What You Need to Know About Kidney Disease Before It’s Too Late
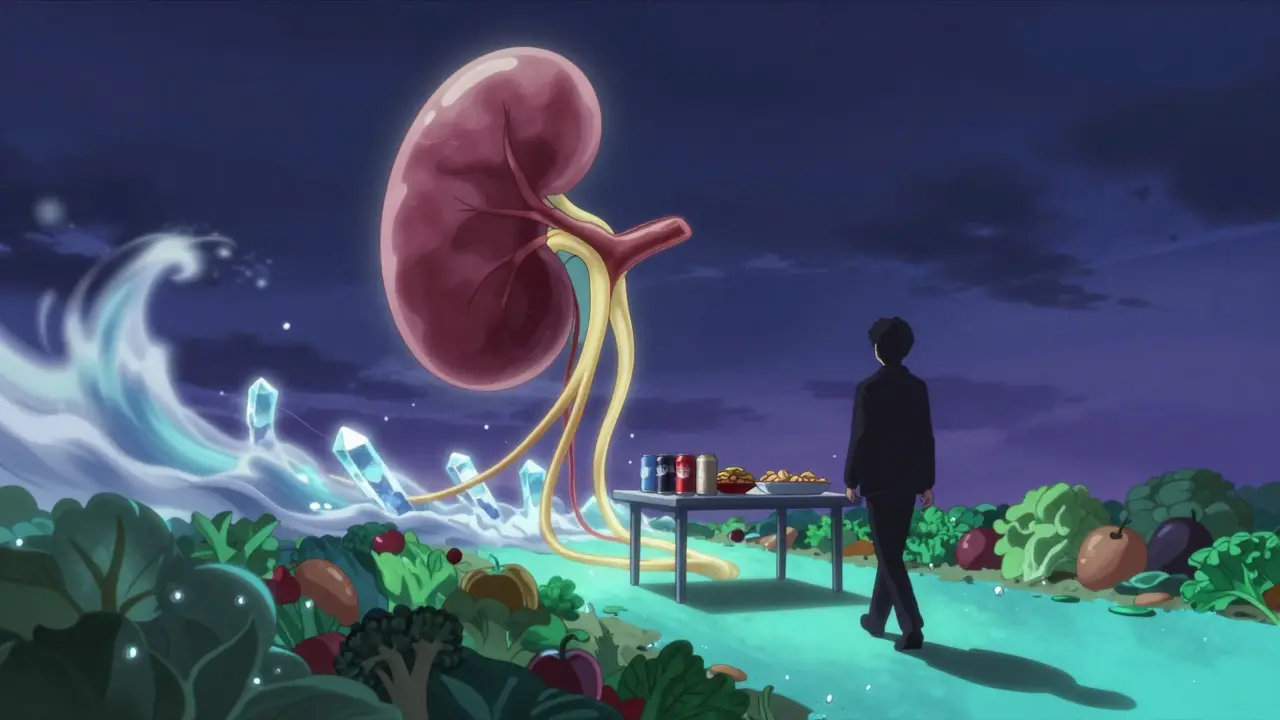
Most people don’t think about their kidneys until something goes wrong. But by then, it’s often too late. Kidney disease doesn’t come with warning signs-no pain, no fever, no obvious symptoms. By the time it’s diagnosed, up to 70% of kidney function may already be gone. The good news? Up to 85% of cases can be prevented or delayed with simple, everyday choices. This isn’t about miracle cures or expensive supplements. It’s about understanding what’s actually harming your kidneys and fixing it before it’s too late.
The Real Culprits Behind Kidney Damage
It’s easy to blame genetics or bad luck, but the truth is, most kidney disease is tied to habits you can change. The biggest threats aren’t mysterious toxins or rare illnesses-they’re the same things that cause heart disease and diabetes: high blood pressure, high blood sugar, and obesity.
