Accidental overdose isn’t always a mistake-it’s often a pattern. Someone takes a pill they forgot they already took. They mix painkillers with alcohol because they didn’t write down what they took yesterday. They increase their dose because they feel like it’s not working, but they can’t remember what they took last week. These aren’t rare cases. They happen every day, and they’re preventable with one simple tool: a medication log.
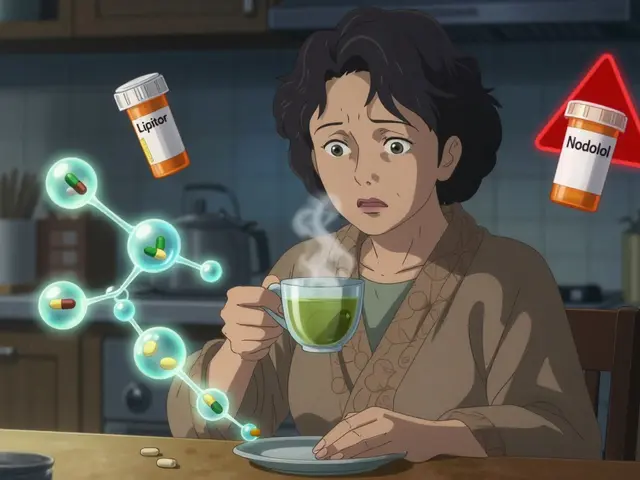
A medication log isn’t just for people on opioids. It works for anyone taking multiple prescriptions, over-the-counter drugs, supplements, or even recreational substances. The goal isn’t to judge your choices-it’s to give you clear, real-time data so you don’t accidentally take too much, too often, or the wrong mix.
What a Medication Log Actually Does
Think of your medication log as a personal Prescription Drug Monitoring Program (PDMP). PDMPs are state-run systems that doctors use to see what controlled substances you’ve been prescribed across all pharmacies. But those systems have delays-they only update when a prescription is filled, not when you actually take it. Your log fills that gap. It shows what you did, not just what you were supposed to take.
Here’s what happens when you skip logging:
- You take 10 mg of oxycodone at 8 a.m. because your back hurts.
- By 3 p.m., the pain is back. You don’t remember taking it earlier, so you take another 10 mg.
- At 8 p.m., you have a drink to relax. You don’t realize you’ve now taken 20 mg of opioids plus alcohol-two substances that can shut down your breathing when combined.
That’s not a one-time mistake. It’s a repeatable risk. A log stops that cycle.
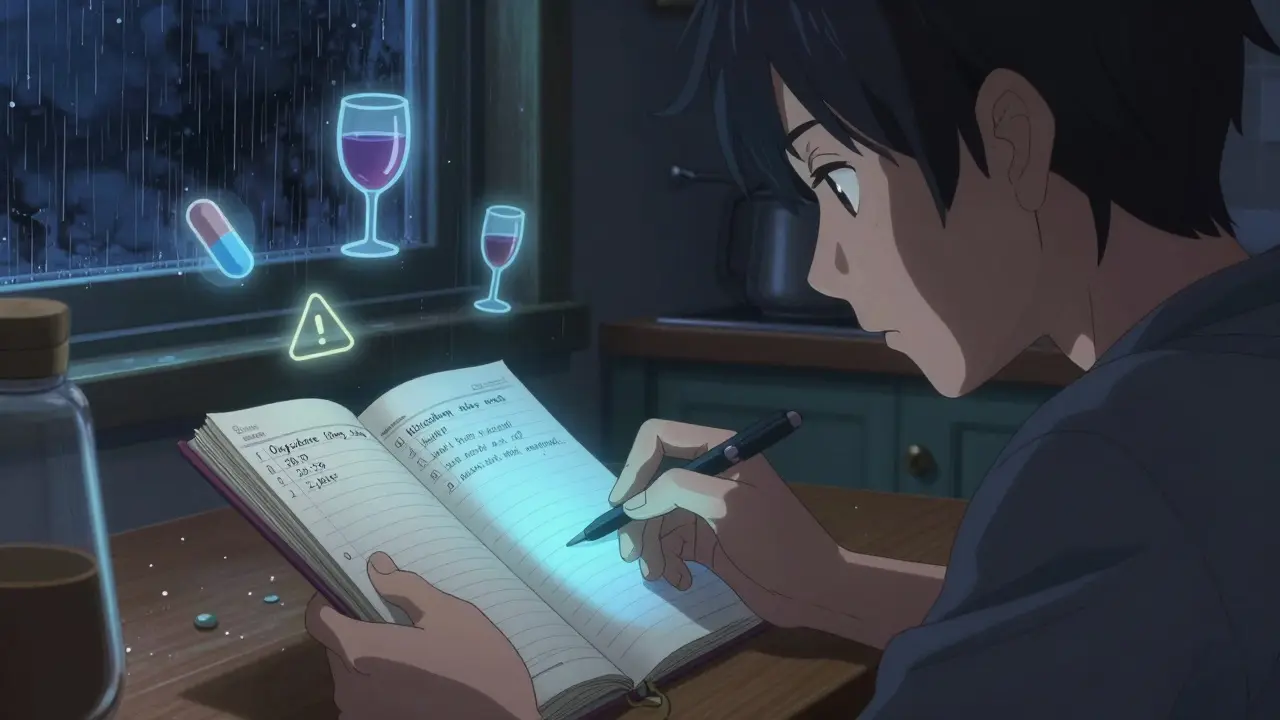
What to Write in Your Log (The 5 Essentials)
You don’t need a fancy app. A notebook, a notes app, or even a printed template works. But every entry needs these five things:
- Medication name - Write the full name. Not “pain pill.” Not “Oxy.” Write oxycodone 10 mg or acetaminophen 500 mg.
- Dosage amount - Exact number of milligrams or milliliters. If you took half a pill, write “5 mg.” If you used a liquid, write “10 mL.”
- Time taken - Use 24-hour time if you can (14:30 instead of 2:30 p.m.). This helps you spot patterns like “I always take it right before bed.”
- Method of use - Swallowed? Snorted? Injected? Smoked? This matters. SAMHSA’s guidelines say your overdose risk jumps when you change how you take a drug. A log makes this visible.
