When you twist your ankle, slam your finger in a door, or get a bad backache after lifting something heavy, you’re feeling nociceptive pain. It’s not nerve damage. It’s not mysterious. It’s your body’s alarm system screaming because something’s physically hurt - a torn muscle, a bruised bone, a swollen joint. This kind of pain makes up about 85% of all acute pain cases, according to a 2022 study in Pain Medicine. And how you treat it matters - not just for comfort, but for recovery.
What Nociceptive Pain Actually Is
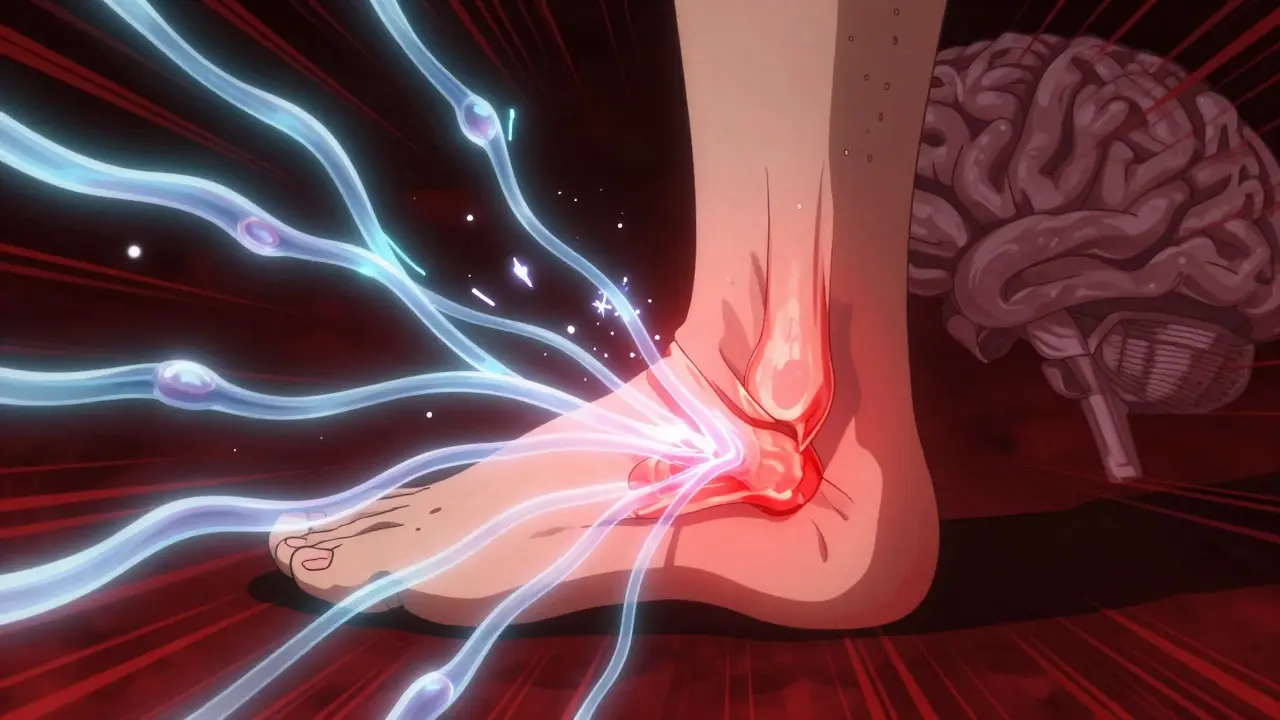
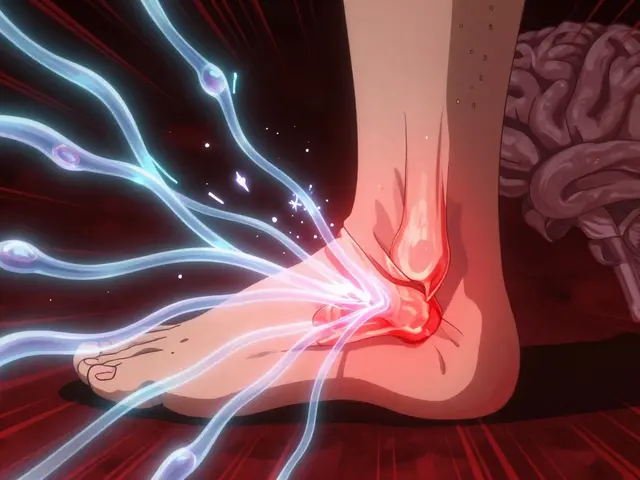
Nociceptive pain comes from real, physical damage to your skin, muscles, tendons, bones, or organs. It’s not in your head. It’s not imagined. Your body has special nerve endings - called nociceptors - scattered all over your tissues. These aren’t pain sensors like a thermometer. They’re more like tripwires. When something harmful happens - extreme heat, crushing pressure, or chemical changes from inflammation - they fire off signals to your brain. That’s pain. There are three main types:- Superficial somatic: Sharp, stinging pain from cuts, burns, or scrapes. These signals travel fast through Aδ fibers.
