When you’re managing asthma or COPD, your inhaler isn’t just a tool-it’s your lifeline. But what happens when your pharmacy switches your Symbicort or Advair to a cheaper generic version without telling you? For many, it’s not just a change in packaging. It’s a change in how you breathe.
Why Generic Inhalers Aren’t Like Generic Pills
You might think switching from a branded inhaler to a generic one is like swapping one pill for another. It’s not. With pills, the active ingredient is what matters. With inhalers, the device is just as important as the medicine. Combination inhalers deliver two drugs at once-usually a corticosteroid to reduce inflammation and a long-acting beta agonist to open airways. Brands like Symbicort, Advair, and Dulera have been the standard for years. But as patents expire, generics like DuoResp Spiromax and other alternatives are hitting shelves. The problem? These generics often use different inhaler devices. And those devices don’t work the same way. A Turbuhaler requires you to twist the base to load a dose. A Spiromax uses a side slider. A pMDI needs you to press and breathe in at the same time. A DPI demands a strong, fast breath. If you’ve used the same inhaler for five years and suddenly get a new one without training, you might be inhaling less than half the dose you think you are.The Data Doesn’t Lie: Substitution Can Hurt
A 2021 study published in the Journal of Aerosol Medicine and Pulmonary Drug Delivery tracked patients switched from Symbicort Turbohaler to the generic Spiromax without any instruction. Within six months, those patients had a 22% increase in asthma attacks. Another study found that 76% of people using the new device without training got the technique wrong. Only 24% got it right-because they were shown how. In the UK, a survey of 1,247 people found that 57% felt confused after being switched to a different inhaler. One in three ended up in the emergency room within three months. On Drugs.com, Symbicort Turbohaler has a 6.2/10 rating. The generic Spiromax? 4.8/10. The top complaints? “Harder to use,” “feels less effective,” “I didn’t know I had to breathe harder.” This isn’t about cost. It’s about control. When your inhaler doesn’t work right, your lungs suffer. And when your lungs suffer, your life slows down.Regulations Are All Over the Map
In the U.S., the FDA says generic inhalers are interchangeable. Their stance? If the drug is the same, the device shouldn’t matter. You’re supposed to use the generic without extra training. In Europe, the EMA says no. They require proof that the generic delivers the same amount of medicine to the lungs as the original. They even demand clinical studies showing no drop in patient outcomes. And they’re clear: switching without consent and training is risky. The UK’s NICE guidelines are even clearer: “Switching inhaler devices without a consultation may be associated with worsened asthma control.” That’s not a suggestion. It’s a warning. And yet, in many places, pharmacists are still allowed to swap inhalers automatically. Why? Because the law treats them like pills. But the science says otherwise.What Happens When No One Shows You How
Imagine this: You’ve been using your Turbuhaler for years. You know the twist. You know the breath. You know the rhythm. One day, your prescription comes back-and it’s a Spiromax. No note. No call. Just a different-looking device in your hand. You don’t realize you need to slide the lever instead of twist. You don’t know you now need to inhale faster and harder. You think, “This isn’t working.” So you use it more. You press harder. You breathe faster. You end up with a dry throat, a racing heart, and a flare-up that lands you in A&E. A 2022 study found that only 28% of community pharmacies in the U.S. consistently provide training when switching inhalers. The rest? They hand you the box and say, “This is your new one.” Even doctors aren’t always prepared. One study showed that 43% of general practitioners couldn’t demonstrate correct technique for either the Turbuhaler or Spiromax. How can they teach you if they don’t know how to use it themselves?How to Protect Yourself
You don’t have to be caught off guard. Here’s what you can do:- Ask before you pick up: “Is this the same device as before?” If the answer is no, ask for a demonstration.
- Request a teach-back: After your pharmacist shows you, do it yourself. If you can’t do it right, say so. They need to keep showing you until you get it.
- Check your prescription: If your doctor wrote “dispense as written” or “do not substitute,” your pharmacy is legally required to honor that.
- Know your device: Take a photo of your inhaler. Write down the steps. Keep it in your phone. If you’re switched, compare.
- Speak up if you feel worse: If your symptoms change after a switch, tell your doctor immediately. Don’t wait. Don’t assume it’s your condition getting worse. It might be the device.
