Why cleanroom standards matter more than you think for generic drugs
Generic drugs are supposed to be exact copies of brand-name medicines. But if they’re made in a dirty room, they’re not copies-they’re risks. Cleanroom standards aren’t just paperwork. They’re the line between a safe, effective pill and a dangerous batch that could sicken or kill someone. For generic manufacturers, these standards aren’t optional. They’re the only way to prove their product works just like the original. The FDA and other global regulators don’t just ask for cleanrooms-they demand them. And failing means recalls, fines, or worse.
What exactly is a pharmaceutical cleanroom?
A pharmaceutical cleanroom is a controlled environment built to keep out dust, microbes, and other contaminants. It’s not just a clean lab. It’s engineered with special air filters, pressure systems, and strict rules for who can enter and how they dress. Think of it like an operating room, but for making pills, injections, and eye drops.
These rooms are ranked by how clean they are. The highest level, Grade A (also called ISO Class 5), lets in no more than 3,520 tiny particles per cubic meter-smaller than a human hair. That’s stricter than a hospital operating room. Lower grades, like Grade C and D, allow more particles but still far less than a normal office. Each grade has exact rules for airflow, temperature, humidity, and how often air is replaced.
Every cleanroom uses HEPA filters that trap 99.95% of particles 0.3 micrometers or larger. Air flows in one direction-like a slow, steady river-to push contaminants out. Temperature stays between 18°C and 26°C. Humidity is kept between 30% and 60%. Too dry, and static electricity pulls dust onto products. Too wet, and mold grows.
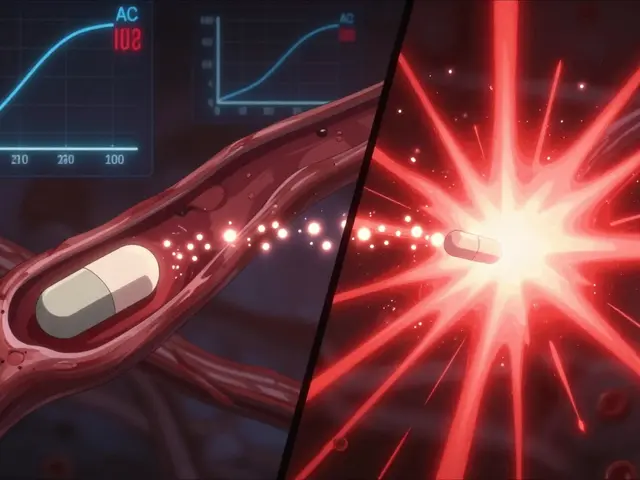
How cleanroom grades work in real manufacturing
Not every drug needs the same level of cleanliness. It depends on how the drug is made and how it’s used.
- Grade A: Used for filling sterile injectables-like insulin, chemotherapy, or IV antibiotics. This is where the drug touches the final container. One particle here could mean infection. Airflow is laminar, meaning it moves in straight lines at 0.36-0.54 meters per second. Every second counts.
- Grade B: The background area around Grade A. Think of it as the prep zone. Workers gown up here before entering the sterile area. At rest, it’s as clean as Grade A. During operations, it’s allowed to be a bit dirtier, but still tightly controlled.
- Grade C: For making non-sterile tablets or capsules that are still sensitive, like eye drops or some oral suspensions. Air changes happen at least 20 times per hour. This is common in generic drug plants producing pills that don’t go into the bloodstream directly.
- Grade D: The lowest level, used for packaging or storing finished products. It’s still cleaner than a regular warehouse, but doesn’t need the same level of control. Many generic manufacturers try to keep this as their baseline to save money.
The EU’s Annex 1 (updated in 2023) and the FDA’s cGMP rules both require these grades. But here’s the catch: the FDA doesn’t always say “ISO Class 5.” It just says “prevent contamination.” The EU spells it out. That’s why many U.S. generic makers follow EU standards-they’re clearer, and easier to prove during inspections.

