When your kidneys aren’t working right, what you eat matters more than you might think. For people with chronic kidney disease (CKD), protein isn’t just about building muscle or feeling full-it’s a balancing act that can slow damage, delay dialysis, or even help you live longer. But here’s the twist: the right amount of protein changes depending on how far your kidney disease has progressed. There’s no one-size-fits-all answer. Too little, and you risk wasting away. Too much, and your kidneys struggle even harder. So what should you actually be eating? Let’s break it down by stage.
Stage 1 and 2: Mild Kidney Damage, No Need to Panic
If you’re in stage 1 or 2 CKD, your kidneys are still doing most of their job. Your GFR (glomerular filtration rate) is 60 or higher. You might not even feel sick. But that doesn’t mean you can ignore protein. The Kidney Health Initiative an expert group focused on improving kidney care through research and guidelines recommends sticking to no more than 0.8 grams of protein per kilogram of your ideal body weight. For someone who weighs 150 pounds (about 68 kg), that’s roughly 54 grams a day.
That’s about the same as what healthy people are told to eat. But here’s where it gets interesting: a 2024 study in JAMA Network Open found that older adults with early-stage CKD who ate more protein-up to 1.3 grams per kilogram-actually had lower death rates. Why? Because for many older people, muscle loss and frailty are bigger threats than kidney damage. So if you’re over 65, or you’re losing weight without trying, your doctor might not push you to cut protein at all. The goal isn’t just to protect your kidneys-it’s to keep you strong.
Stage 3: The Turning Point
Stage 3 is where things shift. Your GFR drops below 60, meaning your kidneys are starting to lose their ability to filter waste. That’s when protein restriction becomes more important. The KDOQI Kidney Disease Outcomes Quality Initiative, the leading clinical guideline body for kidney care in the U.S. recommends 0.55 to 0.60 grams per kilogram. For a 150-pound person, that’s 40 to 54 grams daily.
But here’s the catch: you can’t just eat less protein-you need to make sure what you eat counts. About half of your protein should come from high-quality sources: eggs, milk, chicken, fish, lean beef, and soy. These contain all the essential amino acids your body can’t make on its own. The rest can come from plant sources like beans, lentils, and tofu. Why? Because plant proteins produce less urea and phosphate waste. A 2021 meta-analysis found that replacing just 30% of animal protein with plant protein cut the risk of kidney disease worsening by 14%.
Still, plant proteins aren’t perfect. They’re lower in lysine and methionine, two key amino acids. And if you’re in stage 3b (GFR 30-44), you might also need to watch potassium. A sweet potato or a banana might be healthy for someone else-but for you, it could raise your blood potassium to dangerous levels. That’s why working with a renal dietitian isn’t optional-it’s essential.
Stage 4 and 5: The Critical Zone
By stage 4, your kidneys are functioning at less than 30% of normal. At this point, protein restriction tightens further. DaVita’s 2023 guidelines suggest 0.6 grams per kilogram if your GFR falls below 25. That’s 40-45 grams a day for a 150-pound person. And yes, it feels hard. Many patients say they’re constantly hungry, weak, or tired. One Reddit user wrote: "Cutting my protein from 100g to 45g daily made me feel like I was slowly disappearing."
But here’s the reality: going too low can be just as dangerous as going too high. Studies show that 30-50% of people in stage 3-5 CKD develop protein-energy wasting-a condition where your body starts breaking down muscle just to survive. That’s why every gram counts. You need high-quality protein to preserve muscle, fight infection, and keep your body running.
Some patients are prescribed keto acid analogues like Ketosteril. These aren’t protein-they’re chemical building blocks that help your body make protein without creating waste. They’re used in about 15% of stage 4-5 patients in Europe. In the U.S., they’re less common, but they’re gaining traction. And if you’re diabetic, your target might be slightly higher: 0.8 to 0.9 grams per kilogram, according to the American Diabetes Association. Why? Because low protein can make blood sugar harder to control.
Animal vs. Plant Protein: What’s Really Better?