The Bigger Picture: Cost vs. Consequences
Yes, generics save money. But the savings are misleading. A 2023 IMS Health report found that inappropriate inhaler substitution costs healthcare systems $1.2 billion a year in emergency visits, hospital stays, and missed work. That’s more than the total savings from switching to cheaper inhalers. Countries like Norway have high generic use-62% of respiratory inhalers are generic. But they also have strong training programs. France, where brand-name prescribing is the norm, has lower substitution rates-and lower rates of hospitalizations from inhaler errors. The real question isn’t whether generics should exist. It’s whether we’re letting patients pay the price for shortcuts.What’s Changing Now
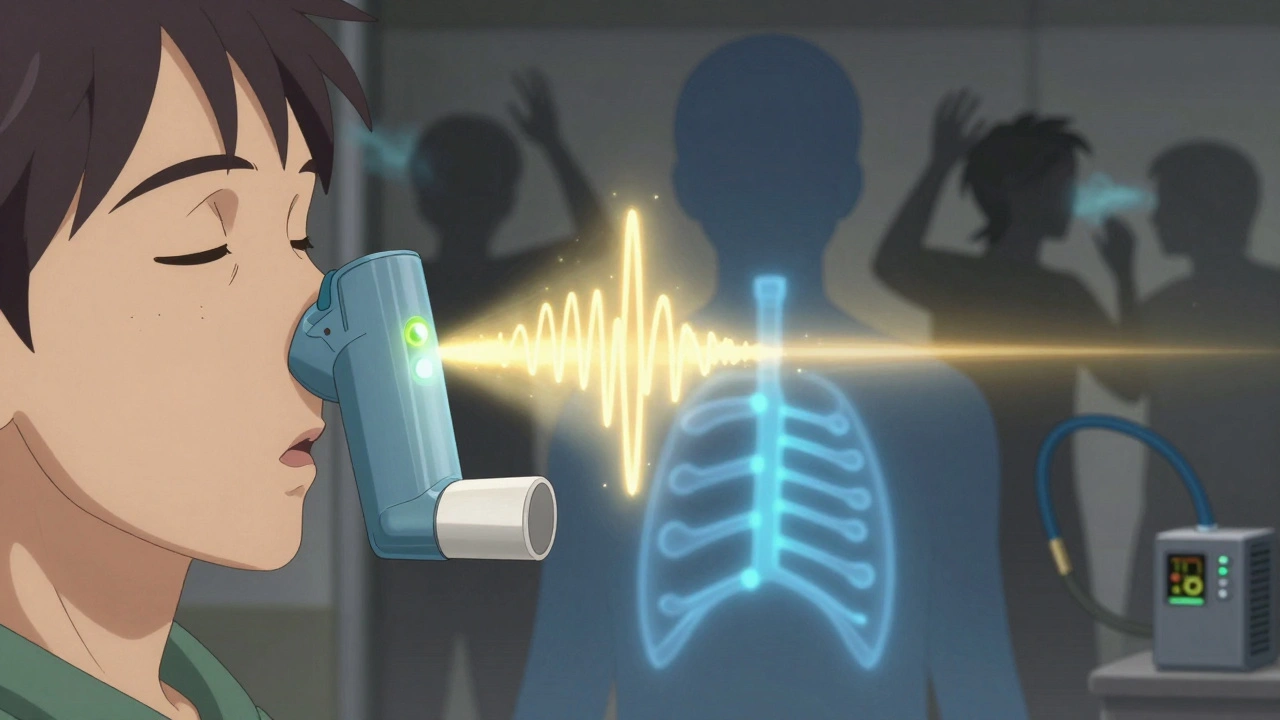
The tide is turning. In 2023, GINA updated its guidelines to say: “Device familiarity and correct technique should be prioritized over generic substitution.” The European Respiratory Society now recommends prescribing by brand name to avoid confusion. The FDA is taking notice too. In May 2023, they released a draft guidance asking for more clinical evidence before approving new inhaler generics. And in the U.S., $25 million has been allocated for research into best practices for inhaler substitution. Smart inhalers-devices with sensors that track your technique-are becoming more common. One study showed that when patients got real-time feedback on their breathing, asthma flare-ups dropped by 33%. The future isn’t just cheaper drugs. It’s smarter care.Bottom Line: Don’t Let a Switch Cost You Your Breath
Generic inhalers aren’t bad. But they’re not the same as the originals-not if the device changes. Your inhaler isn’t a pill. It’s a precision tool. And like any tool, you need to know how to use it. If your pharmacy switches your inhaler, don’t accept it silently. Ask. Learn. Demonstrate. Speak up. Your lungs can’t afford to guess.Can I switch my inhaler without telling my doctor?
