When a generic drug hits the market, you expect it to work just like the brand-name version. But how do regulators make sure it does? For simple pills, checking peak concentration (Cmax) and total exposure (AUC) was enough. But for complex drugs - especially extended-release painkillers, ADHD medications, or heart drugs - those old metrics often miss the real story. That’s where partial AUC comes in.
Why Traditional Bioequivalence Metrics Fall Short
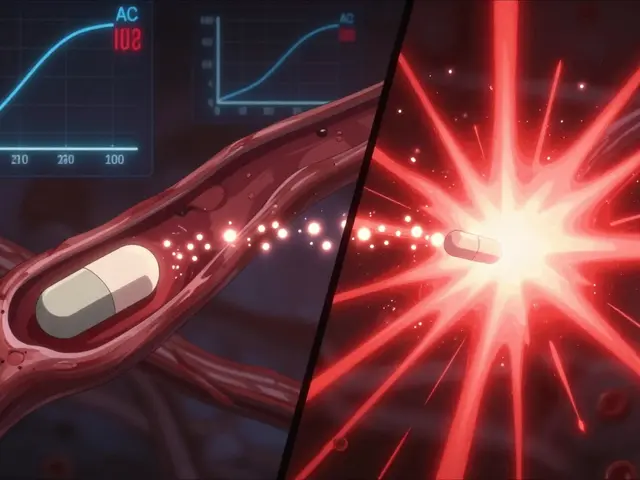
For decades, regulators judged generic drugs by two numbers: Cmax (the highest concentration in the blood) and total AUC (the full area under the concentration-time curve). These told you how much drug got into your system and how fast it peaked. But they didn’t tell you when it got there - or if the shape of the curve matched the original. Take an extended-release opioid. The brand version releases the drug slowly over 12 hours. A generic might hit the same total exposure (AUC) and peak (Cmax), but if it dumps 60% of the drug in the first two hours, it could cause dangerous spikes - or worse, be easier to abuse. Traditional metrics wouldn’t catch that. And that’s exactly what happened in real cases. In 2014, a study in the European Journal of Pharmaceutical Sciences found that 20% of generic products that passed traditional bioequivalence tests failed when partial AUC was applied. When both fasting and fed conditions were tested, that failure rate jumped to 40%. The drug looked fine on paper - but in the body, it behaved dangerously differently.What Is Partial AUC (pAUC)?
Partial AUC, or pAUC, measures drug exposure only during a specific window of time - not the whole curve. Think of it like zooming in on the most important part of a graph. For example, regulators might look only at the first 2 hours after dosing, where absorption happens. Or they might focus on the time when concentrations are above 50% of the peak. The key idea? Focus on the part of the curve that matters most for safety and effectiveness. If a drug needs to work fast - like a fast-acting insulin or a rescue inhaler - then early exposure is critical. If it’s meant to last all day - like a blood pressure pill - then sustained levels matter more. pAUC lets regulators check those specific parts, not just the overall picture. The U.S. FDA and the European Medicines Agency (EMA) started pushing for pAUC around 2013. The EMA first introduced it for prolonged-release formulations. The FDA followed, and by 2018, they were standardizing it across all drug types. Today, over 127 specific drug products require pAUC in their bioequivalence studies.How Is pAUC Calculated?
There’s no single way to define the time window. It depends on the drug. The FDA says the cutoff should be tied to a clinically relevant effect - not just convenience. Common methods include:- From time zero to the time when the reference product reaches its peak (Tmax)
- From zero to when drug concentration drops below 50% of Cmax
- From zero to a fixed time (like 2 or 4 hours) if that’s when the drug’s effect kicks in
Where Is pAUC Used Most?