- Deep somatic: Dull, aching, throbbing pain from sprains, fractures, or muscle strains. Slower C fibers carry this.
- Visceral: Deep, hard-to-pinpoint pain from organs - like a kidney stone or appendicitis. These receptors usually stay quiet until inflammation wakes them up.
Understanding this helps you pick the right treatment. If your pain is swollen, red, and worse with movement - it’s inflammation driving it. That’s where NSAIDs come in.
NSAIDs: The Inflammation Killers
NSAIDs - like ibuprofen, naproxen, and aspirin - don’t just mask pain. They attack the source. They block enzymes called COX-1 and COX-2. COX-2 is the one that makes prostaglandins, the chemicals that cause swelling, heat, and pain at injury sites. Less swelling? Less pain. Faster healing. A 2023 Cochrane Review looked at 35 studies with nearly 8,000 people. The result? Ibuprofen 400mg gave 50% pain relief to 49% of people with sprains and strains. Placebo? Only 32%. That’s a clear edge. For acute injuries - think ankle sprains, tennis elbow, or post-surgery swelling - NSAIDs aren’t just helpful. They’re often essential. Real-world feedback backs this up. On Reddit’s r/PainMedicine, 68% of users said NSAIDs worked better for injury pain. Physical therapists commonly recommend 600mg of ibuprofen three times a day for the first few days after a sprain. Why? Because reducing inflammation speeds recovery by 2-3 days, according to clinical guidelines.Acetaminophen: The Quiet Player
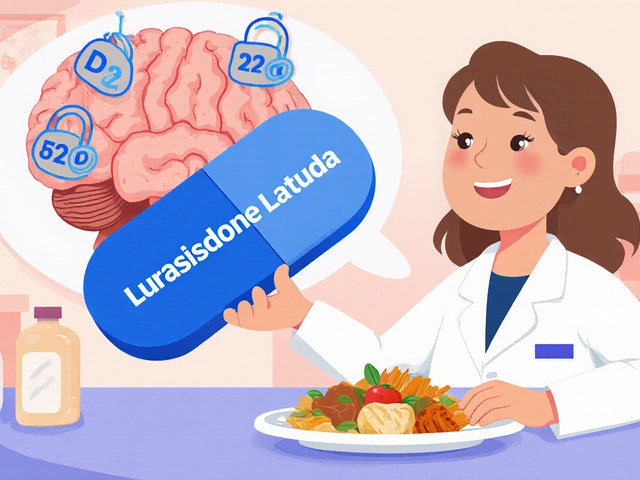
Acetaminophen (paracetamol) doesn’t reduce swelling. It doesn’t touch inflammation. So why do so many people use it? It works mostly in the brain. It’s thought to block a version of COX called COX-3 and may also affect serotonin pathways. But even after 140 years of use, experts still debate exactly how it works. A 2022 JAMA analysis found acetaminophen helped only 39% of people with low back pain. Ibuprofen? 