No, you shouldn’t. Even if your pharmacy switches it automatically, you should always inform your doctor. Changing inhaler devices can affect how much medicine reaches your lungs. If you notice new symptoms like wheezing, coughing, or needing your rescue inhaler more often, it could be the device-not your condition worsening. Tell your doctor right away.
Are all generic inhalers the same?
No. Generic inhalers may contain the same drugs as the brand-name version, but the device can be completely different. For example, the generic version of Symbicort (DuoResp Spiromax) uses a slider mechanism, while the original uses a twist-to-load Turbuhaler. These differences change how you breathe in, how much medicine you get, and whether it works at all.
Why do pharmacies switch inhalers without asking?
In many places, pharmacy laws allow automatic substitution of generic drugs-just like with pills. But inhalers aren’t pills. The law hasn’t caught up with the science. Pharmacists often switch to save money, assuming the drug is the same. But without training, patients get the wrong dose, which can lead to serious health risks.
How do I know if my inhaler has been switched?
Check the packaging. Look at the device itself. Does it look different? Is the name on the device different from what you’ve used before? Even small changes-like a slider instead of a twist, or a different color-mean it’s a new device. If you’re unsure, ask your pharmacist or check your prescription label. Never assume it’s the same.
What should I do if I’ve been switched and I feel worse?
Contact your doctor immediately. Don’t wait. Bring your new inhaler with you. Ask: “Was I switched? Is this device right for me?” Request a technique check. If your doctor doesn’t know how to demonstrate it, ask for a respiratory nurse or pharmacist who can. You have the right to use a device you know how to use safely.
Can I ask my doctor to prescribe a specific brand?
Yes. You can ask your doctor to write “dispense as written” or “do not substitute” on your prescription. This legally prevents the pharmacy from switching your inhaler without your doctor’s approval. Many patients do this successfully, especially if they’ve had bad experiences with switches in the past.
Is there a way to track if I’m using my inhaler correctly?
Yes. Smart inhalers with built-in sensors can track when you use them and how well you inhale. Devices like Propeller Health or Adherium’s Hailie can connect to your phone and give feedback on your technique. If you’ve been switched or are unsure about your technique, ask your doctor if one of these is right for you. Studies show they reduce asthma attacks by up to 33%.










Comments (11)
Regan Mears
December 11, 2025 AT 08:32 AMI’ve been on Symbicort for eight years-same device, same rhythm. When my pharmacy switched me to Spiromax without a word, I thought I was dying. My lungs felt like they were full of sand. I didn’t know I was breathing wrong until I went to my pulmonologist and she showed me the difference. One slide. One breath. That’s it. But no one told me. No one asked. I almost ended up in the ER. Please, if you’re switching, ask for a demo. It’s not just a pill. It’s your breath.
And if your pharmacist says, ‘It’s the same drug,’ tell them they’re wrong. The device matters. It matters more than you think.
David Palmer
December 12, 2025 AT 06:38 AMBro, just use your rescue inhaler more. That’s what it’s for. Stop overthinking it. I switched to the cheap one and I’m fine. Probably just anxiety.
Doris Lee
December 14, 2025 AT 00:55 AMThis hit me right in the chest. I’ve been there. I’ve been switched without warning. I thought I was failing at managing my asthma-turns out, I was just using the wrong tool. My pharmacist didn’t even notice I was holding it wrong. But once I asked for help? Everything changed. You’re not broken. The device is. Don’t be shy. Ask for help. You deserve to breathe easy.
And if your doctor doesn’t know how to show you? Ask for a respiratory nurse. They’re the real MVPs.
Michaux Hyatt
December 15, 2025 AT 10:53 AMLet me break this down real simple: inhalers aren’t pills. The device is part of the drug delivery system. If you change the device, you change how the medicine gets into your lungs. Period. The FDA’s stance is outdated. Europe and the UK get it. The U.S. is still stuck in the 90s.