pAUC isn’t needed for every drug. But it’s become standard for complex formulations:- Central nervous system drugs - like extended-release methylphenidate for ADHD - where early exposure affects focus and side effects
- Pain medications - especially opioids - where rapid release increases abuse risk
- Cardiovascular drugs - like verapamil or metoprolol - where steady levels prevent dangerous spikes or dips
- Abuse-deterrent formulations - any drug designed to resist crushing or dissolving must prove it releases slowly even under abuse conditions
Why Companies Struggle With pAUC
Even though pAUC is scientifically sound, it’s not easy to use. First, sample sizes often need to be bigger. Because pAUC measures a smaller part of the curve, variability increases. One company reported going from 36 to 50 subjects in a study - adding $350,000 to the cost. Another survey found 63% of generic developers needed extra statistical help for pAUC, compared to just 22% for regular AUC. Second, there’s no universal rule for the time window. The FDA’s product-specific guidances vary. Only 42% of them clearly say how to pick the cutoff time. That creates uncertainty. In 2022, 17 ANDA submissions were rejected because the pAUC time interval was poorly defined. Third, you need specialized software and expertise. Tools like Phoenix WinNonlin or NONMEM are required. Biostatisticians often need 3-6 months of training to get comfortable. And now, 87% of bioequivalence job postings list pAUC as a required skill.
Real Impact: Preventing Dangerous Generics
The value of pAUC isn’t theoretical. In 2021, a case study presented at the AAPS meeting showed a generic product that passed traditional AUC and Cmax tests had a 22% lower early exposure than the brand. That difference would’ve been invisible without pAUC. Had it been approved, patients might have gotten inadequate pain relief - or worse, experienced withdrawal symptoms. Another example: an abuse-deterrent opioid generic. The brand version released less than 15% of its dose in the first hour. The generic released 35%. Total AUC was fine. Cmax was fine. But pAUC caught the early spike - and the FDA blocked the approval. That’s exactly what pAUC was designed to do.The Future of pAUC
The FDA is working to make pAUC easier. In 2023, they launched a pilot program using machine learning to recommend time windows based on reference product data. They’re also expanding requirements - 41 new drugs were added to the list in early 2023, bringing the total to 127. By 2027, Evaluate Pharma predicts over half of all new generic approvals will need pAUC. That’s up from 35% in 2022. The big challenge? Global alignment. The EMA, FDA, and other agencies don’t always agree on time windows or methods. The IQ Consortium estimates this inconsistency adds 12-18 months to global drug development. But the science is clear: for complex drugs, traditional metrics aren’t enough. pAUC fills a critical gap. It doesn’t replace Cmax and AUC - it completes them.What This Means for Patients
You don’t need to understand the math. But you should know this: when a generic drug is approved with pAUC data, it means regulators looked deeper. They didn’t just check if the total dose was right. They checked if the drug behaved the same way in your body - from the first minute to the last. That’s not just science. It’s safety.What is partial AUC in bioequivalence?
Partial AUC (pAUC) measures drug exposure only during a specific time window - like the first 2 hours after dosing - rather than the entire concentration-time curve. It’s used to compare how quickly a generic drug absorbs compared to the brand, especially when early exposure affects safety or effectiveness.
Why is pAUC better than total AUC for some drugs?
Total AUC tells you the overall exposure, but not how the drug is released over time. For extended-release or abuse-deterrent drugs, the timing matters. A generic might have the same total AUC but release too much too fast - which could cause side effects or abuse. pAUC catches those differences by focusing on critical early or sustained phases.
Which regulatory agencies require pAUC?
Both the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) require pAUC for certain complex drug products, especially extended-release formulations, abuse-deterrent opioids, and CNS medications. The FDA has mandated pAUC in over 127 product-specific guidances as of 2025.
How do you choose the time window for pAUC?
The time window should be tied to a clinically relevant effect - not just convenience. Common methods include using the reference product’s Tmax, setting a cutoff at 50% of Cmax, or choosing a fixed time (e.g., 0-2 hours) based on when the drug’s effect starts. The FDA recommends linking the window to pharmacodynamic data whenever possible.
