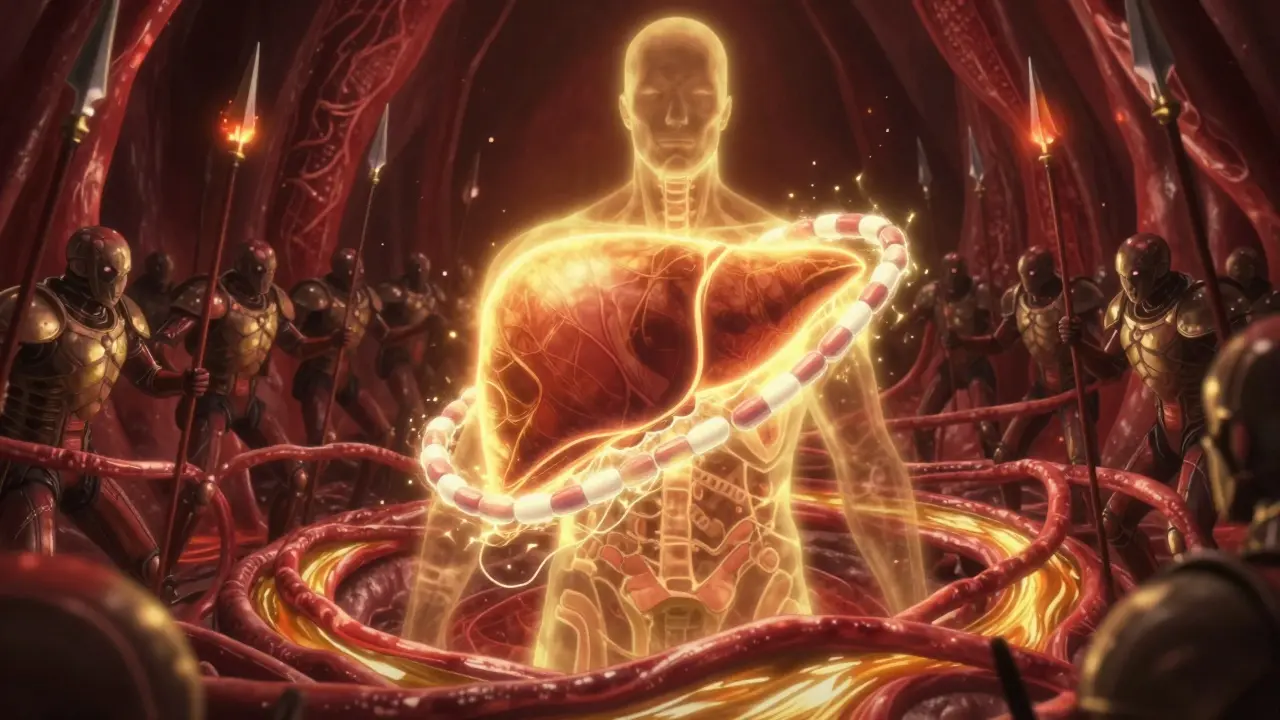
After a liver transplant, the real work begins-not in the hospital, but in your daily life. The surgery is just the start. What keeps your new liver working for years, even decades, is something far less glamorous: taking your pills on time, every single day, and knowing when something’s wrong before it’s too late. Many people think the transplant is the finish line. It’s not. It’s the beginning of a lifelong routine that can mean the difference between living well and losing the organ.
What Happens When Your Body Rejects the New Liver
Your immune system is designed to protect you. But after a transplant, that same system sees your new liver as an invader. This is called rejection. It doesn’t happen because you did something wrong-it’s just how your body reacts. The good news? Modern medicine has made rejection much rarer than it used to be. Still, it can happen at any time, even years after your transplant.There are three types of rejection, each with different timing and signs. Hyperacute rejection is rare today-less than 1% of cases-because doctors now do detailed blood tests before surgery to make sure your body won’t attack the liver right away. If it did happen, you’d feel sick within hours: your liver would stop working, your bilirubin levels would spike, and your skin might turn yellow. Thankfully, this is almost unheard of now.
Acute rejection is the most common. It usually shows up between one week and three months after surgery, but it can pop up even five or ten years later. You might not feel anything at first. That’s the dangerous part. But when symptoms do appear, they’re clear: a fever over 100°F, pain or tenderness near the transplant site, nausea, fatigue, dark urine, or swelling in your legs and belly. Your doctor will check your blood-especially liver enzymes like ALT and AST. If they’re high, it’s a red flag. In fact, a rise of 20% or more in these enzymes over a few days is often the first sign doctors look for.