48%. For mild headaches or minor aches without swelling, it’s fine. But for anything with inflammation - it’s not the best tool. On Drugs.com, 74% of users rated acetaminophen highly for tension headaches. Why? Because it’s gentle on the stomach. No burning, no nausea. That’s why it’s the go-to for kids, older adults, and people with sensitive guts. But here’s the catch: it’s weak where it counts. If your pain is moderate to severe and tied to tissue damage, acetaminophen often falls short. A 2020 BMJ analysis showed the benefit over placebo for many common pains is tiny - especially at over-the-counter doses.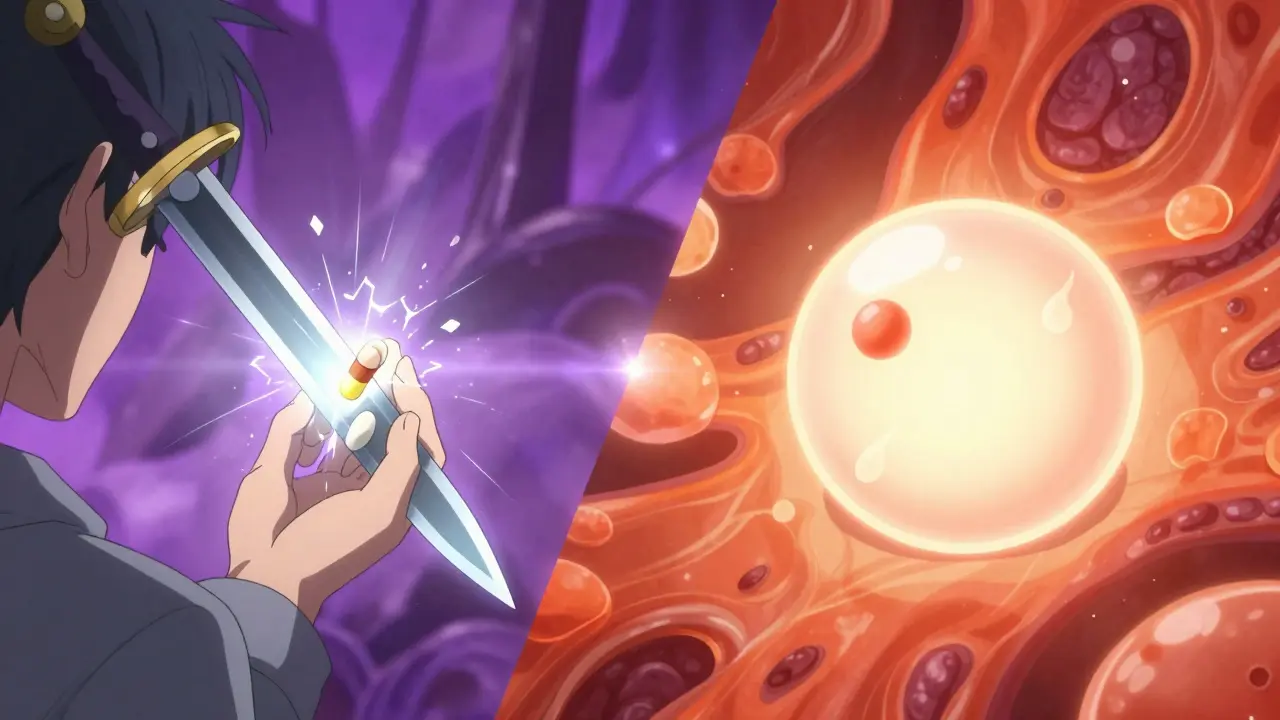
When to Choose Which
You don’t need a doctor to decide - if you know what you’re treating.- Choose NSAIDs if: Your pain is swollen, warm, worse with movement. Sprains, arthritis flare-ups, tendonitis, post-surgical pain. Ibuprofen 400mg every 6-8 hours for 3-7 days is standard. Naproxen works too, but lasts longer - good for overnight relief.
- Choose acetaminophen if: Your pain is dull, constant, no swelling. Tension headaches, mild backaches, post-dental work discomfort. Stick to 650-1,000mg every 6 hours. Don’t go over 3,000mg a day if you have liver issues.
For mixed pain - like osteoarthritis with occasional flare-ups - many people combine both. A 2022 Mayo Clinic survey found 61% of chronic pain patients did this. They reported 32% better control than either drug alone.
Safety: The Hidden Costs
NSAIDs aren’t harmless. Long-term use can cause stomach ulcers. The FDA says 1-2% of people on chronic NSAIDs get serious GI problems. Heart risks? Real. High-dose diclofenac doubles the chance of heart attack, according to a 2017 Lancet study. That’s why low-dose, short-term use is key. Acetaminophen? It’s safer for your stomach. But your liver? That’s another story. The max safe daily dose is 4,000mg - but many people don’t realize it’s in cold medicines, sleep aids, and combo pills. Taking two products with acetaminophen? Easy to overdose. 150-200mg per kg can be fatal. Liver failure from accidental overdose is the #1 cause of acute liver failure in the U.S.Pro tip: If you need NSAIDs long-term, ask about a proton pump inhibitor (PPI) like omeprazole. A 2021 meta-analysis showed it cuts ulcer risk by 74%.
