Heart Medication Interaction Checker
Select all medications you're currently taking. This tool identifies dangerous combinations based on medical research. Always consult your doctor or pharmacist before making changes to your medications.
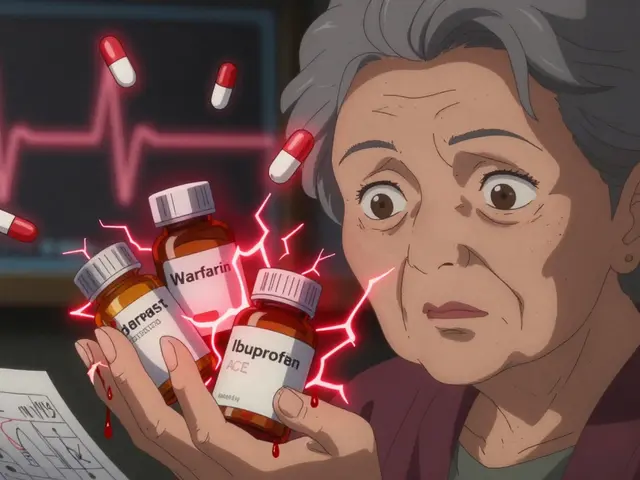
Every year, over 106,000 people in the U.S. die from adverse drug reactions-many of them preventable. For people taking heart medications, the risk isn’t just theoretical. It’s real, urgent, and often hidden in plain sight. You might be taking a blood pressure pill, a cholesterol drug, and an over-the-counter pain reliever without realizing you’re putting your heart at risk. The truth is, some combinations don’t just reduce effectiveness-they can trigger heart attacks, strokes, or sudden death.
Why Heart Medications Are Especially Risky
Heart medications are designed to control critical functions: blood pressure, heart rhythm, clotting, and fluid balance. That’s why even small changes in how they interact can throw your body off balance. A study published in Pharmacoepidemiology & Drug Safety in 2023 found that older adults taking just two or more cardiovascular drugs with known risks had their chance of heart attack, stroke, or death doubled or even tripled. The risk didn’t come from one drug alone-it came from the mix.Over 44% of men and 57% of women over 65 take five or more prescriptions weekly. Many of these are heart-related: beta blockers, ACE inhibitors, diuretics, statins, and anticoagulants. But what happens when you add something else? A painkiller. A supplement. Even alcohol. That’s where things go wrong.
The 7 Most Dangerous Combinations
Not all drug interactions are created equal. Some are rare. Others are common-and deadly. Based on clinical data from MedicineNet, PALTmed, and the USC Schaeffer Center, here are the seven most dangerous combinations you need to avoid:- Warfarin and ibuprofen: Warfarin thins your blood. Ibuprofen irritates your stomach lining. Together, they raise your risk of gastrointestinal bleeding by 300%. One study found that patients on this combo had INR levels spike unpredictably, leading to emergency hospitalizations after minor injuries or dental work.
- Warfarin and acetaminophen: You might think Tylenol is safe. But with chronic use, it can raise your INR by 2 to 3 points-enough to turn a manageable dose into a dangerous one. This interaction is sneaky because it builds slowly, often going unnoticed until bleeding starts.
- PDE-5 inhibitors (like Viagra) and nitrates: This combo can drop your systolic blood pressure below 70 mmHg. That’s not just dizziness-it’s shock. Nitrates are used for chest pain. PDE-5 inhibitors are for erectile dysfunction. Both relax blood vessels. Together, they can cause a sudden, life-threatening crash in blood pressure.
- Statins and amiodarone: Amiodarone is a powerful heart rhythm drug. Statins lower cholesterol. But when combined, they increase the risk of severe muscle damage (rhabdomyolysis) by 400-500%. This can lead to kidney failure. Patients on this combo often report unexplained muscle pain or dark urine-signs you can’t ignore.
- ACE inhibitors and potassium supplements: ACE inhibitors help your heart by relaxing blood vessels. But they also cause your body to hold onto potassium. Add a potassium pill or salt substitute, and your levels can climb past 5.5 mEq/L. That’s dangerous territory. At that level, your heart can stop beating. One study showed 18.7% of patients on this combo developed hyperkalemia, compared to just 4.2% of those not taking both.
- Digoxin and verapamil: Digoxin helps the heart pump stronger. Verapamil slows your heart rate. Together, they cause digoxin levels to jump 60-75%. This leads to nausea, confusion, irregular heartbeat, and even cardiac arrest. Many patients don’t realize verapamil is a calcium channel blocker-it’s often prescribed for high blood pressure or chest pain.
