Emergency Contraceptive Selector
Key Takeaways
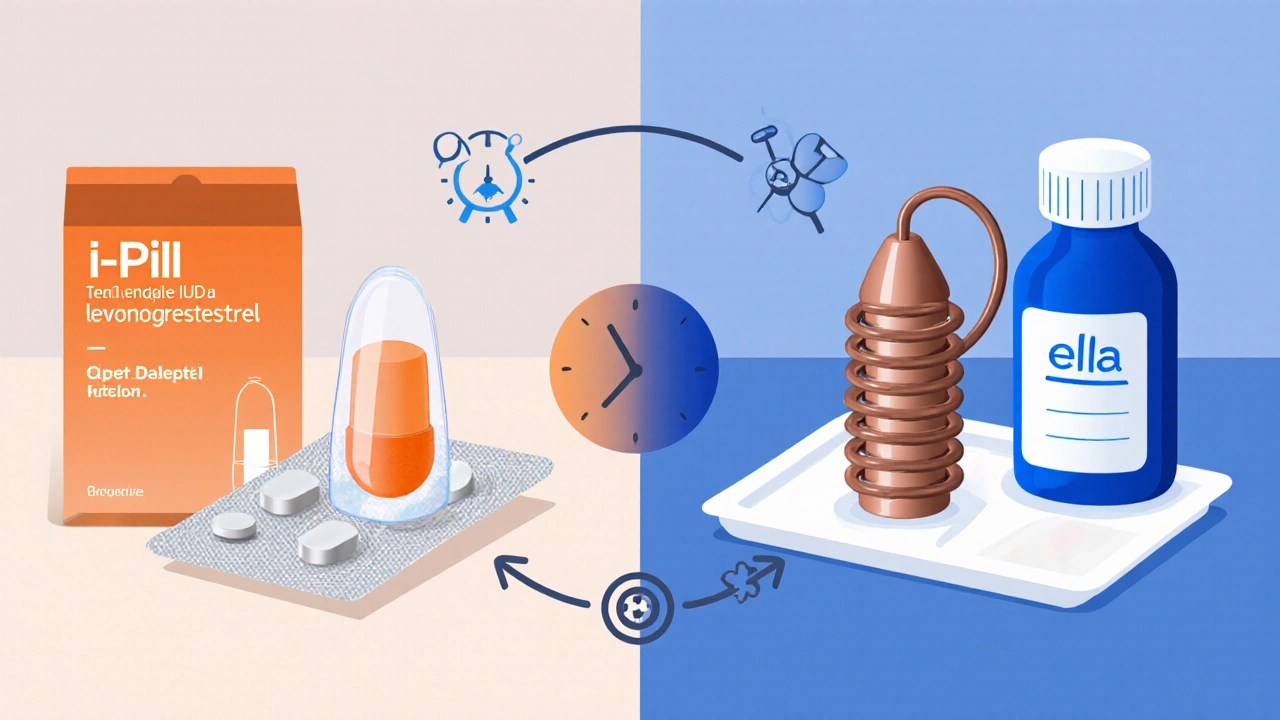
- The I‑Pill (levonorgestrel) is most effective when taken within 72hours, but efficacy drops sharply after 24hours.
- Ulipristal acetate (e.g., Ella) works up to 120hours and maintains higher efficacy throughout that window.
- A copper IUD can prevent pregnancy up to 5days after intercourse and also offers long‑term birth control.
- Side‑effect profiles differ: levonorgestrel may cause nausea, ulipristal can affect menstrual timing, copper IUD can cause heavier periods.
- Cost and access vary across the UK - NHS pharmacies provide levonorgestrel for free, while ulipristal and IUDs often require a prescription and a modest fee.
When an unprotected encounter happens, the first question is usually "What should I take?" The market is crowded with pills, regimens, and even a device that doubles as a regular contraceptive. This guide breaks down the most common options, focusing on the I‑Pill (levonorgestrel) and the viable alternatives you’ll hear about at the pharmacy or online.
How the I‑Pill Works
I‑Pill is a single‑dose emergency contraceptive pill that contains 1.5mg of levonorgestrel, a synthetic progestogen. It works primarily by delaying or preventing ovulation; it does not terminate an existing pregnancy. Because levonorgestrel mimics the hormone progesterone, it signals the body that it’s not the right time to release an egg. If taken before the luteinising hormone (LH) surge, fertilisation cannot occur.
Timing matters. Studies from 2024 show a 95% success rate when taken within 24hours, dropping to about 58% after 72hours. The pill is available over the counter at most UK pharmacies, and the NHS supplies it free of charge for individuals under 25.
What the Main Alternatives Are
Four alternatives dominate the emergency‑contraception landscape in the UK:
- Ella (ulipristal acetate 30mg) - a prescription‑only pill that remains effective up to 120hours.