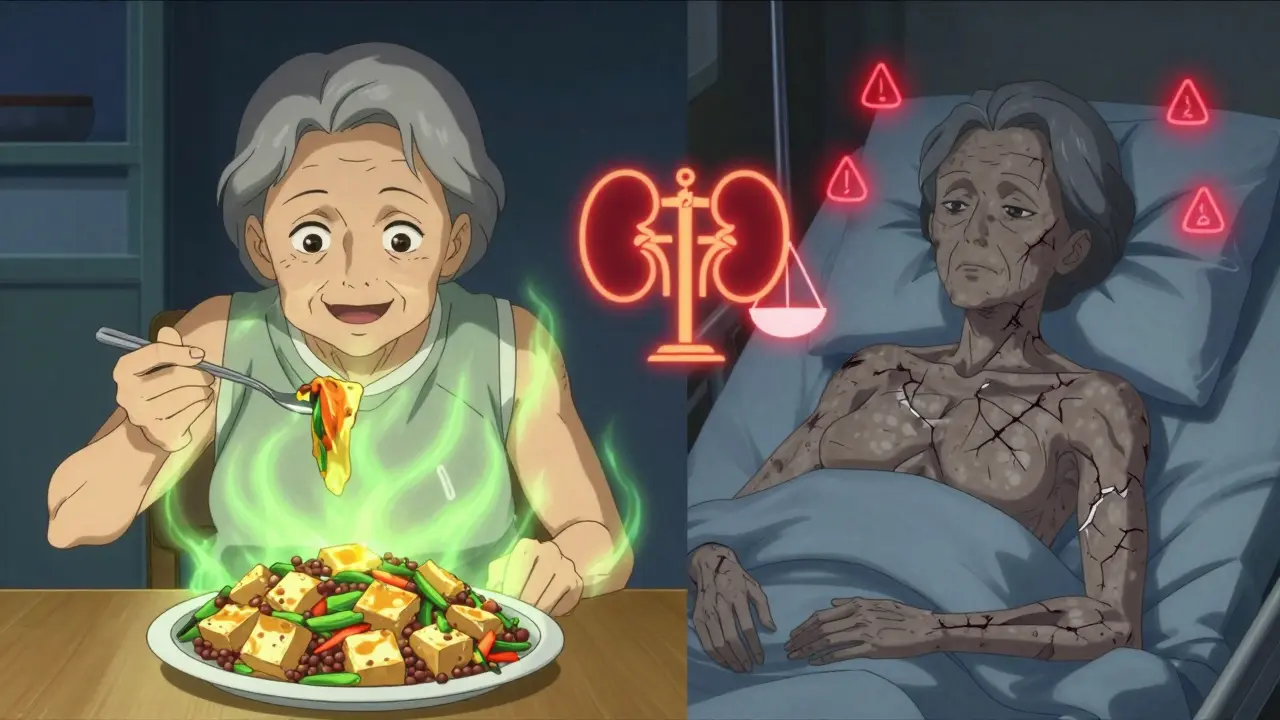
Not all protein is created equal. Animal proteins-like steak, chicken, and cheese-pack a punch of amino acids, but they also dump more urea, phosphate, and advanced glycation end products (AGEs) into your system. AGEs cause inflammation and oxidative stress, which speed up kidney damage. Red meat, in particular, can generate up to 50% more AGEs than plant sources.
Plant proteins-beans, lentils, nuts, tofu-produce 20-30% less waste. They’re also lower in saturated fat and sodium. But they come with trade-offs. They’re higher in potassium and phosphorus. A cup of lentils has 365 mg of potassium-more than a banana. For someone in stage 4 or 5, that’s risky. So you can’t just swap meat for beans and call it a day. You need to plan.
The smartest approach? Mix them. Use plant proteins for bulk and fiber, and anchor your meals with small portions of high-quality animal protein. A 3-ounce chicken breast (about the size of a deck of cards) gives you 21 grams of protein. Pair it with half a cup of cooked rice and a side of steamed cabbage. That’s a renal-friendly meal that keeps you full, nourished, and gentle on your kidneys.
Why Most People Struggle (And How to Succeed)
Let’s be honest: eating less protein is hard. A 2024 survey by the American Kidney Fund found that 74% of patients felt constantly hungry. 62% felt weak. 58% avoided social meals because they couldn’t eat what everyone else was having.
But there’s hope. Patients who work with a renal dietitian are 82% more likely to stick with their plan. Why? Because dietitians don’t just give numbers-they give meals. They help you use apps like MyFitnessPal with renal-specific databases. They teach you how to track protein in mixed dishes like pasta sauce or casseroles (87% of patients struggle with this). They show you how to use the NKF’s Protein Target Calculator a free online tool developed by the National Kidney Foundation to estimate daily protein needs based on weight and CKD stage, which has been downloaded over 47,000 times since 2023.
Meal prepping is another game-changer. Batch-cook lean chicken, portion out tofu, freeze vegetable soups without added salt. Use the Kidney Kitchen a resource from the National Kidney Foundation offering hundreds of low-protein, kidney-friendly recipes with nutritional breakdowns-it gets over 1.2 million visits a month. You don’t have to eat bland food. You just have to eat smarter.