Is pAUC required for all generic drugs?
No. pAUC is only required for complex formulations where traditional metrics (Cmax and total AUC) can’t reliably ensure therapeutic equivalence. This includes extended-release, abuse-deterrent, and certain CNS or cardiovascular drugs. Most simple immediate-release generics still use only Cmax and AUC.
What are the biggest challenges in using pAUC?
The main challenges are higher variability (requiring larger study sizes), inconsistent guidance across products, lack of standardized time windows, and the need for specialized statistical expertise. Many companies now hire external consultants or use advanced software like WinNonlin to handle pAUC analysis correctly.








Comments (10)
Adrienne Dagg
December 18, 2025 AT 21:16 PMI had no idea this was even a thing 😳 My dad’s generic pain meds used to make him feel weirdly wired at first then crash hard. Now I get why. pAUC is literally saving lives.
Monte Pareek
December 18, 2025 AT 21:31 PMLook i get that regulators want to be thorough but the cost of this is insane and its not even consistent across countries and honestly if you think a 50 subject study is expensive wait till you try to get a bioequivalence study done in europe vs usa vs canada the time windows change like the weather and half the time the guidance documents are written by people whove never touched a blood sample in their life so yeah i get that pAUC is scientifically sound but the system is broken and generic companies are getting crushed and patients are paying for it in delayed access and higher prices and dont even get me started on how long it takes to get a new generic approved now its like a bureaucratic nightmare
Elaine Douglass
December 19, 2025 AT 18:04 PMThis is actually really interesting i never thought about how a pill releases over time like this. My cousin takes ADHD meds and she always said the generic made her feel off in the morning. Now it makes sense. Glad someone’s paying attention to the details
Alex Curran
December 20, 2025 AT 05:19 AMFascinating stuff. In Australia we’ve been using pAUC for CNS drugs since 2016 but the lack of standardization still bites us. One product’s window is 0-2h another is 0-Tmax another is 50% Cmax. It’s chaos. Pharma needs to stop treating this like a math puzzle and start treating it like a clinical reality
Nicole Rutherford
December 21, 2025 AT 01:51 AMOf course they’re making this harder. Big Pharma just wants to keep generics out so they can keep charging $500 for a 30-day supply of something that costs $2 to make. This pAUC nonsense is just a backdoor monopoly. They don’t care about safety they care about profit.
Mark Able
December 21, 2025 AT 12:59 PMWait so if a generic passes Cmax and AUC but fails pAUC does that mean it’s dangerous or just not identical? Like can I still take it or should I panic? Someone explain this like i’m 5
Dorine Anthony
December 21, 2025 AT 19:23 PMI’m just glad someone’s finally looking at the full picture. I’ve been on extended-release metoprolol for years and the generic I got last year made me dizzy for a week. Turns out the early spike was off. Took me months to figure out it was the med. Glad they’re fixing this.
William Storrs
December 22, 2025 AT 09:24 AMYou know what’s amazing? This isn’t just about math. It’s about people. Every time pAUC blocks a bad generic it’s saving someone from a bad reaction or a relapse or a withdrawal. This is science doing its job. Keep pushing for it. The system’s messy but you’re making a difference.
James Stearns
December 22, 2025 AT 17:14 PMThe application of partial area under the concentration-time curve constitutes a statistically rigorous and pharmacodynamically informed paradigm shift in the evaluation of bioequivalence for complex pharmaceutical formulations. One must acknowledge that the regulatory framework, while imperfect, is evolving in accordance with the preeminent principles of evidence-based therapeutics and patient-centric safety.
Janelle Moore
December 23, 2025 AT 19:00 PMThey’re hiding something. pAUC is just a cover. The real reason they’re making this so hard is because they’re testing for mind control chemicals. You think they care about your heart? They’re watching your brainwaves through the blood samples. I read it on a forum. 7 out of 10 scientists are in on it.