Diabetes is the #1 cause of kidney failure in the U.S., responsible for 4 out of every 10 cases. High blood sugar slowly damages the tiny filters in your kidneys, making them leak protein and lose function over time. Hypertension is close behind-it’s the second leading cause. When your blood pressure stays too high, it puts constant strain on the blood vessels in your kidneys, weakening them. Together, these two conditions account for 75% of all chronic kidney disease cases.
Then there’s obesity. Extra weight doesn’t just add pounds-it adds stress. Fat tissue releases chemicals that raise blood pressure and insulin resistance, pushing your kidneys into overdrive. Losing even 5 kilograms (about 11 pounds) can cut your risk of kidney disease by 25-30%.
And don’t forget smoking. Smokers are 50% more likely to see their kidney function decline over time. Smoking narrows blood vessels, reduces oxygen flow, and speeds up scarring in the kidneys. It’s not just about quitting for your lungs-it’s about saving your kidneys too.
What You Should Eat (and What to Avoid)
Your diet isn’t just about weight-it’s about protecting your kidneys from the inside out. The goal isn’t to follow a strict “kidney diet” unless you’re already in advanced stages. It’s about making smart, sustainable swaps.
Start with sodium. Most Americans eat over 3,400 mg of salt a day. The recommended limit? Under 2,300 mg. That’s about one teaspoon. But here’s the catch: 70% of that salt comes from packaged and restaurant food-not the salt shaker. Swap canned soups for low-sodium versions. Choose fresh or frozen veggies instead of canned. Rinse canned beans before using them. These small steps can drop your sodium intake by hundreds of milligrams per meal.
Next, cut back on sugar. Sugary drinks-soda, sweetened teas, energy drinks-are the biggest source of added sugar in the American diet. They contribute 7% of daily calories and spike blood sugar fast. One 12-ounce soda can have 39 grams of sugar. That’s more than the daily limit for women. Swap them for water, unsweetened tea, or sparkling water with lemon.
Protein is tricky. You need it, but too much-especially from red meat and processed meats-can overload your kidneys. Aim for lean sources: fish, chicken, beans, tofu. The sweet spot? Around 0.8 grams of protein per kilogram of body weight. For a 70 kg (154 lb) person, that’s about 56 grams a day. If you’re already at risk, talk to your doctor about adjusting this.
And don’t ignore fruits and vegetables. At least five portions a day isn’t just a guideline-it’s a shield. They’re rich in antioxidants, fiber, and potassium (which helps balance sodium). Think apples, berries, spinach, broccoli, carrots. They help lower blood pressure and reduce inflammation, both of which protect your kidneys.
Move More, Sit Less
Exercise isn’t optional if you want to protect your kidneys. You don’t need to run marathons. You just need to move consistently.
The CDC and NHS agree: 150 minutes of moderate activity each week is the minimum. That’s 30 minutes, five days a week. Brisk walking, cycling, swimming, dancing-anything that gets your heart rate up counts. Add strength training twice a week. Lifting weights or doing bodyweight exercises (squats, push-ups, lunges) helps control blood sugar and builds muscle, which improves insulin sensitivity.
And you don’t need a gym. Take the stairs. Park farther away. Walk after dinner. Dance while cooking. These small movements add up. Studies show people who stay active reduce their risk of developing diabetes and high blood pressure by up to 40%. And since those two conditions drive kidney disease, you’re killing two birds with one stone.
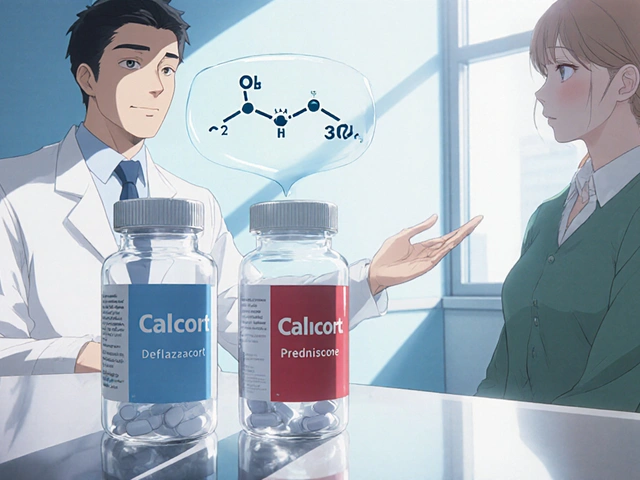
Medications and Supplements: What’s Safe?
