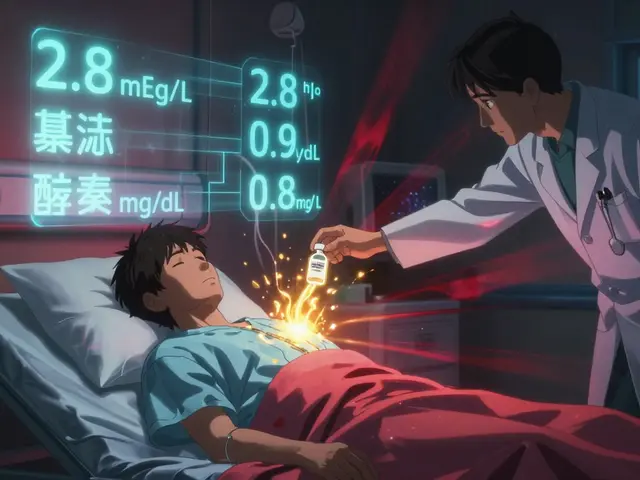
Serotonin syndrome isn’t just feeling “too wired” or having a headache. It’s a dangerous overload of serotonin in your brain and nervous system. Think of serotonin as a chemical messenger. SSRIs stop your brain from reabsorbing it, so more stays around to help lift your mood. But when you add another drug that also boosts serotonin - even something you think is harmless - your body can’t handle the flood. The symptoms don’t sneak up. They hit fast. Muscle rigidity. High fever. Shivering. Confusion. Involuntary jerking movements. Sweating so much your clothes soak through. In severe cases, seizures, irregular heartbeat, or loss of consciousness follow. If you’re on an SSRI and suddenly feel like you’re melting from the inside out, don’t wait. Go to the ER. Doctors now use the Hunter Criteria to diagnose it - not just symptoms, but specific combinations. If you have spontaneous clonus (involuntary muscle spasms) or ocular clonus (eyes darting uncontrollably) along with fever or agitation, it’s serotonin syndrome until proven otherwise.Which Medications Are the Biggest Risks?
Not all drug combos are equal. Some are ticking bombs. Others are low-risk. Here’s what actually matters:- MAOIs - These are the worst. Never, ever mix them with SSRIs. The risk is so high that doctors require a 2-week to 5-week gap between stopping one and starting the other. Fluoxetine’s long half-life means you might need to wait five weeks after quitting Prozac before starting an MAOI. This isn’t a suggestion - it’s a life-or-death rule.
- Linezolid - This antibiotic, used for stubborn infections like MRSA, is a hidden danger. It acts like a weak MAOI. A 2022 study found patients over 65 on SSRIs who took linezolid had nearly 3 times the risk of serotonin syndrome. It’s rare, but it happens - and it’s deadly when it does.
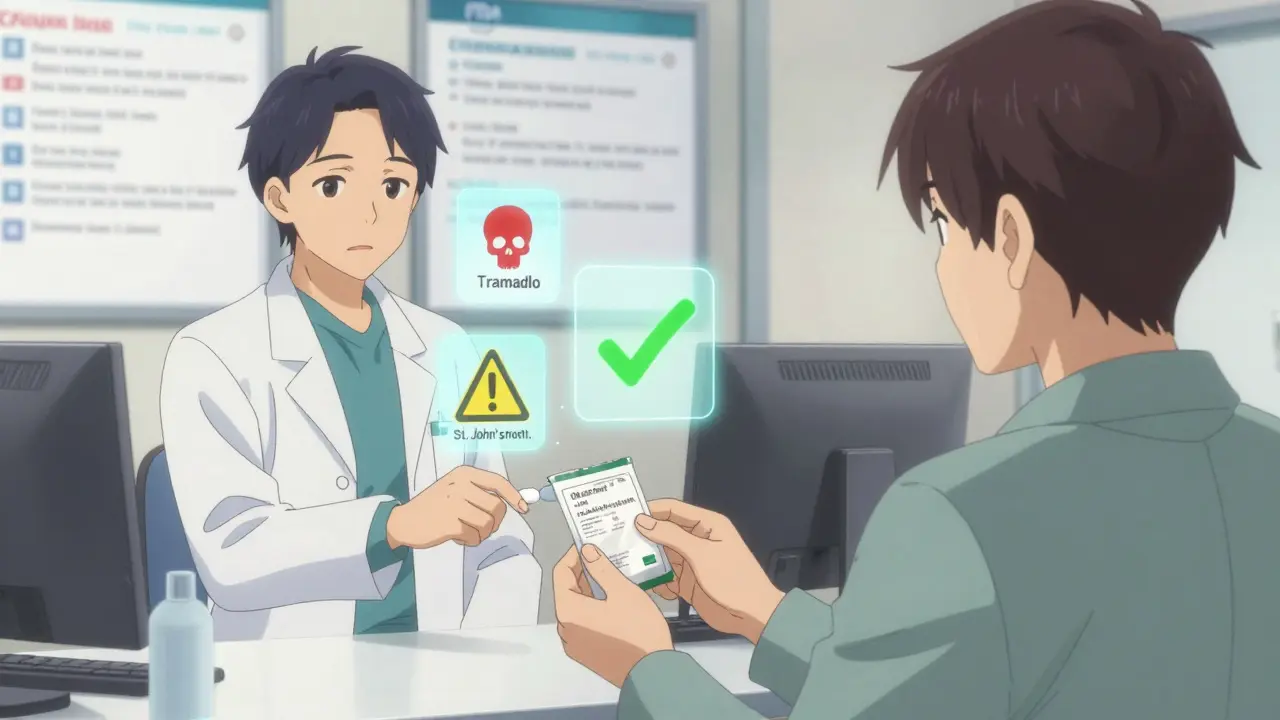
- Tramadol, dextromethorphan, pethidine - These aren’t just painkillers. Tramadol, often prescribed for back pain, has a double effect: it’s an opioid and a serotonin booster. Dextromethorphan is in many cough syrups. Pethidine is an older painkiller still used in hospitals. All three raise serotonin levels sharply. When combined with SSRIs, the risk jumps 4.7 times. That’s not a small increase - that’s a red flag.