Chronic rejection creeps in slowly. It doesn’t come with a sudden fever or sharp pain. Instead, you might notice you’re always tired, your appetite fades, or you gain weight without changing your diet. Blood tests show a gradual rise in bilirubin and alkaline phosphatase. Blood pressure might climb. Over time, the liver’s bile ducts narrow, and function drops. This type is harder to treat, which is why catching rejection early is so critical.
Why Your Medications Are Non-Negotiable
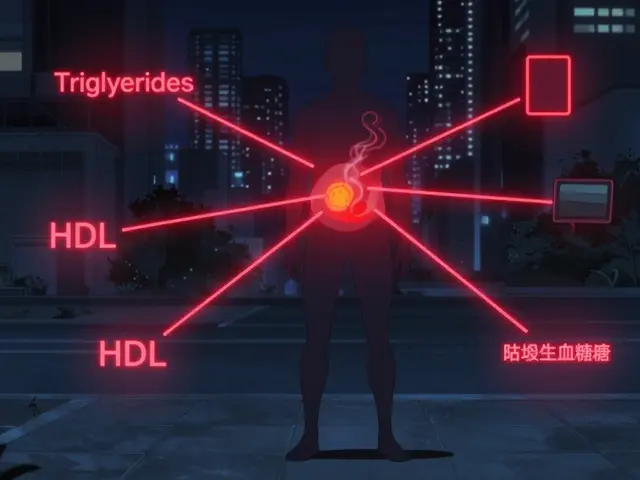
You’ll be on a mix of drugs for the rest of your life. These aren’t optional. They’re what keep your immune system from attacking your new liver. Most transplant patients take three types: calcineurin inhibitors (like tacrolimus or cyclosporine), antimetabolites (mycophenolate or azathioprine), and corticosteroids (prednisone).Tacrolimus is the most common. Your doctor will check your blood levels regularly to make sure you’re in the right range-usually 5 to 10 ng/mL in the first year. Too low, and rejection risks go up. Too high, and you risk kidney damage or nerve problems. That’s why you can’t just guess your dose. You need blood tests. Every month, sometimes more often.
Here’s the hard truth: missing just one or two pills a week can double your chance of rejection. A 2022 study from the American Journal of Transplantation found that patients who missed 20% of their doses had three times more rejection episodes than those who took every pill. And it’s not just about feeling sick. Sometimes, rejection happens quietly. You might have no symptoms at all. That’s why doctors say: adherence isn’t about how you feel-it’s about what you do.
According to the National Kidney Foundation, every 10% drop in medication adherence increases your risk of graft failure by 23%. That’s not a small risk. That’s life-changing. And it’s preventable.
The Real Challenges of Taking Pills Every Day
Let’s be honest: taking pills three or four times a day, every day, for the rest of your life is hard. You’ll be taking up to 12 pills a day in the first year. Some need to be taken on an empty stomach. Others with food. Some at night. Some in the morning. It’s easy to mix them up.Side effects make it worse. Tacrolimus can cause tremors, headaches, or trouble sleeping. Steroids might make you gain weight, cause mood swings, or raise your blood sugar. You might feel like the meds are as hard to live with as the disease was. But stopping them? That’s worse.
Cost is another big issue. Without insurance, these drugs can cost over $28,000 a year. Many patients skip doses because they can’t afford them. That’s why you need to talk to your transplant team. There are patient assistance programs. Generic versions exist. Pharmacies can help you find savings. Don’t suffer in silence.
And then there’s the mental load. After months of hospital visits and recovery, you just want to feel normal. But you’re still tied to pills, blood tests, and doctor appointments. It’s exhausting. That’s why support matters.

How to Stay on Track-Proven Strategies
You don’t have to figure this out alone. Here’s what actually works:- Use a pill organizer-the kind with compartments for morning, afternoon, evening, and night. 63% of long-term transplant survivors use one.
- Set phone alarms-one for each dose. A 2022 study in JAMA Internal Medicine found that reminders improved adherence by 37%.
- Involve a family member-someone who checks in, helps you refill, or even takes the pill with you. Studies show this cuts rejection risk by 28%.
- Use smart pill bottles-these record when you open them and send alerts if you miss a dose. Centers like Mayo Clinic report a 22% drop in rejection among users.
- Meet with your transplant pharmacist monthly-they don’t just fill prescriptions. They help you understand side effects, check for drug interactions, and adjust your plan. Johns Hopkins has 92% adherence rates using this model.
Some centers now use pharmacogenomic testing (like the FDA-approved XyGlo test) to tailor doses based on your genes. This isn’t standard everywhere yet, but it’s coming fast. If you’re eligible, ask your doctor.