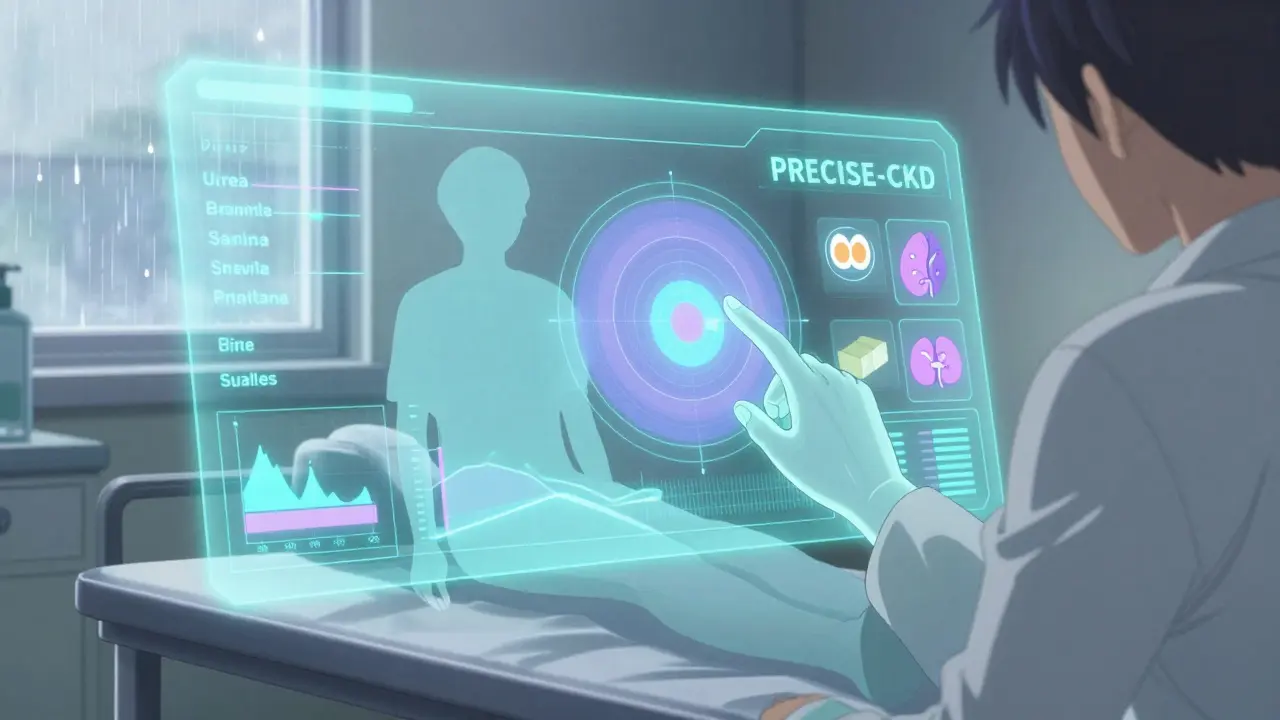
What’s Next? Personalized Protein
The future of renal nutrition isn’t about one number for everyone. The NIH-funded PRECISE-CKD trial is testing whether your protein target should be based on your body’s actual urea production-not just your weight. Some people naturally make more waste than others. Why should they all eat the same amount?
And then there’s the rise of precision nutrition. Machine learning algorithms are now being used to predict how individuals respond to protein changes, using data from genetics, blood tests, and even continuous glucose monitors. The goal? Give you a plan that works for you, not just the guidelines.
For now, the best advice is this: don’t guess. Get tested. Talk to a renal dietitian. Use the tools. And remember-this isn’t about deprivation. It’s about protecting your body so you can keep doing the things you love.
How much protein should I eat if I have stage 3 CKD?
For stage 3 CKD, aim for 0.55 to 0.60 grams of protein per kilogram of your ideal body weight. For example, if you weigh 150 pounds (68 kg), that’s about 40 to 54 grams of protein per day. At least half should come from high-quality sources like eggs, chicken, fish, or soy. Always check with your dietitian-your needs may vary if you’re diabetic, older, or losing weight.
Can I eat plant-based protein with kidney disease?
Yes, and it can be helpful. Plant proteins like beans, lentils, and tofu create less waste for your kidneys and may slow disease progression. But they’re often high in potassium and phosphorus, which can be dangerous in later stages. The key is balance: use plants for fiber and bulk, but don’t rely on them alone. Pair them with small amounts of high-quality animal protein to meet your amino acid needs.
Why do I feel weak on a low-protein diet?
Feeling weak is common if you’re not getting enough high-quality protein. Your body starts breaking down muscle to get the amino acids it needs. This is called protein-energy wasting, and it affects up to half of people with stage 3-5 CKD. The solution isn’t to eat more protein blindly-it’s to eat the right kind. Focus on small portions of eggs, fish, or lean meat, and consider talking to your doctor about keto acid analogues if you’re struggling.
Do I need to see a renal dietitian?
Yes, especially if you’re in stage 3 or beyond. Studies show patients who work with a renal dietitian have over three times higher adherence to their diet. Dietitians help you track protein accurately, avoid hidden sodium and phosphorus, and create meals you actually enjoy. Most insurance plans, including Medicare, now cover up to 3 hours of initial counseling and 2 hours of follow-up each year.
Is it true that higher protein intake can help older adults with CKD live longer?
Yes, according to a 2024 JAMA Network Open study. In older adults with early-stage CKD, eating more protein (up to 1.3 g/kg/day) was linked to lower death rates. Why? Because muscle loss and frailty are bigger risks than kidney decline in this group. The key is individualization. If you’re over 65, losing weight, or have other health issues, your doctor may recommend a higher protein target-not to protect your kidneys, but to keep you strong.
What to Do Next
Start by calculating your ideal body weight. Then, use the NKF’s Protein Target Calculator to get your daily number. Write down what you eat for three days. Look for hidden protein in bread, sauces, and snacks. Talk to your nephrologist about a referral to a renal dietitian. And don’t wait until you’re in stage 5. The best time to start managing your protein is now.