What’s New and What’s Next
Topical NSAIDs - like diclofenac gel - are gaining ground. They deliver pain relief right to the sore spot with only 30% of the systemic exposure of pills. Less stomach trouble. Less heart risk. Great for knees, elbows, wrists. New formulations like Vimovo (naproxen + esomeprazole) combine pain relief with stomach protection. The TARGET trial showed a 56% drop in ulcers. For acetaminophen, research is looking at combinations. The FDA approved Qdolo (tramadol + acetaminophen) in 2022 for moderate-to-severe pain. And future drugs? Eli Lilly’s LOXO-435 targets TRPV1 channels - the same ones acetaminophen might affect - to block visceral pain without side effects. Phase II trials for IBS pain are promising.Bottom Line: Match the Drug to the Injury
Nociceptive pain isn’t one-size-fits-all. If your tissue is inflamed, reach for an NSAID. It reduces swelling, not just pain. If it’s just a dull ache with no redness or heat, acetaminophen is a safe, quiet option. Don’t default to what’s on your shelf. Ask yourself: Is it swollen? Is it worse with movement? Is it hot to the touch? If yes - NSAID. If no - acetaminophen. And never mix painkillers without checking labels. A single extra pill with acetaminophen can push you over the edge. Same with NSAIDs - don’t take them for weeks without a plan. Your body knows when it’s injured. The right medicine helps it heal - not just numb it.Is acetaminophen better than ibuprofen for a sprained ankle?
No. A sprained ankle involves inflammation - swelling, warmth, bruising. Ibuprofen reduces that inflammation, which speeds healing. Acetaminophen only dulls the pain. It won’t reduce swelling. Studies show ibuprofen gives better pain relief and faster recovery for sprains. Use acetaminophen only if you can’t take NSAIDs.
Can I take NSAIDs and acetaminophen together?
Yes, and many people do. Combining them often gives better pain control than either alone. For example, 650mg acetaminophen plus 400mg ibuprofen every 6 hours is a common regimen for moderate pain. Just make sure you’re not doubling up on acetaminophen - check all your meds. Don’t exceed 3,000mg of acetaminophen per day if you have liver issues, and avoid long-term NSAID use without medical advice.
Why do doctors recommend acetaminophen for kids?
Because it’s easier on the stomach and doesn’t carry the same bleeding or kidney risks as NSAIDs in children. The American Academy of Pediatrics recommends acetaminophen as first-line for fever and mild pain in kids. NSAIDs are used too - especially for inflammation like juvenile arthritis - but acetaminophen is the default for most common aches and fevers.
Is acetaminophen safe for people with heart disease?
Yes, generally. Unlike NSAIDs, acetaminophen doesn’t raise blood pressure or increase heart attack risk. That’s why it’s often the preferred painkiller for people with heart disease, kidney problems, or a history of stomach ulcers. But always check with your doctor - especially if you have liver disease or drink alcohol regularly.
How long should I take NSAIDs for a muscle strain?
For most acute strains, 3-7 days is enough. Start with ibuprofen 400mg every 6-8 hours, but only if swelling is present. Don’t use them longer than a week without seeing a doctor. Long-term use increases risks like stomach bleeding and kidney damage. If pain lasts beyond 10 days, the injury may need more than just painkillers - physical therapy or imaging might be needed.
What’s the safest NSAID for occasional use?
Ibuprofen at standard doses (200-400mg) is generally the safest for occasional use. Naproxen lasts longer but has a slightly higher heart risk. Aspirin isn’t ideal for pain - it’s better for blood thinning. Always take NSAIDs with food. Avoid them if you’re pregnant, have kidney disease, or are over 65 without medical supervision.






Comments (14)
Jennifer Glass
January 6, 2026 AT 01:06 AMInteresting breakdown. I’ve always wondered why my physical therapist always pushes ibuprofen over Tylenol after sprains. Now it makes sense-NSAIDs aren’t just masking pain, they’re actually helping the body heal faster by calming inflammation. I used to think it was just placebo effect, but the Cochrane data here is solid.