Many people think painkillers are harmless. They’re not. Over-the-counter NSAIDs like ibuprofen and naproxen can damage your kidneys, especially if you take them regularly or have existing risk factors. These drugs reduce blood flow to the kidneys. In healthy people, that’s usually fine. In someone with high blood pressure or early kidney damage, it can accelerate decline.
The FDA estimates NSAIDs cause 3-5% of new kidney disease cases each year. If you need pain relief, talk to your doctor. Acetaminophen (Tylenol) is often safer for kidneys-but don’t overdo it either. Always check labels. Some cold and flu meds contain NSAIDs you might not expect.
And never ignore herbal supplements. Some, like licorice root or aristolochic acid (found in certain traditional remedies), are linked to kidney damage. Even “natural” doesn’t mean safe. Always tell your doctor what you’re taking-even if you think it’s harmless.
Check Your Numbers-Regularly
Kidney disease is silent. The only way to catch it early is through testing.
If you have diabetes, get your A1C checked at least twice a year. If you’re managing it well, your target should be under 7%. If you have high blood pressure, aim for 120/80 mm Hg or lower. If you’re overweight, lose weight. If you smoke, quit. These aren’t vague goals-they’re measurable targets that directly impact kidney health.
Ask your doctor for two simple tests: a urine albumin test (to check for protein in your urine) and a blood test for creatinine (used to calculate your GFR, or glomerular filtration rate). These tests are quick, cheap, and often covered by insurance. If you’re over 60, have diabetes, high blood pressure, or a family history of kidney disease, get screened yearly.
And here’s the hard truth: 90% of people with early kidney disease don’t know they have it. Don’t be one of them.

Stress, Sleep, and Your Kidneys
It’s easy to overlook stress and sleep, but they matter more than you think. Chronic stress raises cortisol and blood pressure. Poor sleep disrupts hormones that regulate fluid balance and blood sugar. Both can quietly damage your kidneys over time.
Studies from Johns Hopkins show that people who practice mindfulness, meditation, or deep breathing have 15% slower kidney function decline than those who don’t. You don’t need hours of yoga. Try 10 minutes of breathing exercises before bed. Or take a 15-minute walk without your phone.
And aim for 7-8 hours of sleep a night. Sleep apnea-often undiagnosed-is strongly linked to high blood pressure and kidney damage. If you snore loudly or wake up tired, talk to your doctor.
Who’s at Highest Risk?
Not everyone has the same risk. Black Americans are 3.4 times more likely to develop kidney failure than White Americans. Hispanic Americans are 1.3 times more likely. Why? Higher rates of diabetes and hypertension, plus unequal access to care and preventive services.
Family history matters too. If a close relative has kidney disease, your risk goes up-even if you’re healthy now. Age is another factor. Kidney function naturally declines after 60, so screening becomes even more critical.
And if you’ve had kidney stones, recurrent UTIs, or long-term use of certain medications, you’re not off the hook. These can leave lasting damage.
It’s Not Too Late to Start
Here’s the most important thing to remember: kidney disease isn’t a death sentence. And it’s not something you have to wait for. Every choice you make today-what you eat, how much you move, whether you check your blood pressure-adds up.
One study found that people who made just three lifestyle changes-eating healthier, exercising regularly, and quitting smoking-cut their risk of kidney disease by 50%. That’s not luck. That’s control.
You don’t need to fix everything at once. Start with one thing. Swap one soda for water. Take a 10-minute walk after dinner. Check your blood pressure next time you’re at the pharmacy. Small steps lead to big results.