What to Do If You Think Something’s Wrong
If you notice any of these signs, don’t wait: call your transplant team immediately.- Fever over 100°F
- Pain or swelling in your upper right abdomen
- Dark urine or pale stools
- Yellowing of skin or eyes (jaundice)
- Unexplained weight gain (5+ pounds in 48 hours)
- Extreme fatigue that doesn’t go away
- Changes in your usual blood test results
Don’t assume it’s just a cold. Don’t think, “I’ll wait and see.” Rejection can progress fast. Early treatment with steroids or other drugs can reverse it. Delay? You could lose the liver.
The Long-Term Picture: What Adherence Really Means
Data from the University of Pittsburgh tracks over 15,000 transplant patients for 20 years. The results are clear: those who took 95% or more of their pills had an 85% chance of still having a working liver 10 years later. Those who missed more than 20% of doses? Only 42% kept their transplant alive.It’s not about being perfect. It’s about being consistent. Missing a dose once in a while? Talk to your team. They’ll help you fix it. But making it a habit? That’s when things start to unravel.
And here’s something hopeful: new treatments are on the horizon. The ImmuKnow assay (used in 62% of U.S. centers) can now measure your immune activity without a biopsy. Some patients are even being tested in trials that aim to stop immunosuppression entirely-by training the body to accept the new liver. In one study, 40% of participants achieved this after 18 months.
But none of that matters if you stop taking your pills.
Final Thought: This Is Your Lifeline
Your liver transplant gave you a second chance. But that chance depends on you-not your surgeon, not your doctor, not your insurance. It depends on whether you open that pill bottle today. And tomorrow. And the next day.It’s not glamorous. It’s not exciting. But it’s everything.
Can you stop taking transplant meds after a while?
No. Almost all liver transplant recipients need to take immunosuppressants for life. Stopping-even if you feel fine-triggers rejection in most cases. There are rare exceptions, like in clinical trials where patients are carefully weaned off meds under strict monitoring. But outside of those studies, never stop or change your dose without your transplant team’s approval.
What happens if I miss a dose of tacrolimus?
If you miss one dose, take it as soon as you remember-if it’s within a few hours of your usual time. If it’s been longer, skip it and take your next dose at the regular time. Never double up. Missing doses frequently raises your risk of rejection, even if you don’t feel sick. Talk to your pharmacist or transplant coordinator about setting up reminders or using a smart pill bottle to stay on track.
Are there cheaper alternatives to expensive transplant drugs?
Yes. Generic versions of tacrolimus, mycophenolate, and prednisone are widely available and just as effective. Many patients save thousands per year by switching. Your transplant pharmacy or social worker can help you apply for patient assistance programs, coupons, or Medicaid coverage. Never skip doses because of cost-there are always options.
Can you get a second transplant if the first one fails?
Yes, but it’s more complex. Second transplants have higher rejection risks because your body has already been exposed to foreign tissue. You’ll likely need stronger immunosuppression and more medications. Success rates are lower than for first transplants, but many people live for years after a second transplant. The key is preventing the first one from failing in the first place-through strict adherence.
How often do I need blood tests after a transplant?
In the first month, you’ll likely have blood tests weekly. Months 2-3: every two weeks. After that, monthly checks are standard for the first year. Once you’re stable, tests may drop to every 2-3 months. But if you miss doses or have symptoms, your team will test more often. Liver enzymes (ALT, AST), bilirubin, and creatinine are the key numbers they watch.
Can alcohol affect my transplant liver?
Yes. Even small amounts of alcohol can damage your new liver, especially when combined with immunosuppressants. Most transplant centers recommend complete abstinence. If you’re struggling with alcohol use, ask your team for support. Your liver didn’t just survive surgery-it needs protection every day.
Sticking to your meds isn’t just about following rules. It’s about honoring the gift you were given. Your liver is working because of science, because of a donor, and because of you.







Comments (14)
Tatiana Barbosa
February 11, 2026 AT 02:30 AMI can't believe how many people treat their transplant like it's a one-time fix. It's not. It's a daily commitment. I've been 8 years out and still take 10 pills a day. Some days suck, but I'd rather be alive and slightly tired than dead. This post nailed it. Your liver doesn't care if you're 'feeling fine'. It just knows if you took your meds or not.
Brandon Osborne
February 11, 2026 AT 13:26 PMI'm sorry but I have to say this: if you're too lazy or too broke to take your pills, maybe you didn't deserve the transplant in the first place. People die waiting for organs. You got one. Now do the bare minimum. This isn't a privilege, it's a responsibility. Stop making excuses and start taking responsibility.