- Other substances taken - Alcohol? Xanax? Sleep aids? Caffeine? Even herbal teas. Combine opioids with depressants? That’s a red flag. Your log needs to show the full picture.
Optional but powerful: add a short note on how you felt. “Dizzy after 20 minutes.” “No pain relief.” “Nauseous.” This helps you spot side effects early and know when to stop.
How to Start-Simple Steps
You don’t need to be perfect. Start today with what you have.
- Grab a notebook or open Notes - Pick one place and stick with it. No more than two formats.
- Log your next dose - Even if you’re not on opioids. Just write: “10 mg hydrocodone, 11:15, swallowed, no other meds.”
- Set a daily reminder - Use your phone. “Log meds” at 8 p.m. every night. If you forget one day, just start again tomorrow. No guilt.
- Review weekly - Every Sunday, look back. Did you take more than prescribed? Did you mix substances? Did you feel worse after certain times? That’s your data.
That’s it. No complicated system. Just consistent, honest tracking.
Why This Works Better Than Just Relying on Memory
Memory is unreliable. Especially under stress, pain, fatigue, or when substances are involved. Studies show people misremember their dosing by 30-50% within 24 hours. That’s not a flaw in character-it’s how the brain works.
Here’s what a log gives you that memory never can:
- Proof of what you actually took - not what you think you took.
- Patterns you didn’t notice - like taking extra doses on weekends.
- Early warning signs - nausea, dizziness, confusion after certain combinations.
- A way to talk to your doctor - not with “I think I took…” but with clear records.
One person I spoke with (who chose to stay anonymous) started logging after nearly overdosing. “I didn’t realize I’d taken two doses of gabapentin that day. I thought I’d only taken one. The log showed me I was mixing it with alcohol every night. I cut that out. I haven’t had a scare since.”
What to Avoid
Not all logs are helpful. Here’s what to skip:
- Estimating doses - “About 10 mg” isn’t enough. Use the label. If you don’t know the dose, don’t take it until you check.
- Using vague names - “Pill” or “Red one” means nothing. Write the full name.
- Skipping entries - If you miss a day, don’t try to backfill. Just start fresh. Consistency beats perfection.