- NSAIDs (ibuprofen, naproxen, diclofenac) and blood pressure meds: NSAIDs don’t just hurt your stomach-they hurt your heart. They reduce the effectiveness of diuretics by 25-30%, cause fluid retention, and raise blood pressure. For someone with heart failure, this can mean hospitalization. A 2023 study found that 28% of patients on blood pressure meds who took NSAIDs had acute kidney injury or worsening heart failure.
What You Might Not Realize Is Dangerous
It’s not just prescription drugs. Supplements and over-the-counter products are major players in dangerous combinations.St. John’s wort, turmeric, and garlic supplements can interfere with warfarin, making it either too strong or too weak. One patient reported an INR of 8.0 after taking St. John’s wort with warfarin-far above the safe range of 2.0-3.0. That’s a major bleeding risk.
Even something as simple as a cold medicine can be risky. Many contain pseudoephedrine or phenylephrine, which raise blood pressure. If you’re on beta blockers or ACE inhibitors, that’s a problem. And alcohol? Mixing it with opioids, benzodiazepines, or even some blood pressure meds can slow your breathing to dangerous levels.
What About Beneficial Combinations?
Not all combinations are bad. In fact, some are life-saving. Statins, aspirin, and beta blockers together have been shown to cut death risk by 25-30% in high-risk patients. Newer drugs like SGLT2 inhibitors (dapagliflozin) have shown promise when added to standard heart failure therapy, reducing events by 14%.But here’s the catch: even good combinations need monitoring. That’s why fixed-dose combinations-like AstraZeneca’s new pill combining dapagliflozin, sacubitril, and valsartan-are gaining traction. They reduce pill burden, improve adherence, and lower the chance of harmful interactions by design.
How to Protect Yourself
You don’t need to be a doctor to prevent dangerous combinations. You just need to be informed and proactive.- Know your meds. Don’t just say “I take blood pressure pills.” List exact names and doses: “Lisinopril 10 mg daily, metoprolol 50 mg twice daily.”
- Use one pharmacy. Pharmacists can track interactions across all your prescriptions, OTC meds, and supplements. Most pharmacies have systems that flag dangerous combos before you even leave the counter.
- Ask about every new drug. When your doctor prescribes something new, ask: “Can this interact with anything else I’m taking?” Don’t assume they know your full list.
- Review your list every 30 days. Medications change. So should your list. Keep a written or digital copy updated and bring it to every appointment.
- Be wary of OTC and supplements. If you’re on a heart medication, don’t start a new supplement without checking. Even “natural” doesn’t mean safe.
- Know the warning signs. Unexplained bruising, muscle pain, swelling in your legs, dizziness, or confusion could be signs of a bad interaction. Don’t wait.
What the System Is Doing-And What It’s Not
Healthcare systems are starting to wake up. Medicare Part D now covers free medication therapy management (MTM) sessions-20 to 30 minutes with a pharmacist to review everything you take. Electronic health records can flag dangerous combinations with 85-92% accuracy. The FDA has updated labels on 27 heart drugs to include stronger warnings.But here’s the gap: only 37% of primary care doctors routinely screen for dangerous combinations during visits. And only 18% of patients tell their providers about OTC meds or supplements before using them.
The problem isn’t just lack of knowledge. It’s assumption. People assume their doctor knows what they’re taking. They assume their pharmacist will catch it. They assume OTC means safe. None of those assumptions are reliable.
What You Should Do Today
Take five minutes right now. Look at your medicine cabinet. Write down every pill, capsule, patch, and supplement you take-every day. Include the dose and how often. Then, call your pharmacist or doctor. Ask: “Are any of these combinations dangerous?”If you’re on warfarin, avoid ibuprofen and NSAIDs. If you’re on statins, ask if your rhythm medication could increase muscle damage risk. If you’re on an ACE inhibitor, skip potassium supplements. If you take digoxin, check if verapamil or diltiazem is in your regimen.
Heart medications save lives. But they can also harm you-if you don’t know how they work together. The safest heart isn’t the one on the most pills. It’s the one on the right ones-and none of the dangerous combinations.
Can I take ibuprofen with my blood pressure medication?
Generally, no. Ibuprofen and other NSAIDs can reduce the effectiveness of blood pressure meds like ACE inhibitors, beta blockers, and diuretics. They also increase fluid retention and raise the risk of kidney injury. If you need pain relief, ask your doctor about acetaminophen-but even that can interfere with warfarin. Never use NSAIDs long-term without medical supervision.
Is it safe to take St. John’s wort with heart medication?