Why generic drug makers struggle with cleanrooms
Brand-name drug companies charge $10,000 a dose. Generic makers sell the same pill for $0.50. That’s the problem. Cleaning a room to Grade A standards costs $250-$500 per square foot. A 1,000-square-foot cleanroom? That’s $500,000 before you even buy equipment.
And it doesn’t stop there. You need:
- Continuous air monitoring systems ($50,000-$100,000 per room)
- 24/7 temperature and humidity logs
- Staff trained for 40-60 hours just to gown properly
- Documentation for every single air sample, every person who entered, every filter change
One generic manufacturer in Ohio told ISPE they spent $2.3 million upgrading a cleanroom to Grade B for a cancer drug. The payoff? They stopped having 17 out-of-spec batches a year-each worth $500,000. That’s $8.5 million saved annually.
But not everyone can afford that. A small company making generic heparin syringes-worth half a cent each-couldn’t cover the cost of keeping Grade A clean. After two FDA inspections flagged tiny particle spikes, they shut down. That’s the reality: cleanroom costs are squeezing out smaller generic makers.
What happens when cleanrooms fail
In 2012, a compounding pharmacy in Massachusetts didn’t meet basic cleanroom standards. Their steroid injections were contaminated with fungus. Over 750 people got meningitis. 64 died.
That’s why the FDA now watches generic drug cleanrooms like a hawk. In 2022, 63% of all FDA warning letters were about GMP violations-most of them tied to cleanroom failures. One major case: Aurobindo Pharma in 2022. Their Grade B cleanroom had inconsistent air pressure and unmonitored microbial growth. The result? A $137 million recall of sterile injectables. The company had to pay millions in fines and stop shipping for months.
It’s not just about money. It’s about trust. When a generic drug fails, patients lose faith in all generics. That hurts everyone.
How the rules are changing-and what it means
The EU’s 2023 Annex 1 update made things tougher. Now, cleanrooms need real-time particle monitoring, not just spot checks. You can’t just sample air once a day-you have to track it constantly. The FDA says it’s coming soon.
Also, new drugs are harder to make. Biosimilars, inhalers, and complex injectables need tighter controls than ever. The FDA predicts that by 2025, half of all generic drug applications will need Grade A or B environments. That’s up from 35% in 2022.
Some experts argue the standards are too strict for pills. One 2020 study showed oral solids made in Grade D rooms performed just as well as those made in Grade C. But regulators say: “Better safe than sorry.” Especially when a drug is taken by someone with a weak immune system.
How manufacturers are adapting
Big players like Teva are winning by investing smartly. For their generic version of Copaxone, they installed isolator systems-sealed, robotic workstations inside Grade A rooms. Contamination events dropped from 12 per year to just 2. That’s how you get FDA approval after being rejected twice.
Smaller companies are turning to automation. Robots don’t shed skin cells. They don’t sneeze. They don’t forget to gown. AI-powered monitoring systems now predict contamination before it happens. McKinsey projects that by 2028, automation will cut cleanroom operating costs by 25-30%.
Training is also improving. Instead of just reading manuals, staff now train in virtual reality simulations of gowning procedures. One study found this cut human errors by 40%.
What you need to know if you’re buying generic drugs
You don’t need to know the ISO class of the cleanroom where your pill was made. But you should know this: if your generic drug works the same as the brand name, it’s because someone spent millions to make sure it was safe. The FDA doesn’t approve generics based on price. They approve them based on proof-proof that every batch meets the same standards as the original.
That’s why the cheapest generic isn’t always the best. If a company cuts corners on cleanrooms, they might save money now-but they risk your health later.
Resources to learn more
If you work in pharmaceutical manufacturing, here’s where to start:
- FDA’s free cGMP training modules
- ISPE’s Good Practice Guide: HVAC
- Parenteral Drug Association Technical Reports 14, 22, and 45
- EU GMP Annex 1 (2023 version)
- ISO 14644-1:2015 (Cleanroom classification)
These aren’t just guidelines. They’re the rules that keep millions of people safe every day.