- Generic levonorgestrel tablets (often sold as Levonelle or Next Choice) - identical active ingredient to the I‑Pill but typically cheaper.
- The copper IUD (Paragard) - a non‑hormonal device inserted by a clinician within five days of intercourse, offering >99% efficacy and ongoing contraception.
- The Yuzpe regimen - a combination of standard combined oral contraceptive pills taken in two doses 12hours apart.
Each option has distinct pros and cons, which we’ll explore in the comparison table.
Comparison Table
| Attribute | I‑Pill (Levonorgestrel) | Ella (Ulipristal acetate) | Generic Levonorgestrel | Copper IUD | Yuzpe regimen |
|---|---|---|---|---|---|
| Active ingredient | Levonorgestrel 1.5mg | Ulipristal acetate 30mg | Levonorgestrel 1.5mg | Copper (Cu‑T) wire | Ethinylestradiol + levonorgestrel |
| Effective window | Up to 72h (best <24h) | Up to 120h (maintains >90% efficacy) | Up to 72h | Up to 120h (acts as primary EC) | Up to 72h (requires two doses) |
| Prescription needed | No (OTC) | Yes (GP or pharmacist) | No (OTC) | Yes (GP referral) | Yes (prescribed) |
| Cost (UK, 2025) | £0 (NHS for under‑25) or £10‑£15 privately | ~£30‑£35 (prescription) | £5‑£10 (generic) | ~£150‑£200 (including insertion) | £20‑£25 (two pills) |
| Common side‑effects | Nausea, fatigue, headache | Delayed period, mild abdominal pain | Same as I‑Pill | Heavier menstrual bleeding, cramps | Nausea, breast tenderness, spotting |
| Long‑term contraception | No | No | No | Yes (up to 10years) | No |
Choosing the Right Option for You
Decision‑making usually comes down to three questions: how much time has passed, what side‑effects you can tolerate, and whether you want ongoing birth control.
- Time since intercourse. If you’re within 24hours, any levonorgestrel pill (I‑Pill or generic) works well. Beyond 72hours, ulipristal or a copper IUD become the only reliable choices.
- Health considerations. Women taking hormonal contraception already, or those on enzyme‑inducing medicines (e.g., some anti‑epileptics), may experience reduced levonorgestrel efficacy. Ulipristal is less affected by such interactions.
- Future contraception needs. If you’re looking for a one‑off fix, a pill is simplest. If you want a set‑and‑forget method, ask your GP about a copper IUD - it doubles as a regular contraceptive after the emergency window.
Remember that Emergency contraception is not an abortion method. It works before implantation; it will not end an established pregnancy.
How to Get It in the UK (2025)
The NHS provides levonorgestrel for free to anyone under 25 and for those who meet specific clinical criteria. Visit any community pharmacy; the staff can dispense the I‑Pill on the spot. For ulipristal (Ella), you’ll need a prescription, which most pharmacies can arrange after a brief tele‑consultation with a GP.
If you opt for the copper IUD, book an appointment with your GP or a sexual‑health clinic. Some clinics now offer same‑day insertion if you meet the timing window, but expect a short waiting period for a specialist appointment.
Private pharmacies and online tele‑health services also sell generic levonorgestrel and ulipristal, usually with delivery within 24hours. Prices vary, so compare before buying.

Common Myths and Reality Checks
Myth 1: “The I‑Pill can cause a miscarriage.”
Reality: It prevents fertilisation; it has no effect on an already implanted embryo.
Myth 2: “If I vomit after taking the pill, it won’t work.”
Reality: Vomiting within two hours may reduce absorption. In that case, take a second dose and consider a backup method.
Myth 3: “I need to use condoms after taking emergency contraception.”
Reality: EC does not protect against STIs. Use condoms if STI protection is needed.
Quick Reference Cheat‑Sheet
- I‑Pill (Levonorgestrel): OTC, 72h window, cheap/free for under‑25.
- Ella (Ulipristal): Prescription, 120h window, higher cost, slightly better efficacy after 48h.
- Generic Levonorgestrel: Same as I‑Pill, often cheaper, OTC.
- Copper IUD: Clinician‑inserted, 120h window, provides long‑term contraception.
- Yuzpe regimen: Requires two doses, less effective than pills, useful if no dedicated EC pill available.
Frequently Asked Questions
How soon after sex should I take the I‑Pill?
The sooner the better. Effectiveness is about 95% within 24hours and falls to roughly 58% by the end of the 72‑hour window.
Can I take both levonorgestrel and ulipristal together?
No. Ulipristal works best on its own; taking levonorgestrel after ulipristal can reduce the latter’s effectiveness.
