

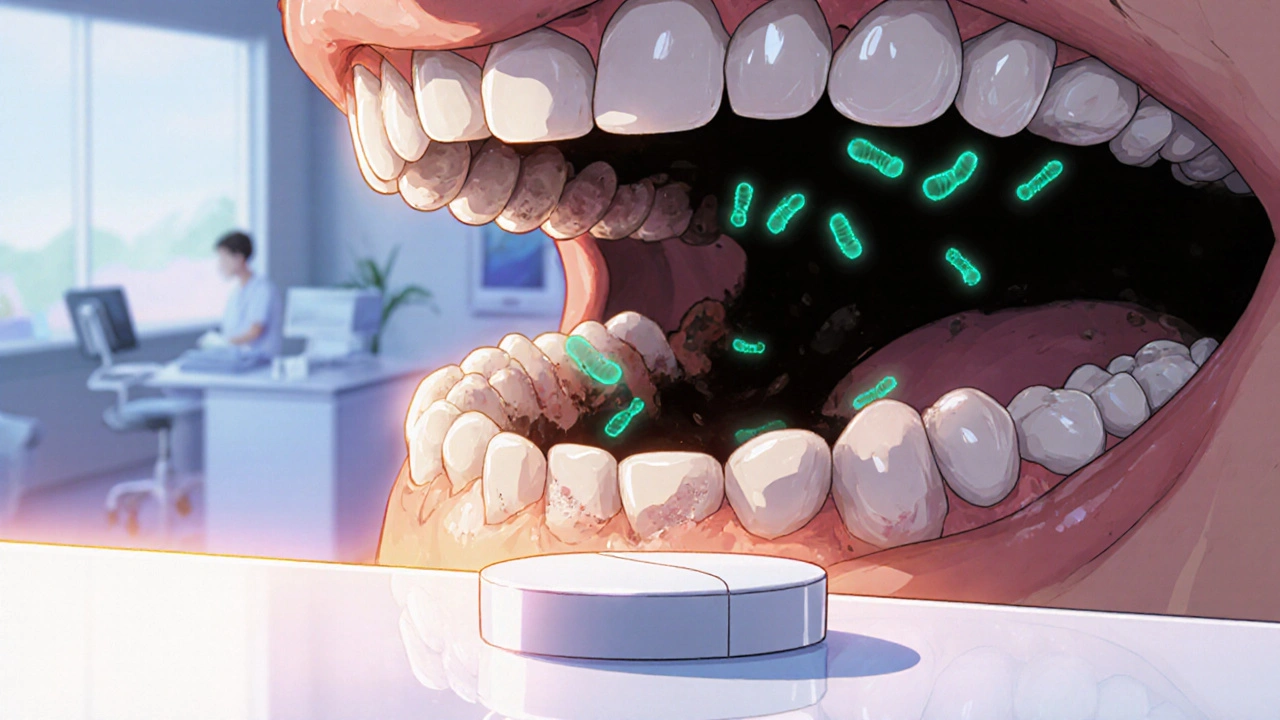
When dealing with antibiotic for gum disease, a medication that targets bacterial infection in the gums to halt the progression of periodontal disease. Also known as oral antibiotic therapy, it plays a key role in managing inflammation and tissue loss. If you’ve been prescribed an antibiotic for gum disease, you probably wonder how it fits into your overall care plan. First, understand that gum disease, an infection of the supporting structures of the teeth caused by bacterial plaque isn’t a single condition; it ranges from mild gingivitis to severe periodontitis. The most destructive form, periodontitis, a deep‑tissue infection that can lead to bone loss and tooth loss, often triggers the need for systemic antibiotics. The core idea is simple: antibiotics target the bacteria that have breached the gum line, while other measures tackle the source. This creates a semantic triple: antibiotic for gum disease encompasses periodontitis treatment. Another triple links hygiene to medication: effective oral hygiene reduces the need for antibiotics. Finally, dental plaque triggers gum disease, which may require antibiotic therapy. Understanding these connections helps you decide when antibiotics add real value.
Beyond the infection itself, several factors shape whether a clinician will prescribe an oral antibiotic, a drug taken by mouth to fight gum‑related bacteria. Severity of the infection, presence of systemic symptoms (fever, swelling), and the patient’s overall health status all matter. For example, a patient with uncontrolled diabetes may need antibiotics sooner because their immune response is weaker. The type of bacterial strain—often identified through a pocket‑site culture—also guides drug selection; common culprits include *Porphyromonas gingivalis* and *Aggregatibacter actinomycetemcomitans*. Timing is crucial: antibiotics work best when paired with professional cleaning that removes the bulk of plaque and calculus. This is why dentists pair drug therapy with scaling and root planing, creating a triple where prescribing antibiotics requires assessment of infection severity. Remember, antibiotics are an adjunct, not a replacement for mechanical plaque control.
Finally, consider the role of dental plaque, a sticky biofilm of bacteria that forms on tooth surfaces and oral hygiene, daily practices like brushing and flossing that keep plaque in check. Even with the best antibiotic, the infection will rebound if plaque isn’t managed. That’s why most treatment plans combine medication with a reinforced hygiene routine, regular dental visits, and sometimes adjunctive therapies like mouth rinses. Below, you’ll find a curated list of articles that dive deeper into specific antibiotics, dosing guidelines, side‑effect management, and how they fit into comprehensive gum‑disease care. Whether you’re a patient curious about your prescription or a professional looking for the latest evidence, the collection ahead offers practical insight you can act on right away.
Discover how secnidazole works, its dental dosing, safety tips, and when to choose it over other antibiotics for oral infections.