Here’s what you can do: 1) Always check the device before you leave the pharmacy. 2) Take a picture of your old one. 3) If it’s different, say ‘I need a demonstration.’ 4) If they refuse, ask for a supervisor. 5) If they still won’t help, file a complaint with the state pharmacy board. You’re not being difficult-you’re being smart.
And yes, smart inhalers? They’re not sci-fi. They’re real. And they work. Ask your doc about them. They’re worth every penny.
Frank Nouwens
December 16, 2025 AT 09:04 AMIt is, indeed, a matter of considerable concern that pharmacological substitution protocols have not evolved in tandem with the biomechanical specificity of inhaler devices. The assumption that bioequivalence of active pharmaceutical ingredients equates to therapeutic equivalence across delivery platforms is, in my professional estimation, scientifically unsound. The data cited in this post are not merely anecdotal; they are statistically significant and clinically actionable. One may reasonably infer that current regulatory frameworks are lagging behind the empirical evidence by at least a decade. It is, therefore, imperative that clinicians and patients alike advocate for policy reform that prioritizes device continuity over cost efficiency.
Kaitlynn nail
December 17, 2025 AT 13:19 PMIt’s not about the inhaler. It’s about control. We’ve been conditioned to trust systems that don’t trust us. The real question: who profits when you gasp for air? Not you. Not your doctor. Someone’s balance sheet. And your breath? It’s just a line item.
Stephanie Maillet
December 18, 2025 AT 12:03 PMIt’s strange, isn’t it? We’ll spend hours choosing the perfect coffee grinder because we care about the flavor-but we hand over our breathing to a machine we’ve never been taught to use? We treat our lungs like they’re disposable, like they don’t deserve the same care we give our cars or our phones. But your breath is the only thing you can’t pause. And yet, we let algorithms and cost-cutting decide how you inhale. That’s not healthcare. That’s neglect dressed up as efficiency.
Maybe the real generic isn’t the inhaler. Maybe it’s compassion.
Jack Appleby
December 19, 2025 AT 22:34 PMLet’s be brutally honest: the FDA’s approval of interchangeable inhalers is a regulatory farce. Bioequivalence ≠ therapeutic equivalence. You can’t measure lung deposition with a spectrophotometer and call it a day. The device’s aerodynamic properties, actuation-to-inhalation delay, particle size distribution, and patient interface dynamics are all critical-and none of them are validated in the current approval pathway. The EMA’s stance isn’t ‘cautious’-it’s scientifically rigorous. The U.S. is playing Russian roulette with patients’ respiratory health, and the only thing worse than the substitution is the ignorance that enables it.
Also, ‘DuoResp Spiromax’ is not a generic-it’s a *different* product. Calling it a ‘generic’ is a semantic fraud. It’s a me-too device with a different patent. The FDA needs to be called out. And pharmacists? They need mandatory training. Not a pamphlet. A live demonstration. With a quiz. And a certification. Because lives aren’t negotiable.
Rebecca Dong
December 21, 2025 AT 06:08 AMTHIS IS A BIG PHARMA SCAM. They know the generics don’t work right. That’s why they’re pushing them. They want you to get sicker so you’ll buy more meds. The FDA is in their pocket. The pharmacy chain? Owned by the same people. They’re letting you die slowly so they can sell you an emergency room visit. And don’t even get me started on ‘smart inhalers’-those are trackers. They’re selling your breathing data. You’re not just getting a bad inhaler-you’re being spied on. Wake up. This isn’t healthcare. It’s a surveillance economy.
Sarah Clifford
December 22, 2025 AT 08:08 AMMy mom got switched and ended up in the hospital. They said it was ‘just a flare-up.’ But she didn’t change anything else. Just the inhaler. Now she won’t use anything but the brand. And she tells everyone. Like, EVERYONE. I think they should just make all the inhalers the same. Or make pharmacies give you a demo. Or something. This is messed up.
Ben Greening
December 22, 2025 AT 09:52 AMInteresting piece. The data on technique failure rates is compelling. I’d be curious to see longitudinal studies comparing long-term outcomes between patients who received structured device training versus those who did not. Also, the cost-benefit analysis presented raises important questions about hidden expenditures in emergency care. The regulatory divergence between the FDA and EMA warrants further policy analysis. Thank you for highlighting this under-discussed issue.