- Keeping it secret - If you have someone you trust, show them your log. A friend, family member, or peer recovery coach can help spot risks you miss.

Tools That Help
You don’t need tech. But if you like apps, here are simple, free options:
- Medisafe - Sends reminders and lets you log doses, side effects, and other substances.
- MyTherapy - Tracks medications, supplements, and mood. Good for spotting patterns.
- Google Keep or Apple Notes - Just create a daily list. Add a timestamp. Done.
Some harm reduction groups now offer printable log templates with space for test strip results. If you use fentanyl or xylazine test strips, write down the result. “Negative for fentanyl” or “Positive for xylazine” is critical info.
When to Ask for Help
Your log isn’t just for you. It’s a tool to protect your life. If you notice:
- Needing more than prescribed to feel the same effect
- Taking drugs to avoid withdrawal, not for pain
- Using alone more often
- Blacking out after taking medication
- those are signs you need more than a log. Talk to a doctor, counselor, or harm reduction worker. You don’t have to do this alone. Resources like SAMHSA’s National Helpline (1-800-662-4357) are free and confidential.
Final Thought: This Isn’t About Control. It’s About Safety.
You’re not trying to be perfect. You’re trying to stay alive. A medication log doesn’t judge your choices. It just gives you the facts. And with facts, you can make smarter decisions. One entry at a time.
Do I need a special app to keep a medication log?
No. A paper notebook, a notepad app, or even a sticky note on your fridge works. The key isn’t the tool-it’s consistency. Write down the name, dose, time, method, and other substances every time you take something. Apps can help with reminders, but they’re not required.
What if I forget to log a dose?
Don’t panic. Don’t try to guess and backfill. Just start again with your next dose. Forgetting happens. What matters is that you keep going. Even logging 80% of your doses is better than nothing. Over time, it becomes a habit.
Can a medication log really prevent an overdose?
Yes-when used correctly. It doesn’t stop every overdose, but it removes one of the biggest causes: accidental double-dosing or dangerous combinations. CDC data shows that people who track their medication use are significantly less likely to take unsafe doses. It’s not magic, but it’s one of the most effective low-cost tools available.
Should I share my medication log with others?
If you feel safe doing so, yes. Sharing your log with a trusted friend, partner, or peer support person can be lifesaving. If you’re using alone and something feels off, they can check your log and know what you took. Many harm reduction programs encourage this as part of safety planning.
What if I’m not on opioids? Do I still need a log?
Yes. Overdose isn’t just about opioids. Mixing benzodiazepines with alcohol, taking too much acetaminophen, or combining supplements with prescription drugs can all lead to serious harm. Anyone taking more than one medication regularly benefits from tracking what they take and when.
How often should I review my log?
Once a week is enough. Look for patterns: Are you taking more on weekends? Do you always feel dizzy after 3 p.m.? Are you mixing substances you didn’t realize were risky? Weekly reviews help you catch problems before they become emergencies.
If you’re using medication regularly, your log is your safest companion. Start today. One entry. One moment of clarity. That’s how you stop an overdose before it starts.







Comments (15)
THANGAVEL PARASAKTHI
February 7, 2026 AT 22:46 PMI started logging my meds after almost passing out from mixing gabapentin and wine. Didn't think it was a big deal till my log showed I did it 3 nights straight. Now I just write it in my phone notes. '1000mg gab, 9:30, swall, 2 glasses wine.' Simple. Works. No app needed.
Frank Baumann
February 9, 2026 AT 21:36 PMLet me tell you something - this isn't just about avoiding overdose, this is about reclaiming your autonomy in a world that wants you to be numb, compliant, and forgetful. You think you're just writing down pills? No. You're building a monument to your own survival. Every entry is a middle finger to the system that told you to just 'take what the doctor says' while they got rich off your dependency. This log? It's your rebellion. It's your proof that you're still in charge - even when your body screams for more. Don't underestimate this. This is life-or-death philosophy in 5 bullet points.
Scott Conner
February 10, 2026 AT 23:37 PMI'm curious - does anyone track their water intake too? Like, if you're on opioids or benzos, dehydration can make side effects way worse. I started writing 'water: 2L' next to my med logs and noticed I stopped getting dizzy by 4 p.m. Maybe it's placebo, maybe not. But it's free and easy.