And if you’re already living with diabetes or high blood pressure, know this: managing those conditions isn’t just about avoiding heart attacks or strokes. It’s about protecting your kidneys for the long haul. The same habits that help your heart help your kidneys too.
The cost of inaction? $128 billion a year in Medicare spending on kidney failure. The cost of action? A healthier life-and a chance to keep your kidneys working for decades to come.
Can kidney disease be reversed?
Early-stage kidney disease (Stages 1-2) can often be slowed or even stabilized with lifestyle changes. Once significant scarring occurs, the damage is usually permanent. But you can still prevent further decline. The key is catching it early through testing and acting fast.
How much water should I drink to protect my kidneys?
There’s no universal number. Most healthy people do fine with 6-8 glasses a day, but needs vary by body size, activity level, and climate. The best rule? Drink when you’re thirsty and check your urine color. Pale yellow means you’re hydrated. Dark yellow or amber means you need more fluids. Avoid forcing huge amounts-your kidneys will tell you what they need.
Is a low-protein diet necessary for everyone?
No. Only people with advanced kidney disease (Stage 4 or 5) typically need to limit protein. For most people, eating too much protein-especially from red meat-is the real issue. Stick to lean sources and keep portions moderate. Aim for about 0.8 grams per kilogram of body weight. If you’re unsure, talk to a dietitian.
Can I still drink alcohol if I want to prevent kidney disease?
Yes, but in moderation. One drink per day for women, two for men. Excessive alcohol raises blood pressure and contributes to liver damage, which indirectly harms the kidneys. It also dehydrates you. Stick to the limit, and avoid binge drinking.
What’s the best way to monitor kidney health at home?
You can’t test your kidney function at home, but you can track key risk factors. Use a blood pressure monitor (check it weekly). Track your weight and blood sugar if you have diabetes. Some smart scales estimate body fat and water weight, which can give clues about fluid balance. But the only way to know your kidney function is through a blood and urine test at your doctor’s office.







Comments (14)
kabir das
January 29, 2026 AT 07:39 AMI've been checking my BP every day since I read this... and I swear, my kidneys are whispering thanks. Seriously, though-why do we wait until we're falling apart to care? I'm 38, no diabetes, no obesity-but I swapped soda for sparkling water. One change. One tiny win. I feel like I'm finally listening to my body.
And yes-I quit ibuprofen like it was a toxic ex. No more 'just one' for headaches. My kidneys aren't a backup engine-they're the whole damn car.
DHARMAN CHELLANI
January 30, 2026 AT 03:36 AMLmao another 'eat veggies and walk' post. Kidney disease? More like corporate pharma’s way to sell dialysis machines. You think a banana’s gonna fix glomerulosclerosis? Nah. It’s epigenetics, toxins, and bad luck. And don’t even get me started on ‘low sodium’-salt is life. My grandpa ate 5 tsp a day and lived to 98. Your ‘science’ is weak.
Laura Arnal
January 30, 2026 AT 05:37 AMThis is SO important!! 🙌 I’m a nurse and I see people come in with Stage 4 CKD and ask ‘why me?’-and it’s always the same story: soda, no exercise, uncontrolled BP. But here’s the beautiful part: it’s NEVER too late to start! Even one walk a day? Huge. One less soda? Massive. You’re not fixing a broken kidney-you’re stopping the damage. And that’s POWERFUL. 💪❤️
Eli In
January 30, 2026 AT 13:48 PMI love how this post doesn’t just throw stats at you-it gives you real, doable steps. I’m from a culture where salt and fried food are love… but I started swapping out samosas for grilled chicken wraps. My mom thinks I’m crazy. But my last blood test? My creatinine dropped. 🌱 I’m not perfect, but I’m trying. And that’s enough.