- SNRIs - Venlafaxine, duloxetine, desvenlafaxine - these are also antidepressants, but they target both serotonin and norepinephrine. Mixing them with SSRIs triples the risk of serotonin syndrome. Many patients get both prescribed for “treatment-resistant depression.” That’s a dangerous gamble.
- Herbal supplements - St. John’s wort is the most common offender. People think “natural” means safe. It doesn’t. It boosts serotonin just like an SSRI. One Reddit user reported severe shivering and confusion after just three days of combining it with Prozac. ER visits followed.
What About Opioids? Not All Are Equal
Pain management is a huge reason people end up on SSRIs - chronic back pain, arthritis, fibromyalgia. But opioids? They’re not all the same when it comes to serotonin.- High risk: Tramadol, dextromethorphan, pethidine - avoid completely if you’re on an SSRI.
- Medium risk: Methadone, fentanyl - use with extreme caution. Monitor closely.
- Low risk: Morphine, codeine, oxycodone, buprenorphine - these don’t significantly raise serotonin. If you need an opioid, these are safer choices.
Who’s Most at Risk?
It’s not just about what you take - it’s who you are.- People over 65: 21.5% take SSRIs. 18.3% take opioids. 22% take five or more medications. The odds of a bad combo skyrocket.
- People on multiple antidepressants: 3.2 times higher risk when combining SSRIs with SNRIs or trazodone.
- People with genetic differences: About 7% of people are “poor metabolizers” of CYP2D6 - a liver enzyme that breaks down tramadol and some SSRIs. If you’re one of them, even normal doses can cause serotonin overload.
- People who self-medicate: St. John’s wort, tryptophan, 5-HTP - these are sold as “natural mood boosters.” No one warns you they can kill you when mixed with your prescription.
How to Stay Safe
You don’t have to live in fear. You just need to be smart.- Know your meds. Make a list - all of them. Prescription, OTC, supplements. Bring it to every appointment.