Jacob Milano
January 7, 2026 AT 04:44 AMMan, I used to pop acetaminophen like candy after my weekend basketball games. Thought it was doing the job. Turns out I was just silencing the alarm while my ankle kept screaming. Started switching to ibuprofen after a bad sprain last year-swelling went down in half the time. My knees thank me now.
Joseph Snow
January 7, 2026 AT 23:07 PMLet’s be real-this whole NSAID vs. acetaminophen narrative is pushed by Big Pharma. The FDA knows NSAIDs cause heart attacks. Why are they still on shelves? And why is acetaminophen’s liver toxicity ignored? They don’t want you to know how dangerous either option is. Just take a cold shower and endure the pain-it’s cheaper and safer.
Akshaya Gandra _ Student - EastCaryMS
January 9, 2026 AT 17:12 PMWait so if i have headache and no swelling i shoudl take tylenol? but what if i have both? like my head hurts AND my neck is stiff? what do i do? 😅
en Max
January 11, 2026 AT 17:10 PMWhile the clinical data presented is methodologically sound, it is imperative to acknowledge the confounding variables inherent in self-reported pain metrics. The efficacy differential between NSAIDs and acetaminophen may be attenuated by placebo response bias, particularly in studies utilizing non-blinded participant cohorts. Additionally, pharmacokinetic variability across populations must be considered.
John Wilmerding
January 12, 2026 AT 05:47 AMFor anyone considering long-term NSAID use: always pair it with a PPI like omeprazole. The 74% reduction in ulcer risk isn’t just a stat-it’s life-changing. I’ve been on naproxen for osteoarthritis for five years. Without the PPI, I’d be in the ER right now. Don’t wait for bleeding to start before you protect your stomach.
Peyton Feuer
January 12, 2026 AT 16:11 PMjust wanted to say thanks for writing this. i’ve been taking tylenol for my lower back for months and wondering why it never really helped. switched to ibuprofen last week and wow. my back doesn’t feel like it’s got a brick on it anymore. also learned i was taking tylenol in my cold medicine too-oops.
Terri Gladden
January 12, 2026 AT 23:38 PMOMG I JUST REALIZED I’VE BEEN TAKING IBUPROFEN AND TYLENOL TOGETHER EVERY NIGHT FOR A MONTH AND I DIDN’T EVEN KNOW THEY BOTH HAVE ACETAMINOPHEN IN THEM WHAT IF I OVERDOSED WHAT DO I DO IM DYING
Angie Rehe
January 14, 2026 AT 07:11 AMOf course the article ignores that NSAIDs inhibit tissue regeneration. You think reducing inflammation helps healing? No-it suppresses the very immune response that rebuilds tissue. Your ‘faster recovery’ is just temporary numbness masking underlying damage. You’re trading long-term function for short-term comfort. That’s not medicine-it’s chemical denial.
Siobhan Goggin
January 16, 2026 AT 07:05 AMI’ve been using topical diclofenac gel for my knee arthritis and it’s been a game-changer. No stomach upset, no dizziness, just quiet relief. I wish more people knew about it. It’s like giving your joint a hug without swallowing a pill.
Shanna Sung
January 17, 2026 AT 10:24 AMThey’re lying about the liver damage. Acetaminophen is fine. It’s the sugar in the pills that’s killing people. The FDA is in bed with Big Sugar. Also, NSAIDs are made by the same companies that make antidepressants. You’re being manipulated.
Vikram Sujay
January 18, 2026 AT 20:58 PMThere is an elegant simplicity in matching pharmacological action to pathophysiological mechanism. Nociceptive pain, as a biological signal of tissue disruption, demands intervention at the site of inflammation-not merely at the level of central perception. The distinction between symptomatic relief and mechanistic intervention is not trivial-it is the foundation of evidence-based practice.
Jay Tejada
January 19, 2026 AT 23:23 PMSo let me get this straight… you’re telling me I’ve been paying $10 a bottle for Tylenol when I could’ve just taken ibuprofen and actually gotten better? And now I’m supposed to feel bad because I didn’t know? Classic. Thanks for the guilt trip, doc.
Enrique González
January 21, 2026 AT 17:20 PMJust started using Vimovo after my knee surgery. No stomach issues. Pain gone in 3 days. I’m not a doctor, but this stuff works. If you’ve been struggling with NSAID side effects, give it a shot. Your gut will thank you.