Ryan Pagan
January 31, 2026 AT 19:10 PMLet’s cut through the fluff: this isn’t about ‘wellness’-it’s about survival. Your kidneys filter 200 quarts of blood daily. That’s a factory running 24/7. Now imagine feeding it diesel instead of premium gas. Sugar? Sodium? NSAIDs? Smoking? That’s not lifestyle-it’s sabotage. And yes, you can reverse early damage. Not because of some miracle herb-but because biology rewards consistency. Do the damn work.
Paul Adler
February 1, 2026 AT 19:33 PMA well-researched and calmly presented overview. I appreciate the emphasis on measurable outcomes-GFR, albuminuria, A1C-rather than vague wellness advice. The data on racial disparities is particularly critical and often under-discussed in public health messaging. For those with chronic conditions, adherence to monitoring protocols is not optional; it is foundational to longevity.
Robin Keith
February 3, 2026 AT 15:33 PMYou know... we’ve been lied to. The medical-industrial complex thrives on the illusion of control. You say ‘lifestyle changes’-but what if your kidneys are already screaming, and you’re just hearing static? What if the real enemy isn’t soda, but the systemic neglect of preventive care in marginalized communities? What if your ‘5-minute walk’ doesn’t matter when your neighborhood has no sidewalks, no clean water, and your job pays you to sit? I’m not denying your advice-I’m mourning the fact that it’s only accessible to those already privileged enough to have the time, space, and safety to follow it.
Sheryl Dhlamini
February 5, 2026 AT 04:36 AMI cried reading this. Not because I’m dramatic-but because I ignored my numbers for years. My dad died of kidney failure at 56. I’m 41. I just got my first urine test back-microalbumin was elevated. I didn’t panic. I didn’t blame myself. I just… started. Walked after dinner. Bought a salt shaker with a lid. Stopped drinking energy drinks. It’s not about being perfect. It’s about being present. And I’m here now.
Doug Gray
February 6, 2026 AT 13:26 PMInteresting framework. Though I’d argue the epistemic authority of ‘CDC/NHS guidelines’ is being overextended here. The correlation between sodium intake and renal decline is confounded by socioeconomic variables-processed food consumption, not salt per se, is the true variable. Also, hydration myths persist. The body is a homeostatic marvel. Don’t over-engineer it. Just… breathe. And maybe don’t take Advil every weekend.
Kristie Horst
February 7, 2026 AT 08:58 AMOh, so now we’re supposed to be grateful that the medical establishment has finally decided to warn us about the consequences of capitalism’s dietary industrial complex? How quaint. Let’s all just eat kale and pray to the FDA while our insurance denies us the specialist we need. 🙄
LOUIS YOUANES
February 8, 2026 AT 11:12 AMI don’t need a blog post to tell me my kidneys matter. I’ve been on dialysis for 3 years. This? This is for people who still think they have time. I’m not mad. Just tired. And honestly? I wish someone had told me this before I turned 30.
Andy Steenberge
February 10, 2026 AT 02:28 AMThis is one of the clearest, most actionable pieces I’ve read on kidney health. The breakdown of protein intake, the emphasis on urine testing, the distinction between early-stage reversibility and late-stage damage-it’s all precise. I’ve shared this with my entire family. My mom has hypertension, my brother is prediabetic. Knowledge isn’t power unless it’s passed on.
Laia Freeman
February 10, 2026 AT 04:26 AMI just started walking after work and I’m already feeling better!! 🙌 Also swapped my 3pm soda for lemon water and OMG I’m not crashing anymore!! I used to think kidney stuff was for old people but now I’m like… wait, I’m 29 and I’ve been poisoning myself for years 😭 I’m gonna do the urine test next week. Wish me luck!!
rajaneesh s rajan
February 11, 2026 AT 04:42 AMYou know what’s funny? We spend years chasing ‘purpose’ and ‘meaning’… but the most profound thing we can do is keep our kidneys working. They don’t care about your LinkedIn profile. They don’t care if you’re ‘productive.’ They just want you to stop eating chips and start walking. Simple. Brutal. True.