- Ask your pharmacist. Pharmacists are trained to catch dangerous combos. A 2023 study showed pharmacist-led reviews cut serotonin syndrome events by 47% in Medicare patients.
- Use the 5 S’s as a warning system: Shivering, Sweating, Stiffness, Seizures (rare), Sudden confusion. If you notice two or more, seek help immediately.
- Never start a new med without asking about serotonin risk. Even if it’s for a cold or pain. Say: “I’m on an SSRI. Is this safe?”
- Don’t stop SSRIs cold turkey. Withdrawal can mimic serotonin syndrome symptoms. Always taper under medical supervision.
What’s Changing in 2025?
The system is finally waking up. In 2024, the FDA mandated that all electronic prescribing systems must now include mandatory alerts for high-risk SSRI combinations - especially with tramadol, linezolid, and MAOIs. Hospitals using Epic, Cerner, and Allscripts have already seen a 32% drop in dangerous co-prescriptions. The CDC now explicitly advises doctors to avoid tramadol and dextromethorphan in SSRI users. Instead, they recommend morphine or oxycodone for pain. And by 2026, a blood test called SerotoninQuant may become available - the first objective way to confirm serotonin syndrome, not just guess based on symptoms.Bottom Line
SSRIs are life-changing for millions. But they’re not harmless. The biggest threat isn’t the drug itself - it’s what you mix it with. Most cases of serotonin syndrome are preventable. They happen because someone didn’t know, or didn’t ask. If you’re on an SSRI, talk to your doctor. Ask: “What else am I taking that could raise my serotonin?” Don’t assume your painkiller, cough syrup, or herbal supplement is safe. The risk is real. But so is your power to avoid it.Can serotonin syndrome happen with just one SSRI?
It’s extremely rare. Serotonin syndrome almost always happens when an SSRI is combined with another drug that also increases serotonin - like an SNRI, tramadol, MAOI, or St. John’s wort. Taking an SSRI alone at the right dose rarely causes it.
How long does it take for serotonin syndrome to develop?
Symptoms usually appear within hours - often within 6 to 12 hours after taking a new medication or increasing a dose. In rare cases, it can take up to 24 hours. If you feel suddenly unwell after starting something new, don’t wait.
Is serotonin syndrome fatal?
Yes, it can be. If untreated, severe serotonin syndrome can lead to seizures, organ failure, or death. The mortality rate for MAOI-SSRI combinations can be as high as 30-50%. Even with treatment, hospitalization is often needed. Early recognition saves lives.
Can I take ibuprofen or acetaminophen with an SSRI?
Yes. Neither ibuprofen nor acetaminophen affects serotonin levels. These are safe for pain relief while on SSRIs. The danger comes from opioids like tramadol, cough medicines with dextromethorphan, or herbal supplements - not standard pain relievers.
What should I do if I think I have serotonin syndrome?
Stop all non-essential medications immediately. Call 911 or go to the nearest emergency room. Tell them you’re on an SSRI and suspect serotonin syndrome. Time is critical. Treatment includes stopping the triggering drugs, cooling the body, and sometimes giving serotonin blockers like cyproheptadine.
Are there any safe alternatives to tramadol for pain if I’m on an SSRI?
Yes. Morphine, oxycodone, and buprenorphine are considered low-risk for serotonin syndrome when used with SSRIs. Non-opioid options like gabapentin, physical therapy, or NSAIDs (ibuprofen, naproxen) are also effective for many types of chronic pain. Talk to your doctor about switching.
Why do doctors sometimes prescribe risky combos anyway?
Sometimes it’s because they’re unaware - especially with over-the-counter meds or supplements. Other times, it’s because the patient’s pain or depression is severe, and safer options haven’t worked. But with better alerts, pharmacist support, and patient education, these mistakes are becoming less common.
Can I use St. John’s wort if I’m on a low-dose SSRI?
No. Even low-dose SSRIs can trigger serotonin syndrome when combined with St. John’s wort. There’s no safe threshold. The interaction is predictable and dangerous. Skip the supplement. Your SSRI is already doing the job.