Comments (13)
Kevin Wagner
November 14, 2025 AT 00:26 AMThis is the kind of stuff nobody talks about but should be screamed from the rooftops. You think your $2 generic pill is just a cheap copy? Nah. It’s a miracle of engineering, sanitation, and human discipline. Someone in a sterile suit, under 20 air changes per hour, just made sure your asthma inhaler won’t kill you. That’s not luck. That’s sacrifice.
gent wood
November 14, 2025 AT 17:15 PMThe level of precision required here is staggering. HEPA filters, laminar airflow, gowning protocols that take hours to master-this isn’t just manufacturing; it’s a controlled environment bordering on surgical. And yet, the public treats generics like discount groceries. The disconnect between cost perception and quality control is terrifying.
Dilip Patel
November 16, 2025 AT 17:04 PMUSA and EU think they own cleanroom rules but India makes 40% of the world’s generics and we do it better. Our labs are clean, our workers trained, our costs low. You think your $0.50 pill is unsafe? Try buying it from a country that cant even spell GMP. We dont need your overpriced ISO standards to make safe medicine. We have discipline.
Jane Johnson
November 18, 2025 AT 16:25 PMI find it deeply concerning that regulatory agencies allow such variance in enforcement. The FDA’s vague language regarding contamination prevention creates dangerous ambiguity. If a facility operates at Grade D for oral solids, and that is deemed acceptable, then the entire framework of pharmaceutical safety is built on subjective interpretation rather than objective science.
Peter Aultman
November 20, 2025 AT 14:38 PMHonestly i didnt realize how insane the cleanroom game was until i read this. Its like making a burger in a nuclear lab. Robots, air rivers, 24/7 logging. Wild. And yet we still get pills that work. Thats the real miracle. Not the brand name. Not the price. The system.
Sean Hwang
November 20, 2025 AT 14:53 PMSmall companies are getting crushed. I know a guy who ran a generic pill shop in Ohio. He upgraded to Grade B for a cancer med. Spent 2.3 mil. Got slapped with a warning letter anyway because a filter wasn’t changed on time. They’re not evil. They’re just outgunned. The system’s rigged for big pharma.
Barry Sanders
November 21, 2025 AT 18:12 PMLet’s be real: 63% of FDA warning letters are cleanroom violations. That’s not a coincidence. That’s a systemic failure. These companies aren’t failing because they’re incompetent-they’re failing because they’re trying to make pennies on pills that cost half a million to produce. This isn’t regulation. It’s economic genocide.
Chris Ashley
November 23, 2025 AT 06:21 AMWait so you’re telling me my $0.10 generic ibuprofen was made in a room that costs half a million to run? And I’m supposed to feel safe? Bro I bought it at a gas station. I’m just glad it didn’t explode.
kshitij pandey
November 23, 2025 AT 18:39 PMIn India, we teach our workers that medicine is sacred. Even if the room is Grade D, the heart is Grade A. We don’t need fancy robots to care. We need pride. And we have it. Every pill we make carries the weight of a family’s hope. That’s the real standard.
Eleanora Keene
November 25, 2025 AT 18:05 PMI’m so proud of the people who work in these rooms. The quiet ones. The ones who gown up for 45 minutes just to press a button. No applause. No raises. Just the knowledge that their work keeps someone alive. That’s the quiet heroism we ignore until someone dies.
Joe Goodrow
November 26, 2025 AT 14:53 PMAmerica used to make this stuff. Now we outsource to countries that can’t even spell ‘HEPA’ and then wonder why our kids get sick. This isn’t about cost. It’s about national security. Your medicine should be made by Americans. Period.
Brittany C
November 27, 2025 AT 11:37 AMThe EU Annex 1 update is a game-changer. Real-time particle monitoring, dynamic airflow validation, microbial trend analysis-these aren’t luxuries. They’re the baseline for patient safety. The FDA’s lagging behind because they’re still operating in a 1990s mindset. The science has moved on. So must we.
Sean Evans
November 28, 2025 AT 23:17 PMI’ve seen the data. 75% of cleanroom failures are caused by human error. Not equipment. Not design. PEOPLE. So why are we spending millions on robots and filters when we should be firing every employee who forgets to wash their hands? This isn’t science. It’s a circus. And we’re all paying for the tickets.