Is a copper IUD safe for teenagers?
Yes, when inserted by a trained clinician and after discussing menstrual changes. Many clinics offer it to teens who need reliable long‑term contraception.
What should I do if I experience severe nausea after a pill?
Take an anti‑emetic like ondansetron if needed, and stay hydrated. If vomiting occurs within two hours of taking the pill, repeat the dose with a new tablet.
Can I use emergency contraception while on the birth control pill?
Yes. The emergency pill is an additional safety net and does not interfere with your regular hormonal regimen.








Comments (11)
Brandon Leach
October 10, 2025 AT 16:18 PMOh joy another pill selector, because picking a birth control is my favorite hobby.
Alison Poteracke
October 11, 2025 AT 14:31 PMIt's good to have a tool that shows the options, especially when you need a quick decision after a mistake.
Marianne Wilson
October 12, 2025 AT 12:44 PMWhile the interface appears user‑friendly, it dangerously oversimplifies a serious medical decision, ignoring the nuanced contraindications of levonorgestrel versus ulipristal acetate and the ethical implications of promoting over‑the‑counter access without proper counseling.
Patricia Bokern
October 13, 2025 AT 10:58 AMCan you believe they're trying to push a pill on us like it's candy?
They don't want us to ask questions, they just want us to swallow whatever they feed us!
Garrett Gonzales
October 14, 2025 AT 09:11 AMThe emergency contraceptive landscape is dominated by two pharmacological agents: levonorgestrel (the I‑Pill) and ulipristal acetate (Ella).
Levonorgestrel exerts its effect primarily by inhibiting ovulation when administered within 72 hours of unprotected intercourse.
Ulipristal, a selective progesterone receptor modulator, maintains efficacy up to 120 hours and displays a higher binding affinity for the progesterone receptor.
Pharmacokinetic profiles differ, with levonorgestrel reaching peak plasma concentrations within 2‑3 hours, whereas ulipristal peaks slightly later but sustains therapeutic levels longer.
The safety margin for levonorgestrel is well‑established, with common side effects including nausea, headache, and mild abdominal cramping.
Ulipristal tends to have a more favorable side‑effect profile regarding nausea but can cause menstrual irregularities that may be misinterpreted as pregnancy.
Cost considerations are significant; levonorgestrel is often available for free on the NHS for those under 25, while ulipristal typically incurs a charge.
Drug interactions are also a factor: enzyme‑inducing agents such as rifampicin can reduce levonorgestrel efficacy, whereas ulipristal is less susceptible to such interactions.
In terms of contraindications, both agents share similar warnings regarding known hypersensitivity and active pregnancy, but ulipristal is contraindicated in patients with severe liver disease.
Clinical guidelines recommend levonorgestrel as first‑line for most patients due to its accessibility and proven track record.
However, for individuals presenting beyond the 72‑hour window or with a high body mass index, ulipristal may offer superior efficacy.
Patient counseling should emphasize the importance of timely administration, regardless of the chosen agent.
Moreover, healthcare providers must discuss the lack of long‑term contraceptive protection from either pill, encouraging follow‑up for ongoing birth control needs.
Finally, the decision matrix should incorporate patient preferences, side‑effect tolerance, and financial constraints to personalize therapy.
By integrating these pharmacological nuances, clinicians can optimize emergency contraception outcomes while respecting patient autonomy.
Aman Deep
October 15, 2025 AT 07:24 AMWow 🌈 this tool is like a rainbow of choices 🎨 it makes the whole pill thing feel less scary and more like an adventure 😅
Herman Bambang Suherman
October 16, 2025 AT 05:38 AMThe comparison is clear and helps decide quickly.
Meredith Blazevich
October 17, 2025 AT 03:51 AMI totally get how overwhelming it can feel when you’re scrambling for answers, especially after a night that didn’t go as planned.
Seeing the side‑effect tolerances and cost breakdown side by side really takes some of the anxiety out of the equation.
Just remember that none of these options replace regular contraception, they’re a safety net, not a primary plan.
If you’re under 25 the NHS hook‑up is a lifesaver, and if you’re over, budgeting becomes part of the decision.
Take a breath, trust the science, and pick the one that fits your body and wallet.
Nicola Gilmour
October 18, 2025 AT 02:04 AMGreat job pulling together the data – this makes it way easier for anyone who’s on the fence.
Darci Gonzalez
October 19, 2025 AT 00:18 AMLove the clear layout 😊 it gives you the info you need without the jargon, so you can act fast and feel confident about your choice.
Marcus Edström
October 19, 2025 AT 22:31 PMOverall the selector is a solid step forward, but remember to follow up with a healthcare professional for ongoing contraception needs.