No. St. John’s wort can interfere with several heart medications, especially warfarin, digoxin, and some beta blockers. It speeds up how your liver breaks down these drugs, making them less effective. In one case, a patient’s INR dropped from 3.0 to 1.2 after starting St. John’s wort, leading to a stroke. Always tell your doctor about supplements before taking them.
What should I do if I accidentally took a dangerous combination?
If you’ve taken a dangerous combination, watch for symptoms like unusual bleeding, swelling, chest pain, dizziness, confusion, or dark urine. Call your pharmacist or doctor immediately. If symptoms are severe-like fainting, difficulty breathing, or chest tightness-go to the ER. Don’t wait. Some interactions can cause harm within hours.
Do all pharmacies check for drug interactions?
Most pharmacies have systems that flag dangerous combinations, but they can’t catch everything-especially if you use multiple pharmacies or take supplements. Using one pharmacy for all your prescriptions improves safety. Also, pharmacists can only act if they know what you’re taking. Always disclose OTC meds and supplements when filling prescriptions.
Can I stop taking a medication if I’m worried about an interaction?
Never stop a heart medication without talking to your doctor. Stopping suddenly can be dangerous-for example, stopping beta blockers can cause rebound high blood pressure or even a heart attack. If you’re concerned about an interaction, ask your doctor for a safer alternative. They may switch you to a different drug or adjust the dose.





Comments (8)
Ashlyn Ellison
February 9, 2026 AT 00:37 AMMy grandma took 12 pills a day and died in her sleep from a combo no one saw coming. No one asked about the turmeric capsules she swore were 'just for inflammation.' We thought she was fine. She wasn't.
Tatiana Barbosa
February 10, 2026 AT 11:22 AMLook I get it you're scared but here's the real deal you don't need to panic you need to organize
Write down every single thing you take even the gummy vitamins
Use one pharmacy dont hop around
Ask your pharmacist to print you a interaction report
Do this once every 30 days
It takes 10 minutes
And it might save your life
Thats not drama thats responsibility
Monica Warnick
February 10, 2026 AT 14:00 PMOh my god this is terrifying I just found out my neighbor died last month because of this exact thing
She was on warfarin and started taking Advil for her arthritis
She didn't even think it was a big deal
One day she just bled out from a tiny cut on her finger
And the ER said it was 100% preventable
How is this not on every drug label in giant red letters
How is this not a national emergency
People are dying from stupid mistakes and no one is talking about it
Ken Cooper
February 10, 2026 AT 22:45 PMso i just checked my med list and i take lisinopril and a daily omega-3 and also i use that garlic supplement for 'heart health'... wait does garlic count as an interaction??
also my doc just prescribed me verapamil last week for palpitations... is that bad with my statin??
oh god i think i might be one of those 18% of people who dont tell their doc about supplements...
im calling my pharmacist right now
John McDonald
February 11, 2026 AT 12:24 PMMost people don't realize that the real danger isn't the drugs themselves
It's the assumption that because something is 'natural' or 'over-the-counter' it's harmless
St. John’s wort isn't a tea
It's a liver enzyme bomb
And ibuprofen isn't just 'a pain pill'
It's a silent killer when paired with ACE inhibitors
Stop treating meds like candy
Your heart doesn't care if it's FDA-approved or sold in a health food store
It only cares about chemistry
And right now your chemistry might be a ticking time bomb
Tom Forwood
February 12, 2026 AT 22:46 PMAs a paramedic in Texas I've seen 3 cases this year alone where someone took NSAIDs with their BP med and ended up in cardiac arrest
One guy was 54, fit, never smoked
Just took naproxen for his back pain for 2 weeks
His kidneys shut down, fluid backed up, heart gave out
He had no idea
And his doctor didn't ask about OTCs
Pharmacists can't save you if you don't tell them everything
And doctors can't fix what they don't know
So ask
And write it down
And bring it to every appointment
It's not paranoia
It's survival
Alex Ogle
February 13, 2026 AT 00:59 AMLet me tell you about my uncle
He was on digoxin for AFib
Got a new script for verapamil for high blood pressure
Didn't think twice
Three weeks later he was in the ICU with digoxin toxicity
His levels were off the charts
They said it was textbook
He didn't even know verapamil was a calcium channel blocker
He thought it was just 'another blood pressure pill'
And his cardiologist didn't check his med list properly
So now he's on a new regimen
But he's got kidney damage and a pacemaker
And the worst part?
He says he's still confused about why this happened
Because nobody sat down with him
And explained how the pieces fit together
Not just what each pill does
But how they fight each other
That's the gap
That's the failure
And it's killing people
Karianne Jackson
February 14, 2026 AT 23:05 PMI took ibuprofen with my blood pressure pill and I almost died. Don't do it. Just don't.