Susan Kwan
February 11, 2026 AT 18:26 PMOh wow, another post telling people they're not doing enough. How about we stop shaming people for being poor or mentally exhausted? The system is broken. $28k a year for meds? That's not 'adherence'-that's a death sentence for anyone without good insurance. Blame the system, not the patient.
Ken Cooper
February 13, 2026 AT 07:05 AMso i got my transplant 3 yrs ago and honestly the hardest part wasnt the pills, it was the constant fear. like every time i got a headache or felt tired i thought 'is this it? is my body starting to reject it?' i started using a smart pill bottle and it changed everything. now i just get a text if i miss a dose. my wife checks in too. its not perfect but its better. also i switched to generics and saved like 15k a year. just saying.
MANI V
February 15, 2026 AT 03:24 AMThis is why society is collapsing. People think they can just take a miracle and then go back to their old lives. You think your liver is a toy? You think the donor's family didn't lose someone? You owe them your life. If you miss a pill, you're not just risking your health-you're disrespecting a death. Wake up.
John McDonald
February 16, 2026 AT 14:31 PMI'm a transplant nurse. I see this every day. The #1 reason for graft failure isn't rejection-it's non-adherence. And the #1 reason for non-adherence? Cost. I've had patients choose between insulin and tacrolimus. That's not a choice. We need policy change. But until then, use the tools: pill organizers, reminders, patient programs. You're not alone. We're here to help.
Random Guy
February 18, 2026 AT 01:17 AMI took my meds for 6 months. Then I said 'screw it' and stopped. Guess what? I'm still alive. Maybe your liver is tougher than they say. Maybe the whole 'you'll die if you miss one pill' thing is just fear-mongering. I'm living proof. They're just trying to keep you dependent on Big Pharma.
Joseph Charles Colin
February 19, 2026 AT 10:50 AMFor those asking about pharmacogenomics: the XyGlo test is FDA-cleared for tacrolimus dosing based on CYP3A5 genotype. Patients with CYP3A5*1/*1 metabolize tacrolimus 3x faster than poor metabolizers. Standard dosing leads to underexposure in rapid metabolizers, increasing rejection risk. Testing reduces variability by 68%. Ask your center if they offer it. It's not experimental-it's evidence-based.
Ryan Vargas
February 20, 2026 AT 13:38 PMLet's think deeper. Why are we so obsessed with 'adherence'? We treat the body like a machine that must be perfectly calibrated. But what if rejection is not a failure of the patient-but a failure of the medical paradigm? What if we're forcing immune suppression instead of teaching tolerance? The real solution isn't more pills-it's reprogramming the immune system. We're treating symptoms, not the root. The donor organ is a mirror. It reflects our arrogance: we think we can control life. But life? Life resists control.
Joshua Smith
February 21, 2026 AT 20:29 PMJust wanted to say thanks for this. I was about to skip my morning dose yesterday because I was 'so tired.' Then I read this and thought-this is what my donor gave up their life for. I took it. Still tired. Still alive. That's the trade-off. No drama. Just gratitude.
Andy Cortez
February 23, 2026 AT 00:05 AMI'm not missing pills. I'm just... forgetting. Sometimes. I'm not lazy. I have PTSD from the hospital. The smell of antiseptic still makes me panic. I don't need another lecture. I need help. And if you're gonna lecture me, at least tell me where to get a free pill organizer. Or a therapist. Or someone who gets it.
glenn mendoza
February 24, 2026 AT 02:10 AMTo the individual who stated that non-adherence is a moral failing: this perspective is not only unhelpful, it is clinically dangerous. Adherence is a behavioral health outcome, not a moral judgment. Depression, cognitive load, financial strain, and systemic barriers are real. Compassion, not condemnation, improves outcomes. The data is clear: supportive interventions reduce rejection by 40%. Shame does not.
Patrick Jarillon
February 24, 2026 AT 06:31 AMThey say 'take your pills' like it's that simple. But what if the pills are making you sicker than the disease? Tacrolimus gave me kidney failure. Prednisone gave me diabetes. I'm not rejecting the liver-I'm rejecting the treatment. They told me to 'live with it.' But what if I don't want to live like this? What if the cure is worse than the disease? I'm not a statistic. I'm a person.
PAUL MCQUEEN
February 25, 2026 AT 10:56 AMThis whole post is just a pharmaceutical ad. They want you dependent. They don't care if you live. They care if you keep buying. The real solution? Regrow your own liver. We're already doing it in mice. Why aren't we doing it in humans? Because it's cheaper to sell pills. Wake up.