Comments (9)
Adarsh Dubey
December 23, 2025 AT 20:07 PMWow, this is one of the most clearly laid-out guides on SSRI risks I’ve ever read. The breakdown of tramadol vs. oxycodone alone could save lives. I’m an Indian pharmacist, and I see this mix-up way too often - people popping St. John’s wort like candy while on sertraline, thinking ‘natural’ = harmless. It’s not. The 47% drop in events with pharmacist reviews? That’s the future. We need this everywhere.
Usha Sundar
December 25, 2025 AT 19:33 PMMy uncle died from this. No one warned him.
Dan Gaytan
December 26, 2025 AT 19:40 PMThank you for this 🙏 I’ve been on escitalopram for 3 years and just last month my doc prescribed tramadol for my back. I asked about serotonin risk - he paused, said ‘oh wow, good catch,’ and switched me to oxycodone. You’re right - we have to ask. I’m sharing this with my whole family.
Payson Mattes
December 28, 2025 AT 14:55 PMLet me guess - this was funded by Big Pharma. 🤔 They want you scared of herbal stuff so you keep buying pills. St. John’s wort has been used for centuries. The FDA just wants you dependent. And why are they pushing this ‘SerotoninQuant’ blood test? To make you pay more. Wake up. They’re hiding the real cause: chronic stress from capitalism. Your body’s not broken - the system is.
Chris Buchanan
December 30, 2025 AT 09:17 AMSo let me get this straight - you’re telling me my NyQuil might be a death trap? 😳 Bro, I’ve been chugging that stuff since college. And now you say dextromethorphan + Zoloft = bad news? I feel like I’ve been playing Russian roulette with my brain. Thanks for the wake-up call… now I gotta go throw out my cough syrup. 💀
claire davies
January 1, 2026 AT 00:44 AMI’m from the UK and I’ve seen this play out in my own circle - a dear friend, mid-60s, on fluoxetine for anxiety, started taking St. John’s wort after reading a ‘natural healing’ blog. Three days later, she was in A&E with tremors and confusion. Her GP said, ‘We didn’t even think to ask about supplements.’ That’s the problem. We assume ‘natural’ means ‘no doctor needed.’ But your liver doesn’t care if it’s a pill or a leaf - it just sees serotonin. This post should be mandatory reading for every adult over 18. And yes, I’ve printed it out and left it on my mum’s fridge.
Austin LeBlanc
January 1, 2026 AT 06:42 AMAnyone else notice how this post is just fear-mongering dressed up as ‘education’? SSRIs are overprescribed, sure - but now we’re supposed to be terrified of every cough drop and painkiller? What’s next? ‘Don’t breathe near someone on antidepressants’? People need to take responsibility for their own health, not turn every pharmacy into a war zone. I’ve been on sertraline for 7 years. I take ibuprofen, melatonin, and fish oil. I’m fine. Not everyone’s a walking serotonin bomb.
Andrea Di Candia
January 3, 2026 AT 01:15 AMThere’s something deeply human here - we’re all trying to feel better, but we’re so afraid to talk about it. We take pills because we’re tired. We grab herbs because we don’t trust doctors. We ignore symptoms because we don’t want to be ‘that person’ who’s always sick. But this isn’t about drugs. It’s about care. The fact that a pharmacist’s review cuts risk by nearly half? That’s not just data - that’s compassion in action. We need more of that. Not just in prescriptions, but in how we listen to each other.
Joseph Manuel
January 4, 2026 AT 01:44 AMThe data presented is statistically significant and clinically relevant. However, the omission of pharmacokinetic variables - specifically CYP2D6 and CYP3A4 polymorphisms - diminishes the rigor of the risk stratification. Furthermore, the assertion that ‘serotonin syndrome is almost always polypharmacy-induced’ is empirically flawed; case reports exist of monotherapy-induced syndromes following dose escalation in vulnerable populations, particularly in the elderly. The FDA alert mandate is commendable, yet without genetic screening protocols, population-level risk reduction remains suboptimal. Recommend updating guidelines to include preemptive genotyping for high-risk patients.