Susan Kwan
February 11, 2026 AT 22:19 PMOh great. Another 'just write it down' solution for people who can't afford therapy. Meanwhile, my cousin overdosed last week because she was taking 3 different meds and her 'log' was scribbled on a napkin while she was high. This isn't a fix. It's a Band-Aid on a hemorrhage.
Random Guy
February 12, 2026 AT 08:06 AMI tried logging. Lasted 3 days. Then I realized I was logging my meds… while high. So I wrote: 'took 20mg oxycodone. Felt like god. Also ate 3 tacos. No other meds.' Then I passed out. My log is now a work of art. And I still didn't overdose. So… point?
Tasha Lake
February 13, 2026 AT 07:30 AMThe 5 essentials are spot on - especially method of use. I didn’t realize snorting my hydrocodone was increasing my respiratory depression risk by 40% per SAMHSA’s 2021 guidelines. Once I started logging 'oral' instead of 'snort,' I caught myself doing it subconsciously. Behavioral awareness > willpower. This is harm reduction 101.
Brett Pouser
February 13, 2026 AT 16:42 PMI’m from rural Texas. We don’t have easy access to doctors or apps. I use a notepad taped to my fridge. My mom writes in it too - she’s on blood pressure meds and diabetes pills. We check it together every Sunday. It’s not fancy. But it’s ours. And we’re still here. That’s what matters.
Karianne Jackson
February 15, 2026 AT 11:54 AMI used to think this was for addicts. Then I started taking 4 different vitamins and a sleep aid and forgot I took them. Woke up with a headache and nausea. Now I write: 'Vit D, 800, 7pm.' Done. No drama. Just don't forget.
Andy Cortez
February 16, 2026 AT 05:22 AMThis whole thing is a scam. You think writing down your pills stops overdoses? Nah. It just makes you feel better while you keep doing the same dumb shit. The real problem? Pharma companies pushing drugs. The government letting them. And now we’re supposed to babysit ourselves with sticky notes? Give me a break.
Jacob den Hollander
February 18, 2026 AT 04:36 AMI’m so glad someone wrote this. My brother was almost gone last year - he didn’t know he was mixing tramadol with melatonin. He thought melatonin was 'safe.' We started logging together. Now he sends me a pic every night. I don’t judge. I just say 'good job.' It’s not about control. It’s about showing up - for yourself, and for someone who loves you.
John Sonnenberg
February 18, 2026 AT 16:53 PMI've been using a physical log since 2018. I use a spiral notebook. I write in pen. I date every entry. I never erase. If I miss a day? I write 'Missed: 4/12' and move on. No guilt. No shame. Just truth. My doctor says my log is the clearest she's ever seen. It's not about perfection. It's about persistence.
Kathryn Lenn
February 19, 2026 AT 16:53 PMSo... this is just government propaganda disguised as self-help, right? 'Log your meds' - sure. But what if the log gets hacked? What if insurance companies use it to deny coverage? What if they start requiring logs just to prescribe anything? This feels like a backdoor to surveillance. Don't be fooled.
John Watts
February 20, 2026 AT 18:09 PMI used to think I was too busy for this. Then I got hospitalized for liver damage from too much Tylenol. Now I log everything - even ibuprofen. I set a daily alarm. It takes 15 seconds. I don’t even think about it anymore. It’s just part of my routine. Like brushing my teeth. And I’m alive. That’s the win.
Chima Ifeanyi
February 22, 2026 AT 10:30 AMIn Nigeria, we don’t have apps. We have WhatsApp groups. My aunt and I have a group called 'Med Log Squad.' We send voice notes: 'Took 5mg oxycodone, 10:30, oral, no alcohol.' She replies with 'Good. Drink water.' It’s not perfect. But it’s ours. And we’re not dead yet.
Angie Datuin
February 23, 2026 AT 22:27 PMI started logging because I was scared to talk to my doctor. Now I show them my log every visit. They say it’s the most helpful thing they’ve seen in months. I didn’t know I was taking extra doses on weekends. I thought I was being careful. Turns out, I was just forgetful. This log saved me from myself.